Type 2 diabetes insulin decision guide: navigating the complexities of insulin therapy for managing blood sugar levels. This guide offers a comprehensive approach, taking you through the essential factors, considerations, and strategies for choosing the right insulin regimen. From understanding the different types of insulin to assessing your individual needs, we’ll explore the entire process, empowering you to make informed decisions with your healthcare team.
This guide delves into the multifaceted world of insulin therapy for type 2 diabetes, providing a personalized approach. We’ll cover everything from understanding the basics of insulin to evaluating your specific needs and preferences. The information is designed to help you feel more confident and empowered in managing your condition.
Introduction to Type 2 Diabetes Insulin Decision-Making
Type 2 diabetes is a chronic condition characterized by elevated blood sugar levels, impacting how the body uses insulin. Effectively managing blood sugar is crucial to prevent long-term complications such as heart disease, nerve damage, and kidney problems. Treatment strategies for type 2 diabetes often start with lifestyle modifications like diet and exercise, but sometimes, insulin therapy becomes necessary.Insulin therapy plays a vital role in managing type 2 diabetes when lifestyle changes are insufficient to control blood sugar.
It works by replacing or supplementing the body’s natural insulin production, allowing glucose to be transported into cells for energy. However, choosing the right type of insulin is a personalized decision, depending on various factors. This guide will explore the factors involved in determining the most appropriate insulin therapy for each individual.
Factors Influencing Insulin Therapy Decisions
Several factors significantly influence the decision to initiate or adjust insulin therapy in type 2 diabetes. These factors include the individual’s blood glucose levels, overall health status, lifestyle, and treatment goals. A thorough assessment by a healthcare professional is essential to determine the most effective approach. Individualized treatment plans are vital to optimize outcomes and patient well-being.
Types of Insulin Available
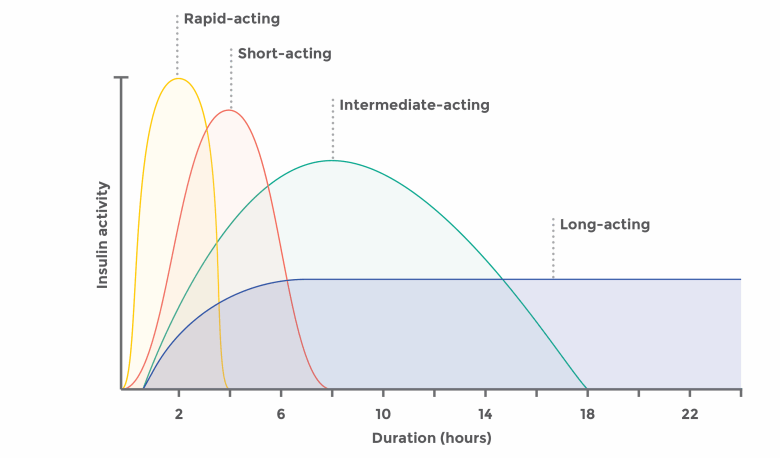
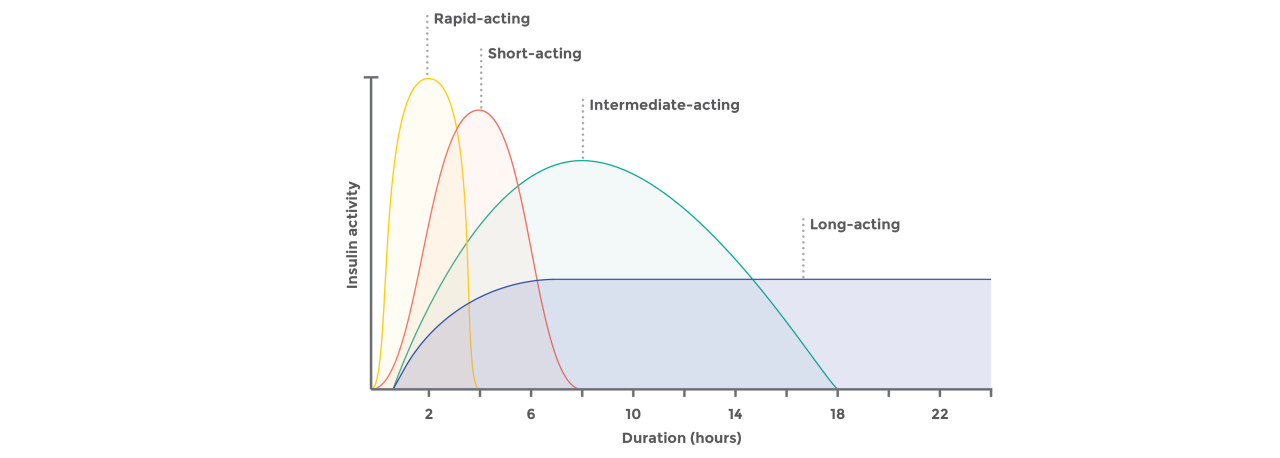
Different types of insulin vary in their onset, peak, and duration of action. Understanding these characteristics is crucial for tailoring the insulin regimen to the individual’s needs.
| Insulin Type | Onset (hours) | Peak (hours) | Duration (hours) | Typical Usage |
|---|---|---|---|---|
| Rapid-acting insulin (e.g., lispro, aspart, glulisine) | 15-30 minutes | 1-2 hours | 3-5 hours | Taken immediately before meals to manage postprandial (after-meal) blood glucose spikes. |
| Short-acting insulin (e.g., regular insulin) | 30 minutes – 1 hour | 2-3 hours | 5-8 hours | Often used in combination with other types of insulin or as a supplemental dose. It is also administered intravenously in hospital settings for critical situations. |
| Intermediate-acting insulin (e.g., NPH insulin) | 2-4 hours | 4-12 hours | 18-24 hours | Used to provide a basal (background) level of insulin throughout the day. |
| Long-acting insulin (e.g., detemir, glargine) | 1-2 hours | No pronounced peak | 20-24 hours | Administered once daily to provide a steady release of insulin throughout the day and night. Often used as a basal insulin. |
Choosing the right insulin type depends on factors like meal timing, blood glucose levels, and individual responses. The dosage and frequency of insulin injections will also vary based on the type of insulin chosen and the individual’s specific needs. This information should be carefully considered and discussed with a healthcare professional.
Thinking about a type 2 diabetes insulin decision guide? It’s a big decision, and navigating the options can be overwhelming. Recently, the FDA approved a new injectable drug regimen for people with HIV, highlighting the innovative strides in treatment for various chronic conditions. While the HIV treatment is interesting, a type 2 diabetes insulin decision guide still requires careful consideration of individual needs and blood sugar control goals.
Personalized Approaches to Insulin Treatment
Tailoring insulin therapy to each individual is crucial for achieving optimal blood glucose control and minimizing adverse effects. A personalized approach involves considering individual factors, lifestyle, and health goals. This may involve a combination of different insulin types and strategies to find the most effective regimen. Continuous glucose monitoring (CGM) can be valuable in adjusting insulin doses based on real-time blood glucose readings, allowing for more precise management.
Factors Influencing Insulin Decisions
Choosing the right insulin regimen for type 2 diabetes is a personalized journey, and several factors play crucial roles in making the best decision for each individual. These factors, which are intertwined and should be considered holistically, encompass patient characteristics, blood glucose control, treatment goals, delivery methods, and potential risks. Understanding these aspects allows healthcare providers to tailor a plan that promotes optimal blood sugar management while minimizing adverse effects.A thorough evaluation of these factors ensures the insulin regimen aligns with the patient’s unique needs and preferences, ultimately improving their overall health and quality of life.
Patient Characteristics Impacting Insulin Choices
Individual differences significantly impact insulin selection. Age, lifestyle, and pre-existing conditions (comorbidities) all influence the appropriate approach. Younger patients with active lifestyles might require different strategies compared to older individuals with more sedentary habits or other health concerns. Consideration of these factors helps tailor the insulin regimen to the specific circumstances of each patient.
- Age: Older adults may have different metabolic responses to insulin compared to younger patients, and their overall health status might require a more gradual approach to insulin initiation.
- Lifestyle: Individuals with active lifestyles and consistent exercise routines may require different insulin dosing adjustments compared to those with less active lifestyles. Consistent meal timing and portion control are essential for effective blood glucose management.
- Comorbidities: The presence of other medical conditions, such as kidney disease, heart disease, or liver disease, significantly impacts insulin selection and dosing. These conditions can affect how the body processes insulin and requires careful consideration in treatment planning.
Role of A1C Levels and Other Blood Glucose Metrics
Monitoring blood glucose levels and A1C (hemoglobin A1c) is crucial for determining the appropriate insulin strategy. A1C reflects average blood glucose levels over several months, providing a comprehensive picture of long-term glycemic control. Other metrics, such as fasting blood glucose and postprandial glucose (blood sugar after meals), offer insights into short-term glucose fluctuations.
- A1C Levels: High A1C levels often indicate the need for insulin therapy. The target A1C level for most individuals is below 7%, although this target may be adjusted based on individual circumstances and risk factors.
- Fasting Blood Glucose: Elevated fasting blood glucose levels can signal a need for adjustments in basal insulin, which controls blood sugar between meals.
- Postprandial Glucose: High postprandial glucose levels may necessitate adjustments to mealtime insulin doses to manage blood sugar spikes after meals.
Significance of Patient Preferences and Goals
Patient preferences and treatment goals significantly impact the selection of an insulin regimen. Understanding the patient’s lifestyle, preferences for injections or pumps, and willingness to engage in self-management are key considerations. Patient education and active participation in the treatment plan are essential for success.
- Patient Preferences: Some patients prefer the convenience of insulin pumps, while others may find injections more manageable. Tailoring the delivery method to the patient’s preference can improve adherence and engagement with the treatment plan.
- Treatment Goals: Patient goals regarding their health, lifestyle, and treatment preferences play a vital role in selecting the right insulin regimen. These goals might include achieving and maintaining a specific A1C level, improving overall well-being, and avoiding potential side effects.
Comparison of Insulin Delivery Methods
Different insulin delivery methods offer varying degrees of convenience and flexibility. Injections, either with syringes or pens, remain a common approach. Insulin pumps offer continuous insulin delivery, potentially providing more precise glucose control.
- Injections: Injections, using syringes or insulin pens, are a widely accessible and relatively inexpensive method. They provide flexibility and control, but require regular self-administration.
- Insulin Pumps: Insulin pumps deliver insulin continuously, mimicking the natural release of insulin from the pancreas. They offer more precise glucose control, but require more technical knowledge and potentially greater cost.
Importance of Considering Potential Side Effects and Risks
Insulin therapy, while essential for many individuals with type 2 diabetes, carries potential side effects and risks. Hypoglycemia (low blood sugar) is a common concern and requires careful monitoring and management. Weight gain and other side effects may also occur.
- Hypoglycemia: A significant risk associated with insulin therapy is hypoglycemia, which can lead to various symptoms and complications. Patients should be educated on recognizing and managing hypoglycemia.
- Weight Gain: Insulin therapy can sometimes lead to weight gain, which is an important factor to discuss with the patient and consider in the treatment plan.
- Other Side Effects: Other potential side effects of insulin therapy include allergic reactions, lipodystrophy (changes in fat tissue), and infection at injection sites.
Summary of Insulin Regimens
| Insulin Regimen | Pros | Cons |
|---|---|---|
| Basal-bolus | Highly customizable, often achieving tight glucose control | Complex, requiring multiple daily injections or pump use |
| Premixed Insulin | Convenient, requiring fewer injections | Less flexible, may not achieve optimal glucose control in all cases |
| Combination Injections | Convenient, combining basal and bolus insulin in one injection | May not be optimal for individuals with fluctuating glucose levels |
Assessing Patient Needs for Insulin
Choosing the right insulin regimen for a patient with type 2 diabetes is a deeply personal journey. It’s not a one-size-fits-all approach. Successful management hinges on a thorough understanding of the patient’s individual needs, lifestyle, and preferences. This section delves into the crucial steps of assessing patient needs to tailor an effective insulin strategy.A patient’s ability to successfully manage insulin therapy is directly correlated with their understanding of the condition and the treatment plan.
Factors such as lifestyle, support systems, and emotional well-being all play critical roles in a patient’s success. This personalized approach ensures that the chosen insulin regimen aligns with their unique circumstances and fosters adherence to the treatment plan.
Understanding of Type 2 Diabetes and Insulin
A patient’s knowledge about type 2 diabetes and insulin is fundamental to their ability to effectively manage the condition. Assessing this understanding involves gauging their comprehension of blood glucose levels, the role of insulin in regulating these levels, and the potential side effects of different insulin types.
- Patients should possess a clear understanding of the role of insulin in managing blood sugar levels, and how their daily activities affect these levels.
- Knowledge of different types of insulin (e.g., rapid-acting, long-acting), their respective durations, and when to administer them is crucial for proper self-management.
- Patients should be aware of the potential side effects of insulin, including hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar), and how to recognize and manage these symptoms.
- A patient’s familiarity with monitoring blood glucose levels, understanding the importance of regular testing, and recognizing patterns in their results is key to insulin management.
Evaluating Ability to Manage Insulin Therapy
Assessing a patient’s ability to manage insulin therapy requires a multifaceted approach. This includes evaluating their practical skills, emotional preparedness, and support systems.
- Practical skills, such as accurate insulin injection technique, proper blood glucose monitoring, and understanding the importance of a healthy diet and exercise, are critical to effective insulin management.
- The patient’s emotional preparedness and motivation to adhere to the treatment plan should be assessed. Factors like stress, anxiety, and depression can significantly impact adherence.
- Support systems, including family members, friends, or support groups, can play a crucial role in providing encouragement and assistance.
- The patient’s ability to access resources, such as healthcare providers, educational materials, and supplies, also influences their ability to manage insulin.
Considering Patient Lifestyle Factors and Preferences
Tailoring an insulin regimen to a patient’s lifestyle is essential for long-term adherence. This includes understanding their daily routines, dietary habits, and physical activity levels.
- Lifestyle factors, including work schedule, meal patterns, and physical activity levels, should be considered to design an insulin regimen that aligns with their daily routine.
- Patient preferences for different insulin types, administration methods (e.g., injections, pumps), and frequency of monitoring should be factored into the decision-making process.
- Incorporating the patient’s cultural and socioeconomic background is important in understanding their access to resources and support systems.
Patient-Centered Questions for a Diabetes Consultation
Patient-centered questions are crucial for eliciting information about the patient’s individual needs and preferences. These questions should be open-ended and encourage the patient to share their experiences and perspectives.
- Open-ended questions, such as “Can you describe your typical daily routine?” or “What are your concerns about managing your diabetes?”, allow the patient to elaborate on their experiences.
- Questions that assess the patient’s understanding of their condition, like “How do you feel your current knowledge helps you manage your diabetes?”, promote a deeper understanding of the patient’s perspective.
Key Questions about Medical History and Lifestyle
A structured approach to gather information helps ensure comprehensive patient assessment. The table below Artikels key questions for gathering information about medical history and lifestyle.
| Category | Questions |
|---|---|
| Medical History | Previous diagnoses, hospitalizations, allergies, and family history of diabetes. |
| Lifestyle Factors | Dietary habits, physical activity levels, sleep patterns, and stress levels. |
| Support Systems | Availability of support from family, friends, or healthcare professionals. |
| Personal Preferences | Preferred insulin administration method, frequency of blood glucose monitoring, and desired level of involvement in decision-making. |
Strategies for Insulin Initiation and Adjustment
Initiating and adjusting insulin therapy for type 2 diabetes requires careful consideration of individual patient needs and responses. A personalized approach, guided by ongoing monitoring and education, is crucial for achieving optimal glycemic control and minimizing complications. This section will Artikel strategies for initiating insulin and adjusting dosages, emphasizing the importance of patient education.
Insulin Initiation Strategies
Insulin initiation in type 2 diabetes often begins with a basal insulin regimen, focusing on providing a constant level of insulin throughout the day to control fasting glucose levels. This approach is frequently chosen because it’s less complex than bolus insulin, which requires more frequent dosing adjustments. The specific type of basal insulin (e.g., long-acting analogs like glargine or detemir) and initial dose will vary based on the patient’s individual characteristics and baseline blood glucose control.
Navigating type 2 diabetes insulin decision guides can feel overwhelming, but it’s crucial for managing blood sugar levels effectively. Choosing the right sound machine for baby, like the one recommended on this helpful resource, best sound machine for baby , can also be a significant factor in creating a peaceful sleep environment. Ultimately, a well-informed approach to both sleep and diabetes management is key for overall well-being.
Clinical guidelines and the patient’s response to the therapy will influence subsequent adjustments.
Insulin Dose Adjustment Process
Adjusting insulin doses involves a systematic approach based on frequent monitoring of blood glucose levels. This monitoring typically includes both fasting and postprandial (after meals) glucose readings. The goal is to achieve target blood glucose levels while minimizing hypoglycemia (low blood sugar). The process is iterative, requiring ongoing evaluation and adaptation of the insulin regimen.
Importance of Patient Education
Patient education plays a critical role in successful insulin management. Empowering patients with knowledge about insulin administration, glucose monitoring techniques, and recognizing hypoglycemic symptoms is vital for long-term adherence and optimal outcomes. This includes understanding how food choices, physical activity, and stress can affect blood sugar levels, enabling proactive management.
Steps for Effective Insulin Dose Adjustments
A structured approach to insulin dose adjustments is essential for achieving optimal glycemic control. The following steps provide a framework for this process:
- Baseline Assessment: Determine the patient’s current blood glucose levels, including fasting and postprandial readings, and identify any pre-existing health conditions or medications.
- Initial Insulin Dosage: Begin with a basal insulin dose based on clinical guidelines and the patient’s characteristics. Consider factors like age, weight, and current medication use.
- Regular Monitoring: Monitor blood glucose levels regularly, typically daily or more frequently, depending on the patient’s needs and the insulin regimen.
- Dose Adjustments: Adjust the insulin dose based on the monitoring results. Small, incremental adjustments are generally recommended to avoid significant fluctuations in blood sugar.
- Dietary and Lifestyle Modifications: Encourage healthy dietary choices and regular physical activity to complement insulin therapy and improve overall metabolic health.
- Regular Follow-up: Schedule regular follow-up appointments with the healthcare provider to assess progress, adjust the treatment plan, and address any concerns.
Common Insulin Initiation Protocols
Different healthcare settings and providers may use various protocols for initiating insulin therapy. Here’s a table outlining some common approaches:
| Protocol | Insulin Type | Initial Dose | Monitoring Frequency | Adjustment Criteria |
|---|---|---|---|---|
| Protocol A | Glargine | 10 units daily | Daily fasting glucose | Increase dose by 2 units every 2-3 days if fasting glucose remains above target |
| Protocol B | Detemir | 0.2 units/kg/day | Daily fasting and postprandial glucose | Adjust basal dose based on fasting glucose; bolus insulin added for meals if postprandial glucose remains elevated |
| Protocol C | NPH | 10-15 units daily | Daily fasting and pre-meal glucose | Increase dose by 2-4 units based on fasting and pre-meal glucose, considering meal size and activity |
Long-Term Management and Monitoring
Insulin therapy for type 2 diabetes isn’t a one-and-done deal. It’s a dynamic process requiring ongoing monitoring and adjustments to maintain optimal blood sugar levels and overall health. This phase emphasizes the importance of long-term commitment and collaboration between the patient and healthcare team.Successful long-term management hinges on proactive engagement and understanding of how lifestyle choices, stress levels, and other factors impact blood glucose control.
This ongoing monitoring allows for adjustments to the insulin regimen, ensuring the most effective and personalized approach to diabetes care.
Importance of Ongoing Monitoring and Adjustments
Regular monitoring is crucial to detect any changes in blood sugar control and adjust insulin doses accordingly. This proactive approach allows for timely intervention to prevent complications. For instance, a patient experiencing increased blood sugar levels might need a higher insulin dose, while someone whose levels remain consistently low may require a dose reduction. These adjustments ensure blood glucose levels remain within a target range, minimizing the risk of serious health problems.
Role of Regular Follow-Up Appointments
Regular follow-up appointments with a healthcare professional are essential components of a diabetes management plan. These appointments provide opportunities to discuss any concerns, review blood test results, and adjust the insulin regimen as needed. The doctor can assess how the patient is responding to treatment, and make necessary changes to maintain optimal blood glucose levels. These interactions allow for personalized adjustments, ensuring the therapy aligns with the patient’s specific needs and lifestyle.
Figuring out the best insulin for type 2 diabetes can be tricky, and a decision guide can be really helpful. Sometimes, similar symptoms can make diagnoses challenging, like when endometriosis symptoms mimic appendicitis, as seen in this insightful article about endometriosis mistaken for appendicitis. Ultimately, a proper diagnosis and personalized insulin regimen are crucial for effective management of type 2 diabetes.
A consistent dialogue between the patient and healthcare team is vital for achieving long-term success.
Importance of Patient Self-Management Skills and Support
Effective self-management is paramount for successful long-term insulin therapy. This involves regular blood glucose monitoring, understanding insulin action, and recognizing patterns in blood sugar fluctuations. Patients should be empowered to take an active role in their care, recognizing the connection between lifestyle choices and blood sugar levels. Support from healthcare providers, family members, and support groups can be invaluable in fostering self-management skills and adherence to the treatment plan.
This holistic approach promotes a stronger sense of control and empowers patients to proactively manage their condition.
Components of a Comprehensive Diabetes Management Plan
A well-structured diabetes management plan encompasses various elements crucial for successful long-term control. These elements work together to optimize blood sugar levels, promote overall well-being, and minimize the risk of complications.
| Component | Description |
|---|---|
| Blood Glucose Monitoring | Regular monitoring using a glucometer to track blood sugar levels throughout the day, allowing for identification of patterns and trends. |
| Insulin Administration | Precise and consistent administration of insulin according to the prescribed regimen. This includes understanding the different types of insulin, their durations of action, and proper injection techniques. |
| Dietary Management | Following a balanced and healthy diet tailored to individual needs, considering carbohydrate counting and portion control to regulate blood sugar levels. |
| Physical Activity | Regular exercise to improve insulin sensitivity and aid in blood sugar control. This should be tailored to the individual’s capabilities and preferences. |
| Stress Management | Developing strategies to manage stress, as stress can impact blood sugar levels. This may include relaxation techniques, mindfulness, or counseling. |
| Regular Medical Checkups | Scheduled appointments with healthcare professionals for monitoring, reviewing blood test results, and adjusting the treatment plan. |
| Patient Education and Support | Receiving education on diabetes management, including insulin therapy, healthy lifestyle choices, and available support resources. This also includes understanding potential complications and preventative measures. |
Illustrative Case Studies
Understanding how insulin therapy works in real-world scenarios is crucial for effective diabetes management. These case studies highlight the decision-making process, factors considered, and monitoring strategies involved in initiating and adjusting insulin regimens for individuals with type 2 diabetes.
Case Study 1: Mr. Smith
Mr. Smith, a 55-year-old male with a history of type 2 diabetes for 10 years, presents with elevated HbA1c levels (9.5%) despite oral medication. He reports experiencing frequent episodes of hyperglycemia, particularly after meals. He is overweight (BMI 30) and leads a sedentary lifestyle. He expresses concerns about potential side effects and the complexity of managing insulin.
Factors Influencing Insulin Decisions
Several factors were considered when developing Mr. Smith’s insulin treatment plan:
- His current HbA1c level (9.5%) and history of elevated blood glucose levels indicated a need for insulin to achieve optimal glycemic control.
- His relatively recent diagnosis of type 2 diabetes (10 years) suggests that his beta-cell function may be partially preserved, potentially making a basal-bolus approach a suitable option.
- His lifestyle factors, including sedentary habits and weight, contributed to his current glycemic status and were acknowledged as areas needing improvement.
- His concerns about potential side effects and complexity of insulin management were addressed by providing clear and concise information, and offering support.
Insulin Regimen Chosen
A basal-bolus insulin regimen was chosen for Mr. Smith. This approach involves a long-acting insulin (e.g., glargine) administered once daily to maintain basal glucose control and rapid-acting insulin (e.g., lispro) administered before meals to manage postprandial glucose surges. The dosage was carefully titrated based on his individual needs and response.
Monitoring Patient Response
Mr. Smith’s response to treatment was monitored through regular blood glucose monitoring (at least 4 times daily) and HbA1c checks every 3 months. This allowed for adjustments to his insulin dosage as needed. His weight was also monitored, and lifestyle modifications were encouraged to further improve glycemic control.
Key Steps in Managing Mr. Smith’s Case
| Step | Action |
|---|---|
| 1 | Initiate basal-bolus insulin regimen with long-acting and rapid-acting insulin. |
| 2 | Educate Mr. Smith on proper insulin injection techniques and the importance of adherence to the regimen. |
| 3 | Monitor blood glucose levels regularly (at least 4 times daily) and adjust insulin doses as needed based on the results. |
| 4 | Schedule follow-up appointments every 3 months to assess HbA1c levels and overall glycemic control. |
| 5 | Encourage lifestyle modifications (diet and exercise) to improve glycemic control and overall health. |
Resources and Support Systems: Type 2 Diabetes Insulin Decision Guide
Navigating type 2 diabetes, especially when insulin is introduced, can feel overwhelming. Fortunately, a robust network of support and resources is available to help you every step of the way. This section explores the vital tools and organizations that can empower you with knowledge, community, and practical strategies for managing your condition effectively.
Reputable Organizations Offering Support and Education
Numerous organizations provide invaluable support and educational materials for individuals with type 2 diabetes. These organizations often offer online resources, workshops, and support groups, tailored to meet diverse needs. They play a crucial role in fostering a sense of community and shared experience.
- The American Diabetes Association (ADA): A leading voice in diabetes research and advocacy, the ADA offers comprehensive information, resources, and tools for individuals with type 2 diabetes. Their website features articles, videos, and educational materials on insulin management, alongside access to support groups and local chapters.
- The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): A part of the National Institutes of Health, the NIDDK provides evidence-based information and research on diabetes, including insulin therapy. Their website offers a wealth of resources on various aspects of diabetes management, including treatment options and potential complications.
- The Juvenile Diabetes Research Foundation (JDRF): While primarily focused on type 1 diabetes, JDRF also offers valuable information and support for individuals with type 2 diabetes. They often host online forums and provide access to a network of support and educational resources.
Online Resources and Tools for Insulin Management
Numerous online resources and tools can significantly aid in the management of insulin therapy. These tools often offer personalized insights and practical guidance.
- Diabetes management apps: Several apps provide detailed tracking of blood glucose levels, insulin doses, and other relevant data. These tools can help users monitor trends, identify patterns, and communicate effectively with healthcare providers. Examples include SugarWise, and others that offer features like reminders, meal planning, and educational content.
- Online calculators: Various online calculators can help estimate carbohydrate counts, insulin doses, and other factors. While these tools can be helpful, they should be used as a supplement to professional medical advice, not a replacement.
Finding Local Support Groups for Patients, Type 2 diabetes insulin decision guide
Connecting with other individuals facing similar challenges can provide invaluable support and encouragement. Local support groups offer a platform for sharing experiences, exchanging tips, and building a sense of community.
- Local chapters of diabetes organizations: Contacting local chapters of the ADA, or other relevant organizations, can lead to information about support groups in your area.
- Community centers and healthcare facilities: Local community centers and healthcare facilities often host support groups for various health conditions, including diabetes. Inquire with your local diabetes educator or doctor.
Useful Websites, Apps, and Support Groups
The following table provides a summary of reputable websites, apps, and support groups that can assist individuals managing type 2 diabetes, including insulin use.
| Resource | Description | Website/App |
|---|---|---|
| American Diabetes Association | Comprehensive resources, including support groups and educational materials. | diabetes.org |
| National Institute of Diabetes and Digestive and Kidney Diseases | Evidence-based information on diabetes, including insulin therapy. | niddk.nih.gov |
| SugarWise | Diabetes management app for tracking glucose levels, insulin doses, and other data. | (Example App Store link) |
| MySugr | Diabetes management app with features for blood glucose tracking, medication management, and reminders. | (Example App Store link) |
Conclusion
In conclusion, this type 2 diabetes insulin decision guide offers a practical framework for navigating insulin therapy. By understanding the factors influencing your choices, assessing your needs, and learning about initiation and long-term management strategies, you can work collaboratively with your healthcare team to develop a personalized plan. Remember, ongoing monitoring and support are crucial for success. This guide is intended to be a resource, not a replacement for professional medical advice.
Consult your doctor for personalized recommendations.