Using stem cells to heal broken bones is a rapidly evolving field with the potential to revolutionize bone fracture treatment. This exciting area explores how stem cells, like mesenchymal stem cells and bone marrow-derived stem cells, can stimulate bone regeneration. We’ll delve into the mechanisms behind this process, examining current research, clinical trials, and delivery methods. From the challenges and ethical considerations to successful case studies, we’ll cover it all.
This exploration will provide a comprehensive overview of this promising treatment.
Stem cell therapy offers a potential alternative to traditional bone repair methods, such as surgery and casting. This approach aims to address the limitations of traditional techniques by promoting natural bone regeneration. We will examine the advantages and disadvantages of different stem cell types and delivery methods, providing a detailed comparison that will equip you with a better understanding of this evolving field.
Introduction to Stem Cell Therapy for Bone Fractures: Using Stem Cells To Heal Broken Bones
Stem cell therapy is rapidly emerging as a promising avenue for treating various medical conditions, including bone fractures. This innovative approach leverages the body’s inherent regenerative capacity by utilizing specialized cells to stimulate bone growth and repair. The potential for accelerated healing and reduced recovery time makes stem cell therapy a compelling alternative to traditional treatments for certain fracture types.Stem cells are undifferentiated cells with the remarkable ability to develop into various specialized cell types, including bone cells.
Their inherent plasticity allows them to participate in the intricate processes of bone regeneration, potentially offering a solution to challenging or difficult-to-treat fractures. This approach holds significant promise for patients with delayed or non-union fractures, where traditional methods have proven insufficient.
Types of Stem Cells Used in Bone Repair
Various types of stem cells show promise in bone fracture healing. Understanding their characteristics and potential benefits is crucial for optimizing treatment strategies.
Stem cell treatments are showing promising results in healing broken bones, fostering new bone growth and accelerating the recovery process. It’s fascinating to see how this same technology has also been used to treat other conditions like HIV, as seen in this case study of how a 4th person was cured of HIV after stem cell treatments. how a 4th person was cured of hiv after stem cell treatments.
This highlights the incredible potential of stem cells to revolutionize medicine, potentially paving the way for even faster bone repair in the future.
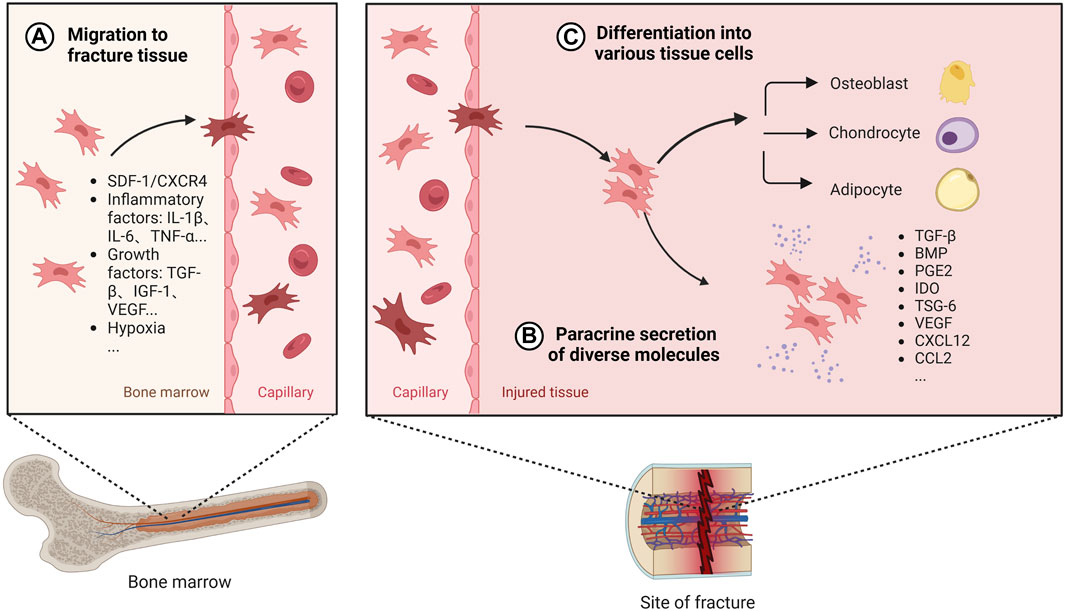
- Mesenchymal Stem Cells (MSCs) are multipotent stromal cells found in various tissues, including bone marrow. They possess the capacity to differentiate into various cell types, including osteoblasts (bone-forming cells), and chondrocytes (cartilage-forming cells). Their ability to migrate to sites of injury and promote the formation of new bone makes them attractive candidates for fracture repair.
- Bone Marrow-Derived Stem Cells (BMSCs) are a subset of mesenchymal stem cells found within bone marrow. They are readily accessible and relatively easy to isolate, making them a practical choice for clinical applications. These cells have shown efficacy in promoting bone formation and vascularization at the fracture site, contributing to a more robust healing response.
Mechanisms of Stem Cell Action in Bone Regeneration
Stem cells play a multifaceted role in the bone regeneration process. Their actions are not limited to direct differentiation into bone-forming cells.
- Secretion of Growth Factors: Stem cells release a plethora of growth factors that stimulate the proliferation and differentiation of osteoblasts, directly influencing bone formation. Examples of these growth factors include transforming growth factor-β (TGF-β), insulin-like growth factor-1 (IGF-1), and vascular endothelial growth factor (VEGF).
- Promoting Angiogenesis: Stem cells promote the formation of new blood vessels (angiogenesis) at the fracture site. This increased blood supply is critical for delivering essential nutrients and oxygen to the healing tissues, accelerating the entire process of bone regeneration.
- Reducing Inflammation: Stem cells can modulate the inflammatory response at the fracture site, preventing excessive inflammation that can hinder bone healing. This delicate balance is critical for successful fracture repair.
Comparison of Stem Cell Types, Using stem cells to heal broken bones
| Stem Cell Type | Advantages | Disadvantages |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Versatility in differentiation, readily available from various tissues, potential for autologous transplantation | Variability in efficacy depending on source, potential for immune rejection, need for appropriate expansion techniques |
| Bone Marrow-Derived Stem Cells (BMSCs) | Relatively easy isolation, abundant availability, well-established safety profile | Limited proliferative capacity compared to some other sources, potential for contamination with other cell types |
Current Research and Clinical Trials
Stem cell therapy for bone fractures is a rapidly evolving field, promising innovative approaches to bone healing. Researchers are actively exploring various stem cell types and delivery methods to optimize fracture repair. This section delves into the current state of research, highlighting key areas of investigation and the progress being made through clinical trials.
Current Research Areas
Research into stem cell therapies for bone fractures is multifaceted. Researchers are investigating different stem cell sources, including mesenchymal stem cells (MSCs) derived from bone marrow, adipose tissue, and umbilical cord blood. This diversity reflects the quest for efficient and readily available cell sources. Furthermore, studies are exploring the optimal methods for delivering these cells to the fracture site, examining the potential benefits of scaffolds and growth factors.
Techniques for enhancing cell viability and promoting integration with the surrounding tissue are also crucial aspects of this research.
Clinical Trial Design and Stages
Clinical trials are essential for evaluating the safety and efficacy of stem cell therapies. These trials meticulously follow a standardized process, typically progressing through phases. Understanding these phases is critical for evaluating the reliability of results.
| Stage | Description |
|---|---|
| Phase 1 | This initial phase focuses on establishing the safety of the therapy in a small group of patients. Researchers carefully monitor for adverse effects and identify appropriate dosages. The primary goal is to determine a safe dose range for future trials. For example, in a Phase 1 trial, researchers might administer different concentrations of stem cells to assess tolerance. |
| Phase 2 | Phase 2 trials expand the study population to evaluate the therapy’s efficacy and further refine dosage regimens. Researchers investigate the treatment’s potential benefits in relation to fracture healing. This stage might involve comparing stem cell therapy to standard treatments, like surgery or casts. For instance, a Phase 2 trial could assess whether stem cell injections accelerate bone union in patients with delayed union fractures. |
| Phase 3 | Phase 3 trials involve a larger cohort of patients to confirm the efficacy and safety of the therapy in a wider clinical setting. These trials often compare the treatment to existing standard-of-care treatments. The goal is to establish the treatment’s clinical significance and potential impact on patient outcomes. For example, a Phase 3 trial might compare the long-term bone healing outcomes of patients treated with stem cells to those treated with conventional methods. The results obtained from this phase provide strong evidence for the therapy’s use in routine clinical practice. |
Key Breakthroughs and Examples
Several promising breakthroughs have emerged in recent years. For example, researchers have demonstrated that certain types of stem cells can stimulate bone regeneration by increasing the production of bone-forming cells. Another key area of research focuses on combining stem cell therapies with other regenerative medicine approaches, such as biomaterials and growth factors. This combined approach holds immense potential for accelerating bone healing and improving patient outcomes.
Clinical trials are actively evaluating these novel strategies, and initial results are promising. One example includes a study examining the use of adipose-derived stem cells to promote healing in tibia fractures. Another study investigated the use of MSCs in combination with a biocompatible scaffold to enhance bone regeneration.
Methods and Procedures for Stem Cell Delivery
Stem cell therapy for bone fractures holds immense promise, but successful treatment hinges on effectively delivering these cells to the injury site. The journey from isolating stem cells to precisely placing them at the fracture site involves intricate procedures and various delivery methods. Careful consideration of each method’s advantages and limitations is crucial for optimal outcomes.The efficacy of stem cell therapy hinges on their ability to reach the fracture site and initiate the healing process.
Precise delivery methods are paramount, ensuring stem cells reach the damaged area while minimizing adverse effects. Different methods offer varying degrees of control over cell localization and survival.
Stem Cell Isolation and Expansion
Stem cells, often derived from bone marrow or adipose tissue, need careful isolation and expansion to achieve sufficient numbers for therapeutic use. Bone marrow aspirates are commonly used, requiring sterile procedures to minimize contamination. Specific protocols for isolating mesenchymal stem cells (MSCs) from the aspirate are meticulously followed. These protocols typically involve cell surface markers and specific culture media to enrich and expand the MSC population.
This expansion process aims to generate a sufficient number of viable cells for treatment while maintaining their therapeutic potential.
Delivery Methods
Various methods for delivering stem cells to the fracture site exist, each with its own advantages and drawbacks.
- Direct Injection: This method involves directly injecting the isolated and expanded stem cells into the fracture site. It’s a relatively simple technique, minimizing the need for additional materials. However, precise targeting of the fracture site can be challenging, and the cells may not always reach the desired location in sufficient quantities. Potential challenges include cell loss during injection, inadequate cell penetration into the fracture site, and the risk of inducing inflammation or other adverse reactions.
- Scaffolds: Scaffolds are biocompatible materials designed to provide a supportive framework for cell growth and tissue regeneration. These scaffolds can be implanted at the fracture site and seeded with stem cells. This method can enhance cell retention and facilitate tissue regeneration. Examples include biodegradable polymers, natural materials like collagen, and ceramic scaffolds. However, proper scaffold design and material selection are critical to ensure biocompatibility, mechanical stability, and optimal cell integration.
Potential challenges include scaffold degradation, the potential for inflammatory reactions to the scaffold material, and ensuring appropriate cell-scaffold interactions.
- Genetically Modified Stem Cells: Stem cells can be genetically modified to enhance their therapeutic efficacy. For instance, they can be modified to express growth factors that stimulate bone regeneration or to express fluorescent proteins to track their migration and localization within the fracture site. This method requires sophisticated genetic engineering techniques and poses risks related to potential off-target effects or uncontrolled gene expression.
Potential challenges include the ethical considerations surrounding gene modification and the potential for unpredictable long-term effects.
- Combination Approaches: Combining different delivery methods can maximize the benefits and minimize the drawbacks of individual approaches. For instance, stem cells can be loaded onto scaffolds and then injected into the fracture site. This approach aims to improve the targeting and retention of cells while minimizing cell loss. Potential challenges include the complexity of combining methods and ensuring compatibility between the different components.
Effectiveness Comparison
A comparative analysis of different delivery methods is complex and dependent on several factors, including the specific fracture characteristics, the type of stem cells used, and the overall patient condition. Currently, there is ongoing research to evaluate the effectiveness of each method and identify optimal strategies for bone fracture healing. No single method has consistently proven superior to others in all situations.
Clinical trials are essential to gather more data and establish clear benchmarks for optimal stem cell delivery strategies.
Challenges and Future Directions
Stem cell therapy holds immense promise for treating bone fractures, offering a potential pathway to accelerate healing and minimize long-term complications. However, several hurdles need to be addressed before widespread clinical adoption. Understanding these challenges and potential solutions is crucial for navigating the path toward effective and safe stem cell-based therapies for bone repair.Current stem cell therapies face limitations in terms of efficacy and reproducibility, and the field continues to evolve.
Addressing these challenges through innovative research will pave the way for the development of more reliable and broadly applicable treatments.
Key Challenges in Stem Cell Therapy for Bone Fractures
The application of stem cell therapy for bone fractures is not without its challenges. These range from the complex biology of stem cell differentiation and engraftment to the practical considerations of delivering and monitoring the treatment.
Stem cell therapies show promise for mending broken bones, with the potential to accelerate the healing process. However, while the science behind these treatments is fascinating, it’s important to consider that there’s currently no definitive proof that energy drinks harm blood vessels, a factor potentially influencing bone repair. So, while we explore the regenerative potential of stem cells, it’s crucial to stay informed about the latest research, like this study on the impact of energy drinks on the vascular system, no proof energy drinks harm blood vessels , and continue to focus on proven methods to support bone health.
- Stem Cell Source and Differentiation: Ensuring a consistent and sufficient supply of suitable stem cells is a critical challenge. Different stem cell sources, such as bone marrow-derived mesenchymal stem cells (MSCs) or induced pluripotent stem cells (iPSCs), have varying differentiation potentials and therapeutic effects. Further research is needed to identify the optimal stem cell type and culture conditions to promote robust bone regeneration.
- Delivery Methods and Targeting: Effective delivery of stem cells to the fracture site remains a hurdle. Stem cells need to be transported to the precise location of injury, while minimizing loss and ensuring their survival and integration into the surrounding tissue. Development of advanced delivery methods, such as targeted drug delivery systems, will be critical.
- Immunogenicity and Safety: The immune response to transplanted stem cells can be unpredictable and may lead to rejection or inflammation. The risk of tumorigenesis and other adverse effects also requires careful monitoring and mitigation strategies. Developing strategies to minimize immunogenicity and ensure the safety of stem cell therapies is paramount.
- Cost and Accessibility: The cost of stem cell therapies, including cell isolation, culture, and administration, can be prohibitive, potentially limiting access to this treatment for many patients. Research and development focusing on cost-effective and scalable production methods are essential for widespread application.
- Reproducibility and Standardization: Consistency in treatment outcomes is crucial for clinical validation. Developing standardized protocols for stem cell isolation, culture, and delivery will be essential to ensure reproducibility and comparable results across different treatment centers and patient populations.
Potential Solutions and Future Research Directions
Addressing the challenges Artikeld above requires a multi-pronged approach.
- Improved Stem Cell Delivery: Advanced biomaterials and nanotechnology could enhance stem cell delivery, increasing their retention at the fracture site and promoting their integration with the surrounding bone tissue. Research into targeted drug delivery systems that direct stem cells to the fracture site and stimulate bone regeneration could be a promising avenue.
- Enhanced Stem Cell Differentiation: Understanding the molecular mechanisms regulating stem cell differentiation could lead to the development of strategies to direct stem cell differentiation towards specific bone cell types. This approach could potentially enhance bone formation and reduce the need for lengthy treatment durations.
- Minimizing Immunogenicity: Strategies to mitigate the immune response to transplanted stem cells, such as pre-conditioning the recipient or modifying the stem cells themselves, could significantly improve the safety and efficacy of stem cell therapies. Developing immunosuppressive strategies could minimize the risks associated with immune rejection.
- Cost-Effective Production Methods: Scalable and cost-effective methods for producing large quantities of high-quality stem cells are crucial for broader accessibility. Research into novel bioreactor systems and automated cell culture techniques could dramatically reduce the cost and improve the efficiency of stem cell production.
- Ethical Considerations: Ethical considerations surrounding stem cell research and clinical application should be carefully addressed. Transparency in clinical trials, informed consent, and responsible oversight are critical to ensure ethical practices throughout the process.
Ethical Considerations in Stem Cell Research and Clinical Application
Ethical considerations are paramount in stem cell research and clinical application. Strict adherence to ethical guidelines is essential to protect patients and ensure responsible progress in this field.
- Informed Consent: Patients undergoing stem cell therapies must be fully informed about the risks and benefits, as well as alternative treatment options, before providing consent. Open communication and clear understanding are essential for patient autonomy.
- Transparency in Research: Clinical trials must be conducted transparently, with all data publicly available and accessible for peer review. Rigorous evaluation and oversight are critical to maintain quality and integrity.
- Responsible Oversight: Appropriate regulatory oversight and ethical review boards are crucial to ensure the safety and efficacy of stem cell therapies. Clear guidelines and standards should be established to guide the development and implementation of new treatments.
Illustrative Case Studies
Stem cell therapy for bone fractures is rapidly evolving, moving from laboratory experiments to promising clinical applications. Observing real-world patient outcomes is crucial to understanding the efficacy and limitations of this approach. Detailed case studies provide valuable insights into the nuances of treatment and help refine future strategies.This section presents several case studies highlighting successful applications of stem cell therapy in treating bone fractures.
These examples illustrate the diverse patient populations and fracture characteristics where stem cell therapy can be beneficial, while also acknowledging the factors influencing treatment outcomes.
Patient Demographics and Fracture Characteristics
Case studies often include detailed information about the patient’s age, gender, medical history, and the specific characteristics of the fracture. These factors can influence the healing process and the potential effectiveness of stem cell therapy. For instance, a younger patient with a healthy immune system and a relatively uncomplicated fracture might respond better to treatment compared to an older patient with pre-existing conditions or a complex fracture.
Treatment Outcomes
The outcomes of stem cell therapy for bone fractures are evaluated based on several criteria. These include the rate of bone healing, the quality of the regenerated bone, and the reduction in pain and functional limitations. Successful cases often show a significant acceleration in fracture healing, resulting in improved mobility and a return to normal activities. The specific outcomes depend on factors like the type of stem cells used, the delivery method, and the individual patient’s response.
Factors Contributing to Success or Failure
Several factors can influence the success or failure of stem cell therapy for bone fractures. Patient-specific factors, such as pre-existing health conditions, nutritional status, and adherence to post-treatment protocols, play a crucial role. Furthermore, the quality and viability of the administered stem cells, the precise method of delivery, and the surgeon’s expertise are critical components in achieving positive outcomes.
Stages of Bone Healing
| Stage | Healing without Stem Cell Therapy | Healing with Stem Cell Therapy |
|---|---|---|
| Inflammation (Days 1-3) | Initial inflammatory response, blood clot formation, and recruitment of immune cells. | Similar inflammatory response, but potentially accelerated due to enhanced cell recruitment and signaling. |
| Repair (Days 3-21) | Formation of a soft callus, comprising cartilage and collagen, bridging the fracture gap. | Faster formation of a stronger callus, potentially with higher density of osteoblasts and faster mineralization, potentially enhanced angiogenesis. |
| Remodeling (Weeks-Months) | Gradual replacement of the soft callus with hard bone tissue, remodeling and strengthening of the new bone structure. | Increased rate of bone remodeling and structural strengthening. |
The table above visually represents the stages of bone healing with and without stem cell therapy. Note that stem cell therapy is expected to accelerate and enhance the healing process. However, factors like patient health and fracture severity influence the ultimate outcome.
Stem cell therapies are showing promise in repairing broken bones, offering a potential solution for faster healing. However, it’s crucial to consider other health risks, like the dangers of rat lungworm disease, which can lead to severe complications. Understanding the risks associated with such parasitic infections is key to evaluating the overall safety of treatments like stem cell therapy for broken bones.
This article, how dangerous is rat lungworm disease , offers insights into the severity of this often-overlooked illness. Ultimately, advancements in stem cell therapies hold significant potential for treating broken bones, and careful consideration of related health concerns like rat lungworm disease is vital for safe and effective medical practices.
Comparison with Traditional Bone Repair Methods
Stem cell therapy for bone fractures presents a compelling alternative to traditional methods, promising faster healing and potentially better long-term outcomes. However, the efficacy, safety profile, and cost-effectiveness of this approach need careful comparison with established techniques. Understanding the nuances of each method is crucial for informed decision-making.Traditional methods like surgery and casting have served as cornerstones of bone fracture management for decades.
These approaches have proven reliable in many cases, but limitations exist, particularly in scenarios involving complex fractures or delayed healing.
Effectiveness of Approaches
Traditional methods like surgical intervention, involving the precise realignment of bone fragments and the use of plates, screws, or other implants, aim to restore the structural integrity of the fractured bone. Casting immobilizes the affected area, allowing the bone to heal in a stable position. The effectiveness of these methods depends heavily on the type and severity of the fracture, as well as the patient’s overall health.
Surgical interventions, while often effective, can carry risks, including infection, complications related to the implant, and potential damage to surrounding tissues. Casting, while less invasive, can lead to stiffness and limited mobility in the affected area.
Safety Considerations
The safety profile of stem cell therapy is an evolving area of research. While generally considered safe, potential risks, such as infection, immune response, and tumor formation, require rigorous monitoring. Traditional methods, such as surgery and casting, also carry inherent risks. Surgical interventions, for example, can lead to complications like bleeding, nerve damage, or blood clots. Casting, though generally safe, can lead to skin irritation or pressure sores if not properly managed.
Cost-Effectiveness Analysis
The cost-effectiveness of stem cell therapy is a complex issue, as it is a relatively new field. Initial costs associated with stem cell collection, processing, and application can be significantly higher than traditional methods. However, long-term cost implications, such as reduced need for future surgeries or rehabilitation, could potentially offset these initial expenses. Traditional methods, while having lower upfront costs, might incur higher long-term expenses if complications arise or if the fracture does not heal optimally.
Summary Table
| Feature | Stem Cell Therapy | Traditional Methods (Surgery/Casting) |
|---|---|---|
| Effectiveness | Potentially faster healing, improved bone regeneration in some cases. | Generally effective for uncomplicated fractures, but limitations exist for complex or delayed healing. |
| Safety | Generally safe, but potential for complications (infection, immune response) requires careful monitoring. | Inherent risks, including infection, bleeding, nerve damage, or implant-related complications. |
| Cost | Higher initial cost; potential for lower long-term costs depending on outcomes. | Lower initial cost; potential for higher long-term costs due to complications or need for further interventions. |
| Recovery Time | Potentially faster recovery due to accelerated bone regeneration. | Variable recovery time depending on fracture severity and individual factors. |
| Patient Factors | Patient’s overall health, bone density, and specific fracture characteristics. | Patient’s overall health, bone density, and fracture characteristics. |
Potential Risks and Complications
Stem cell therapy, while promising, carries inherent risks, just like any medical procedure. Understanding these potential complications is crucial for informed decision-making and ensuring patient safety. Careful patient selection and rigorous monitoring protocols are paramount to mitigate these risks and maximize the benefits of the therapy.
Potential Side Effects and Adverse Events
Stem cell therapy for bone fractures, like any treatment, can have potential side effects. These can range from mild discomfort to more serious complications. The body’s reaction to the introduced stem cells, the specific type of stem cells used, and the method of delivery all influence the likelihood and severity of side effects. Careful monitoring of the patient post-treatment is essential to promptly identify and manage any adverse events.
Importance of Patient Selection and Monitoring
Careful patient selection is critical to minimize risks. Patients with pre-existing conditions, such as immune deficiencies or clotting disorders, may be at a higher risk of complications from stem cell therapy. Thorough evaluation and assessment of a patient’s overall health are essential. Monitoring patients post-treatment is crucial to promptly identify and manage any adverse reactions or complications.
Regular checkups, including blood tests and imaging studies, are vital to track the healing process and detect any potential issues early on. This close monitoring ensures appropriate intervention if complications arise.
Categorization of Potential Complications
Careful consideration and documentation of potential complications are essential for responsible stem cell therapy. This is crucial for both clinicians and patients. The following table summarizes potential complications, categorized by likelihood and potential severity.
| Category | Potential Complications | Likelihood | Severity | Management Strategies |
|---|---|---|---|---|
| Local | Inflammation, swelling, pain at the fracture site, hematoma formation | High | Mild to Moderate | Pain management, ice packs, elevation, rest |
| Infectious | Infection at the injection site or fracture site, systemic infection | Moderate | Moderate to Severe | Antibiotics, surgical intervention (if necessary) |
| Immune | Immune rejection, allergic reaction, graft-versus-host disease (rare) | Low | Variable | Immunosuppressants, supportive care |
| Vascular | Blood clots, bleeding, thrombosis | Moderate | Moderate to Severe | Anticoagulants, thrombolytics, supportive care |
| Tumorigenesis | Risk of tumor development, particularly in cases of undifferentiated or immature stem cells (rare) | Very Low | High | Long-term follow-up, close monitoring |
Regulatory Landscape and Future Implications
Stem cell therapies, while promising, face significant regulatory hurdles before widespread adoption in bone fracture treatment. Navigating these complexities is crucial for ensuring patient safety and efficacy. This section delves into the current regulatory landscape, highlighting potential future implications for both healthcare and the broader field of regenerative medicine.The regulatory environment for stem cell therapies is intricate and differs significantly across jurisdictions.
Standardization and rigorous testing are paramount to mitigate the risks associated with off-label use and unregulated products.
Regulatory Approvals and Guidelines
The approval process for stem cell therapies is often lengthy and demanding. Specific regulatory pathways and guidelines are established by governing bodies like the FDA in the US, EMA in Europe, and similar agencies in other countries. These pathways typically involve rigorous preclinical and clinical trials to demonstrate safety and efficacy. The standards for data collection, analysis, and reporting are meticulously defined to ensure that only therapies that meet stringent criteria are approved for use in patients.
Potential Impact on the Future of Bone Fracture Treatment
Stem cell therapy holds the potential to revolutionize bone fracture treatment. The ability to accelerate bone healing, potentially reducing recovery times and minimizing the need for invasive procedures, presents a significant advancement. Early clinical trials are showing promising results, but wider implementation hinges on successful regulatory approvals and robust clinical evidence.
Potential Impact on Healthcare Costs and Accessibility
The cost-effectiveness of stem cell therapy for bone fractures is a key consideration. While initial costs may be higher than traditional methods, the long-term benefits, such as reduced rehabilitation time and potentially lower overall healthcare expenditure, need to be evaluated. Ensuring accessibility for all patients, regardless of socioeconomic status, is a crucial consideration in the future implementation of this therapy.
Factors such as treatment costs, availability of specialized personnel, and the geographic location of treatment centers will impact equitable access. Cost-benefit analyses and potential cost-sharing models are essential to address these issues. Comparative cost analysis with traditional methods needs to be considered, focusing on long-term outcomes to accurately predict cost-effectiveness.
Last Word
In conclusion, using stem cells to heal broken bones presents a compelling prospect for enhanced bone fracture treatment. While challenges remain, the potential benefits are significant, especially when compared to traditional methods. Further research and clinical trials are crucial to refine delivery methods, improve stem cell differentiation, and ensure ethical considerations are addressed. The future of bone fracture treatment could be profoundly impacted by this innovative approach.
Let’s keep an eye on the progress in this exciting area!
