Upper GI and small bowel series offer a detailed look into the upper gastrointestinal tract and small intestines. This in-depth exploration delves into the procedures, from preparation to interpretation, providing a comprehensive understanding of their purpose, techniques, and significance in diagnosing and managing various gastrointestinal conditions. We’ll cover everything from the initial imaging process to post-procedure care, highlighting the crucial role these examinations play in modern medicine.
Understanding the intricacies of these procedures is vital for patients and healthcare professionals alike. This guide will simplify the complexities, making the process accessible and informative. The procedure’s steps, imaging techniques, and the crucial role of contrast agents will be explored in detail. Different types of contrast agents will be compared and contrasted. We’ll also discuss the significance of interpreting the findings, examining potential abnormalities, and their implications in clinical practice.
Introduction to Upper GI and Small Bowel Series
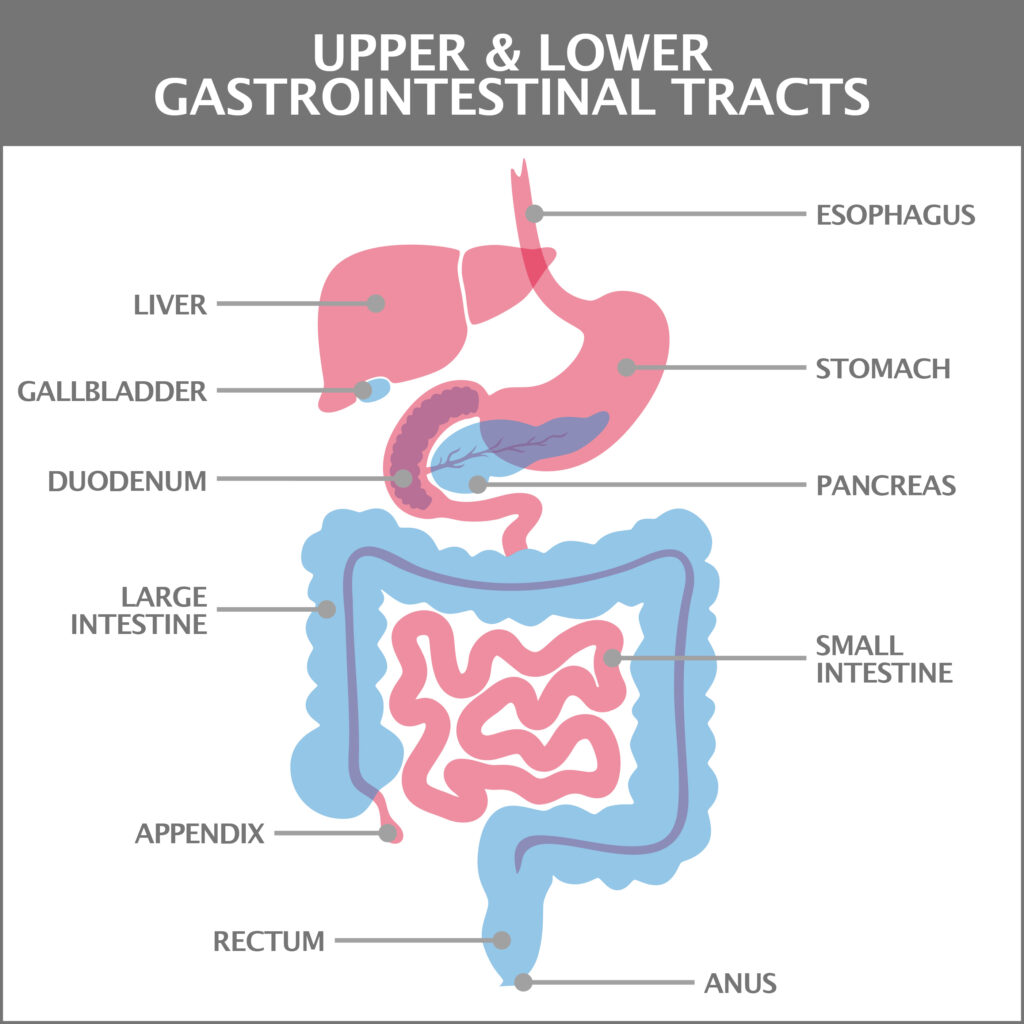
Upper GI and small bowel series are specialized X-ray procedures that provide detailed images of the upper digestive tract, from the esophagus to the small intestine. These non-invasive examinations are crucial for diagnosing a wide range of digestive issues, from ulcers and tumors to obstructions and inflammatory conditions. Understanding the process, preparation, and purpose of these examinations is vital for both patients and healthcare professionals.
Procedure Definition
Upper GI and small bowel series are radiographic examinations that visualize the upper gastrointestinal (GI) tract and small bowel, respectively. An upper GI series, also known as a barium swallow, involves the ingestion of a barium contrast material that coats the lining of the esophagus, stomach, and duodenum. The small bowel series, in contrast, uses a similar contrast material and specialized techniques to visualize the small intestine.
Both procedures utilize X-rays to capture the images, which are then interpreted by a radiologist.
Purpose of the Examinations
These procedures are employed to identify various abnormalities within the upper GI and small bowel. They help detect ulcers, tumors, strictures, obstructions, inflammatory conditions, and other structural or functional issues. By visualizing the organs and their contents, radiologists can pinpoint the location and nature of the problem. This aids in the formulation of a precise diagnosis and guides further management strategies.
Patient Preparation
Proper patient preparation is essential for obtaining high-quality images and accurate diagnostic results. Patients are typically asked to fast for a specific period before the examination, often 8 to 12 hours, to ensure the stomach and small intestine are empty. Clear liquids are often permitted a few hours prior. They are instructed to avoid any food or drink, and medications that could alter the results.
This preparation allows for a clear visualization of the structures being examined.
Equipment Used
The equipment used in these procedures typically includes a fluoroscopy machine, a barium contrast material, and various specialized accessories. The fluoroscopy machine uses X-rays to generate real-time images of the digestive tract, allowing for adjustments during the examination. The barium contrast material coats the lining of the organs, enhancing their visibility on the X-ray images. Specific accessories, such as tubes or catheters, may be employed depending on the specific requirements of the examination.
I recently had an upper GI and small bowel series, and it got me thinking about natural remedies. While I’m still waiting for the results, I’ve been researching natural solutions for skin conditions like eczema. Apparently, black seed oil for eczema is a popular topic, with many claiming it helps soothe irritated skin. black seed oil for eczema seems to be a promising area of research.
Hopefully, the upper GI and small bowel series results will give me more clarity on my overall health and allow me to explore more natural remedies in the future.
Summary Table
| Procedure Name | Purpose | Preparation | Equipment |
|---|---|---|---|
| Upper GI Series | Visualizes the esophagus, stomach, and duodenum to detect abnormalities like ulcers, tumors, or obstructions. | Fasting for 8-12 hours, clear liquids allowed hours before. | Fluoroscopy machine, barium contrast, specialized accessories. |
| Small Bowel Series | Visualizes the small intestine to identify issues such as Crohn’s disease, tumors, or obstructions. | Similar fasting protocol to Upper GI Series. | Fluoroscopy machine, barium contrast, specialized accessories. |
Imaging Techniques and Procedures: Upper Gi And Small Bowel Series
The upper GI and small bowel series are essential diagnostic tools for evaluating the structures of the upper digestive tract. These procedures utilize radiographic techniques to visualize the esophagus, stomach, duodenum, and small intestine, aiding in identifying abnormalities such as ulcers, tumors, strictures, and obstructions. Understanding the specific radiographic techniques and contrast agents employed is crucial for interpreting the resulting images and making accurate diagnoses.
Radiographic Techniques for Upper GI Series
The upper GI series, often referred to as a barium swallow, utilizes fluoroscopy to visualize the upper digestive tract. Fluoroscopy involves a continuous x-ray image of the area of interest. A radiopaque contrast agent, typically barium sulfate, is ingested by the patient, allowing the radiologist to observe the movement of the contrast medium through the esophagus, stomach, and duodenum.
This dynamic visualization helps identify structural abnormalities and motility issues. Key techniques include:
- Patient Positioning: The patient is positioned in various positions, such as supine and upright, to facilitate the visualization of different parts of the upper gastrointestinal tract and observe contrast passage.
- Imaging Timing: Fluoroscopy is performed at intervals during the procedure to capture images as the contrast agent moves through the digestive tract. This is particularly useful in identifying areas of delayed or abnormal transit.
- Specific Views: Different projections (views) of the esophagus, stomach, and duodenum are obtained to ensure a complete assessment of these organs. This allows the radiologist to evaluate the anatomy and structure from multiple angles.
Radiographic Techniques for Small Bowel Series
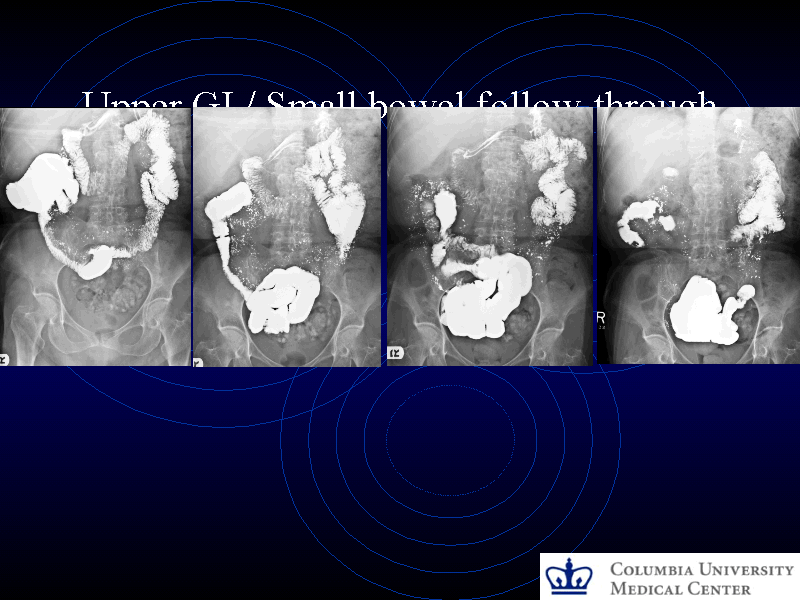
The small bowel series, also known as a small bowel follow-through, builds upon the principles of the upper GI series. Here, the contrast agent is typically allowed to pass through the stomach and into the small intestine. This allows for a more detailed visualization of the small bowel, which is longer and more complex than the upper GI structures.
The procedure involves:
- Oral Contrast Administration: A radiopaque contrast agent, usually barium sulfate, is given to the patient orally. The agent is swallowed and allowed to pass into the small intestine.
- Serial Imaging: Fluoroscopy is performed at regular intervals (often 15-30 minutes) to follow the contrast medium as it progresses through the small intestine. This continuous monitoring allows for the detection of any slow transit, blockage, or malabsorption issues.
- Specific Views: Multiple views of the small bowel are obtained to ensure a thorough examination. This may include positioning changes to visualize the different segments of the small bowel and to allow for an assessment of the bowel wall thickness and morphology.
Contrast Agents Used
Contrast agents are essential for visualizing the digestive tract structures. Barium sulfate is the most commonly used agent in both upper and small bowel series. It is a suspension of barium in water. Its radiopacity makes it readily visible on x-ray images.
Comparison of Contrast Agents
- Barium Sulfate: High density, widely available, and relatively inexpensive. It is non-absorbable and does not cause significant harm when ingested. A potential downside is that it can cause bowel discomfort or constipation in some individuals.
- Gastrografin: A water-soluble iodinated contrast agent. It is absorbed more rapidly than barium sulfate, which can be helpful in some instances. A potential downside is that it can cause a sensation of nausea or vomiting in some patients.
Comparison of Radiographic Techniques
| Characteristic | Upper GI Series | Small Bowel Series |
|---|---|---|
| Contrast Agent | Barium sulfate | Barium sulfate |
| Imaging Duration | Shorter, typically under 30 minutes | Longer, typically 1-2 hours |
| Purpose | Evaluate esophagus, stomach, and duodenum | Evaluate the small intestine |
| Contrast Administration | Direct ingestion of contrast agent | Ingestion of contrast agent, followed by serial imaging |
Indications and Contraindications
Upper GI and small bowel series are valuable diagnostic tools, providing crucial insights into the health of the upper digestive tract. These procedures can identify a wide range of abnormalities, from benign conditions to serious diseases. Understanding the indications, contraindications, and patient considerations is vital for clinicians to determine when these procedures are appropriate and to ensure patient safety.
Indications for Upper GI and Small Bowel Series
This procedure is used to visualize the upper gastrointestinal (GI) tract, including the esophagus, stomach, duodenum, and small intestine, to identify abnormalities. These abnormalities can include ulcers, tumors, strictures, or obstructions. The series can help determine the location, size, and extent of these problems, enabling more accurate diagnoses and tailored treatment plans.
- Suspected esophageal disorders: Conditions like esophageal strictures, webs, or tumors can cause dysphagia (difficulty swallowing). An upper GI series can visualize these structures and help determine the cause of the dysphagia.
- Gastric or duodenal ulcers: Upper GI series can reveal the presence and location of ulcers, providing crucial information for diagnosis and treatment. For example, a patient with chronic heartburn and upper abdominal pain might undergo this procedure to rule out ulcers.
- Small bowel obstructions: The series can identify obstructions in the small intestine, such as adhesions, tumors, or hernias, which can cause significant symptoms like abdominal pain, vomiting, and constipation. A patient with these symptoms and a history of abdominal surgery might be a candidate for this procedure.
- Suspected inflammatory bowel disease (IBD): In cases of suspected Crohn’s disease or ulcerative colitis, an upper GI and small bowel series can reveal characteristic findings such as inflammation, strictures, or fistulas. This is particularly helpful in assessing the extent and severity of the disease.
Contraindications for Upper GI and Small Bowel Series
Certain conditions and patient factors may make an upper GI and small bowel series unsuitable. It’s crucial to consider these factors to ensure patient safety and to select the most appropriate diagnostic approach.
- Recent or ongoing bowel perforation: This is a serious contraindication due to the risk of worsening the perforation and potentially causing further complications. Immediate surgical intervention may be required in these cases.
- Active bleeding: If a patient is actively bleeding, the procedure should be postponed until the bleeding is controlled. Active bleeding can increase the risk of complications during the procedure and subsequent interventions.
- Severe coagulopathy: Patients with significant blood clotting disorders are at increased risk of bleeding complications during or after the procedure. Careful consideration of the risks and benefits is necessary before proceeding with the examination.
- Pregnancy: While generally safe, the use of radiation during the procedure necessitates careful consideration. The benefits of the procedure must be weighed against the potential risks to the developing fetus.
Patient Considerations for Ordering the Procedure
Proper patient preparation and management are essential for obtaining accurate and safe results. These considerations must be thoroughly evaluated before scheduling the procedure.
- Patient history: A detailed medical history, including previous surgeries, diagnoses, and current medications, is crucial for evaluating potential risks and complications.
- Patient allergies: Allergies to contrast agents or other medications used in the procedure should be identified and documented.
- Patient’s ability to comply with preparation instructions: The patient’s ability to follow dietary restrictions and other pre-procedure instructions is important for ensuring the quality of the images.
- Patient’s overall health status: Patients with significant underlying medical conditions may require additional precautions and monitoring.
Table: Indications, Contraindications, and Patient Considerations
| Category | Description |
|---|---|
| Indications | Suspected esophageal disorders, gastric/duodenal ulcers, small bowel obstructions, suspected inflammatory bowel disease |
| Contraindications | Recent or ongoing bowel perforation, active bleeding, severe coagulopathy, pregnancy (consideration needed) |
| Patient Considerations | Patient history, allergies, ability to comply with preparation, overall health status |
Interpretation of Findings
Decoding the X-ray images from an upper GI and small bowel series provides valuable insights into the health of the digestive tract. These specialized radiographic examinations, often crucial in diagnosing various gastrointestinal conditions, require meticulous interpretation to identify subtle anomalies. A comprehensive understanding of the normal anatomy, coupled with the ability to recognize potential abnormalities, is essential for accurate diagnosis and subsequent patient management.The interpretation process involves carefully scrutinizing the images for any deviations from the expected anatomical structures.
This meticulous analysis can reveal a wide range of conditions, from benign to life-threatening. A trained radiologist, gastroenterologist, or other qualified medical professional is vital for accurately interpreting these complex images and translating them into actionable medical information.
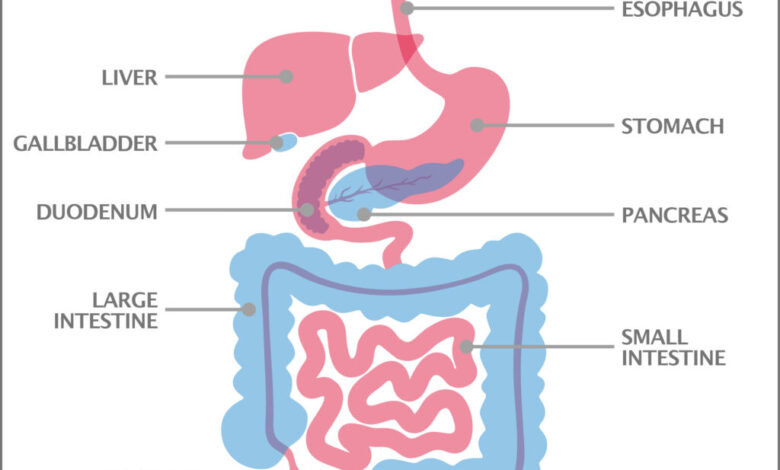
Typical Anatomical Structures Visualized in an Upper GI Series
The upper gastrointestinal (GI) series visualizes the esophagus, stomach, and duodenum. Barium contrast, swallowed by the patient, Artikels these structures, allowing for detailed visualization of their shape, size, and any irregularities. The esophagus, a muscular tube connecting the mouth to the stomach, is observed for its smooth, continuous passage. The stomach’s contour, the presence of any ulcers or tumors, and the pyloric sphincter’s function are key aspects to note.
Upper GI and small bowel series are crucial diagnostic tools, helping visualize the upper digestive tract. Thinking about diet, it’s interesting to consider how food choices can impact health. For instance, recent research suggests that consuming dairy products might actually help lower the risk of type 2 diabetes, while regularly eating processed meats could unfortunately raise it. This connection between diet and disease is something I’ve been researching lately, and I found some compelling insights on the subject in this article how dairy products can help lower type 2 diabetes risk while processed meats raise it.
Ultimately, understanding these potential dietary influences on health is vital to maintaining a holistic approach to care, even when dealing with procedures like an upper GI and small bowel series.
The duodenum, the first part of the small intestine, is also visualized for its normal shape and any abnormalities, such as strictures or tumors.
Typical Anatomical Structures Visualized in a Small Bowel Series
A small bowel series, often employing a similar barium contrast technique, allows for visualization of the jejunum and ileum. The small intestine is significantly longer than the stomach and duodenum, making it crucial to thoroughly assess the entire length. The series helps identify the normal folds, loops, and haustrations of the small intestine. Smooth, continuous filling and the expected pattern of folds and coils in the jejunum and ileum are critical to a normal finding.
Common Abnormalities in Upper GI and Small Bowel Series
Various abnormalities can be detected in upper GI and small bowel series. In an upper GI series, these might include esophageal varices, achalasia, gastric ulcers, tumors, or strictures. In a small bowel series, conditions like Crohn’s disease, celiac disease, and tumors or strictures are common findings. Obstructions, whether partial or complete, are significant indicators of potential issues.
Significance of Findings in Clinical Practice
Accurate interpretation of upper GI and small bowel series findings is paramount in patient care. These images can confirm suspected diagnoses, guide further investigations, and assist in planning treatment strategies. The results guide treatment decisions and determine the need for further diagnostic procedures. Early detection and intervention based on these findings can dramatically improve patient outcomes.
Table: Normal Anatomical Structures and Potential Abnormalities in an Upper GI Series
| Normal Anatomical Structure | Potential Abnormalities |
|---|---|
| Esophagus | Strictures, diverticula, esophageal varices, achalasia |
| Stomach | Ulcers, tumors, polyps, gastric folds, pyloric stenosis |
| Duodenum | Ulcers, tumors, strictures, duodenal diverticula |
Clinical Applications and Significance
Upper GI and small bowel series are invaluable tools in gastroenterology, providing critical insights into the health of the digestive tract. These imaging procedures offer a comprehensive view of the esophagus, stomach, small intestine, and proximal portion of the large intestine, enabling clinicians to visualize structural abnormalities and assess the function of these organs. Their diagnostic capabilities extend beyond mere visualization, encompassing the ability to evaluate the presence, extent, and potential causes of various gastrointestinal disorders.
Role in Diagnosing Gastrointestinal Disorders, Upper gi and small bowel series
Upper GI and small bowel series play a significant role in identifying a wide array of gastrointestinal disorders. These procedures are particularly useful in detecting structural abnormalities such as ulcers, strictures, tumors, and polyps. They can also reveal motility issues, such as those seen in conditions like Crohn’s disease or achalasia. The ability to visualize the entire digestive tract allows for a comprehensive assessment of the disease process.
Assessing Presence and Extent of Diseases
These procedures excel at not only detecting the presence of disease but also in determining its extent. For example, an upper GI series can pinpoint the precise location and length of a stricture, which is crucial information for planning surgical intervention or medical management. Likewise, the small bowel series can reveal the extent of inflammation or stricturing in the small intestine, providing vital information for treatment planning in conditions like Crohn’s disease.
This precise assessment allows for targeted interventions.
Importance in Treatment Planning
The information gathered from these procedures is instrumental in formulating treatment plans. Knowledge of the location, size, and nature of a lesion, obtained from the imaging studies, helps guide decisions regarding surgical resection, endoscopic procedures, or medical therapies. For example, a stricture visualized on an upper GI series may necessitate a dilation procedure, while a tumor identified on a small bowel series might require a biopsy or surgical intervention.
The imaging findings are pivotal in selecting the most appropriate treatment strategy.
Upper GI and small bowel series are crucial diagnostic tools, helping pinpoint issues within the upper digestive tract. While these procedures are vital for identifying potential problems, it’s also important to consider the broader context of healthcare choices, especially in the face of difficult diagnoses. For example, the debate around death with dignity laws in the Trump era death with dignity laws in trump era highlights the complex interplay between medical procedures and personal autonomy.
Ultimately, these tests are just one piece of the puzzle when it comes to comprehensive patient care.
Guiding Further Diagnostic Steps
The results of upper GI and small bowel series often serve as a springboard for further diagnostic investigations. For instance, if an abnormality is detected, additional tests like endoscopic procedures, biopsies, or blood tests may be required to confirm the diagnosis and determine the underlying cause. The imaging findings provide a focused approach to subsequent diagnostic steps. The results act as a crucial filter, guiding the selection of the most appropriate and effective subsequent tests.
Examples of Diagnoses and Diagnostic Aid
| Gastrointestinal Disorder | How Upper GI/Small Bowel Series Can Be Helpful |
|---|---|
| Peptic Ulcer Disease | Visualization of ulcers in the stomach or duodenum, helping to determine the extent and location of the ulcer. |
| Esophageal Stricture | Detection of narrowing or constriction in the esophagus, crucial for determining the cause and planning treatment options. |
| Crohn’s Disease | Identification of inflammation, strictures, and fistulas in the small intestine, allowing for a comprehensive assessment of disease extent. |
| Tumors (e.g., lymphoma) | Visualization of masses or abnormal growths in the GI tract, aiding in their location and size assessment. |
| Intestinal Obstruction | Detection of blockages in the small or large intestine, helping to determine the cause and the need for urgent intervention. |
Post-Procedure Considerations
After undergoing an upper GI or small bowel series, patients require careful monitoring and management to ensure a smooth recovery and minimize potential complications. This phase involves understanding post-procedure care instructions, recognizing potential problems, and implementing appropriate follow-up strategies. Proper patient education and proactive management are crucial for a positive outcome.
Patient Post-Procedure Care Instructions
Patient education plays a vital role in successful recovery. Clear instructions regarding dietary restrictions, activity limitations, and medication adherence are essential. Patients should be educated on the importance of reporting any unusual symptoms, such as abdominal pain, nausea, vomiting, or fever, immediately to their healthcare provider. Specific instructions might include avoiding strenuous activity, maintaining a soft diet for a few days, and taking prescribed medications as directed.
Potential Complications and Management
While upper GI and small bowel series are generally safe procedures, potential complications can arise. These can range from minor discomfort to more serious issues. Mild discomfort, such as bloating or cramping, is common and usually resolves spontaneously. However, more severe complications like perforation, bleeding, or infection require prompt medical attention. Prompt diagnosis and appropriate interventions are key in managing these complications effectively.
Follow-Up Procedures
Follow-up procedures may be necessary depending on the patient’s individual circumstances and the findings of the initial imaging study. These could include repeat imaging studies, such as additional X-rays or CT scans, or endoscopic procedures to further investigate any abnormalities detected during the initial imaging. This allows for more detailed analysis and the confirmation or dismissal of potential issues.
Importance of Monitoring Patients After the Procedure
Close monitoring of patients after the procedure is crucial for early detection and management of any complications. Regular observation for signs of infection, bleeding, or other adverse effects is essential. This proactive approach helps prevent serious complications and ensures prompt intervention if necessary. A dedicated healthcare team can effectively monitor vital signs, observe for any unusual symptoms, and respond appropriately.
Table of Post-Procedure Considerations
| Post-Procedure Aspect | Potential Complications | Follow-up Protocols |
|---|---|---|
| Dietary Restrictions | Nausea, vomiting, abdominal discomfort | Soft diet for a few days, gradual return to normal diet as tolerated. |
| Activity Limitations | Increased abdominal pain, discomfort | Avoid strenuous activity for a few days. |
| Medication Adherence | Uncontrolled symptoms, delayed healing | Adhere to medication schedule as prescribed. Report any medication-related issues. |
| Symptom Reporting | Abdominal pain, fever, bleeding, infection | Immediate reporting to healthcare provider. Further imaging or other diagnostic tests may be necessary. |
| Monitoring Vital Signs | Signs of infection, dehydration, or other complications | Regular monitoring of temperature, pulse, and blood pressure. |
Advanced Techniques and Variations
Diving deeper into the world of upper GI and small bowel series, we encounter a fascinating array of advanced techniques. These methods offer enhanced visualization and diagnostic capabilities, often surpassing the limitations of traditional approaches. They provide crucial insights into subtle pathologies and allow for more precise diagnoses, ultimately improving patient care.Advanced imaging techniques in upper GI and small bowel series are continually evolving, incorporating innovations in equipment and contrast agents.
This evolution allows for better delineation of subtle abnormalities, leading to more accurate diagnoses and tailored treatment plans. The ability to visualize the intricate structures of the gastrointestinal tract with greater precision and detail is crucial in managing various digestive disorders.
Newer Imaging Techniques
Several newer imaging techniques are revolutionizing the way we approach upper GI and small bowel series. These techniques often involve specialized equipment and contrast agents, offering improved visualization and diagnostic capabilities compared to traditional methods. Examples include CT enterography, which combines computed tomography (CT) with contrast agents to produce detailed images of the small bowel, and magnetic resonance enterography (MRE), which leverages the magnetic properties of the body to produce high-resolution images of the small bowel without the use of ionizing radiation.
These techniques have emerged as powerful tools for evaluating complex small bowel pathologies.
Specialized Equipment
Specialized equipment plays a critical role in these advanced imaging techniques. High-resolution CT scanners with advanced reconstruction algorithms, for instance, are used in CT enterography to obtain detailed images of the small bowel. Similarly, specialized MR coils are utilized in MRE to enhance image quality and reduce artifacts. The use of advanced equipment allows for superior image resolution and visualization, leading to more precise diagnoses and treatment planning.
Contrast Agents
Advanced contrast agents are crucial for enhancing the visibility of the gastrointestinal tract in these procedures. Novel contrast agents with improved characteristics, such as longer half-lives or tailored molecular structures, enhance the contrast and provide more detailed images. Moreover, the ability to customize contrast agents to target specific structures or pathologies further enhances the diagnostic capabilities. The improved contrast provided by these agents leads to a better understanding of the structures and potential abnormalities present.
Benefits and Limitations of Advanced Techniques
Advanced techniques offer several advantages over traditional methods. Firstly, they provide higher resolution images, enabling detection of subtle abnormalities that might be missed with conventional approaches. Secondly, they can offer real-time visualization in certain cases, facilitating the dynamic assessment of motility and function. Thirdly, some advanced techniques, like MRE, reduce the need for ionizing radiation, which is a significant benefit for patients, especially children or those requiring frequent imaging.
However, these techniques also have limitations. They may be more expensive, require specialized equipment and personnel, and might not be readily available in all healthcare settings. Furthermore, some advanced techniques, such as CT enterography, expose patients to ionizing radiation.
Comparison of Traditional and Advanced Techniques
| Feature | Traditional Upper GI/Small Bowel Series | Advanced Techniques (CT Enterography/MRE) |
|---|---|---|
| Resolution | Moderate | High |
| Visualization of small bowel | Limited | Excellent |
| Detection of subtle abnormalities | Limited | Enhanced |
| Radiation exposure | Low | Higher (CT Enterography) |
| Cost | Lower | Higher |
| Availability | More widespread | Less widespread |
This table highlights the key differences between traditional and advanced imaging techniques in upper GI and small bowel series. The advanced techniques offer significant improvements in terms of resolution, visualization, and detection capabilities, but they also come with trade-offs in terms of cost and availability.
Illustrative Examples
Diving deeper into the practical applications of upper GI and small bowel series, let’s explore real-world case studies. These examples highlight the diagnostic power of these imaging techniques, demonstrating how they can identify various conditions and guide treatment decisions. Understanding these cases provides a valuable perspective on the utility of these procedures in clinical practice.
Case Study 1: Suspected Upper GI Disorder
A 45-year-old male presented with persistent heartburn, dysphagia, and occasional regurgitation. His medical history was unremarkable, except for a reported history of GERD in the past. The upper GI series revealed a narrowing in the distal esophagus, suggestive of a stricture. Further investigations, including endoscopy, confirmed the presence of a peptic stricture, likely caused by chronic GERD.
The imaging findings correlated with the patient’s symptoms, providing a clear diagnostic picture and guiding treatment options, such as endoscopic dilation or medication adjustments.
Case Study 2: Suspected Small Bowel Obstruction
A 65-year-old female presented with acute abdominal pain, nausea, and vomiting, along with constipation. The patient’s medical history included a recent appendectomy. The small bowel series demonstrated a significant narrowing and dilation of the small bowel, consistent with a mechanical obstruction. Further investigation confirmed the presence of adhesions, resulting from the previous surgical procedure, as the cause of the obstruction.
This case illustrates the crucial role of a small bowel series in detecting and localizing mechanical obstructions, enabling prompt intervention and preventing complications.
Case Scenario with Detailed Description
A 32-year-old female presented with intermittent abdominal pain, bloating, and diarrhea for the past six months. She reported a history of food intolerances and occasional bouts of nausea. Physical examination revealed mild tenderness in the right upper quadrant. The upper GI series showed no abnormalities in the esophagus, stomach, or duodenum. However, the small bowel series revealed a segment of dilated and thickened small bowel loops, with multiple areas of narrowing, suggestive of Crohn’s disease.
Further investigations, including colonoscopy and biopsies, confirmed the diagnosis of Crohn’s disease. This case demonstrates how a combination of upper and small bowel series can be instrumental in identifying subtle small bowel pathologies, particularly when the clinical presentation is non-specific.
Case Scenario with Normal and Abnormal Findings
The following table illustrates a comparison of normal and abnormal findings in a small bowel series.
| Finding | Normal | Abnormal |
|---|---|---|
| Small Bowel Appearance | Smooth, continuous loops with consistent caliber | Dilated, thickened, or narrowed loops, with skip lesions or strictures |
| Intestinal Pattern | Uniform distribution of contrast medium | Uneven distribution of contrast medium, with areas of obstruction or stasis |
| Gas Pattern | Minimal gas pockets throughout the small bowel | Significant gas pockets or air fluid levels, especially in obstructed areas |
| Transit Time | Normal transit of contrast medium | Delayed transit or stasis of contrast medium |
The normal small bowel series reveals smooth, continuous loops of small bowel with a uniform distribution of contrast. Abnormal findings include dilated or narrowed loops, skip lesions, strictures, and delayed transit. These differences are critical in distinguishing between normal and abnormal small bowel function. The illustrative diagrams below depict these variations.
Diagram 1 (Normal): A series of smooth, continuous loops of small bowel filled with contrast medium, showing consistent caliber and transit time.
Diagram 2 (Abnormal): A segment of dilated and thickened small bowel loops with a narrowed segment and delayed contrast medium transit. The abnormal findings in this diagram are suggestive of a mechanical obstruction.
Final Thoughts
In conclusion, upper GI and small bowel series remain invaluable diagnostic tools for evaluating the upper gastrointestinal tract and small intestines. Their ability to visualize anatomical structures, identify potential abnormalities, and guide treatment plans is unparalleled. While traditional methods are still prevalent, newer techniques and variations are constantly emerging. By understanding the preparation, procedure, interpretation, and post-procedure care, both patients and healthcare providers can navigate this process with confidence and ensure optimal patient outcomes.
The detailed information and case studies included will hopefully provide a thorough understanding of this important diagnostic procedure.
