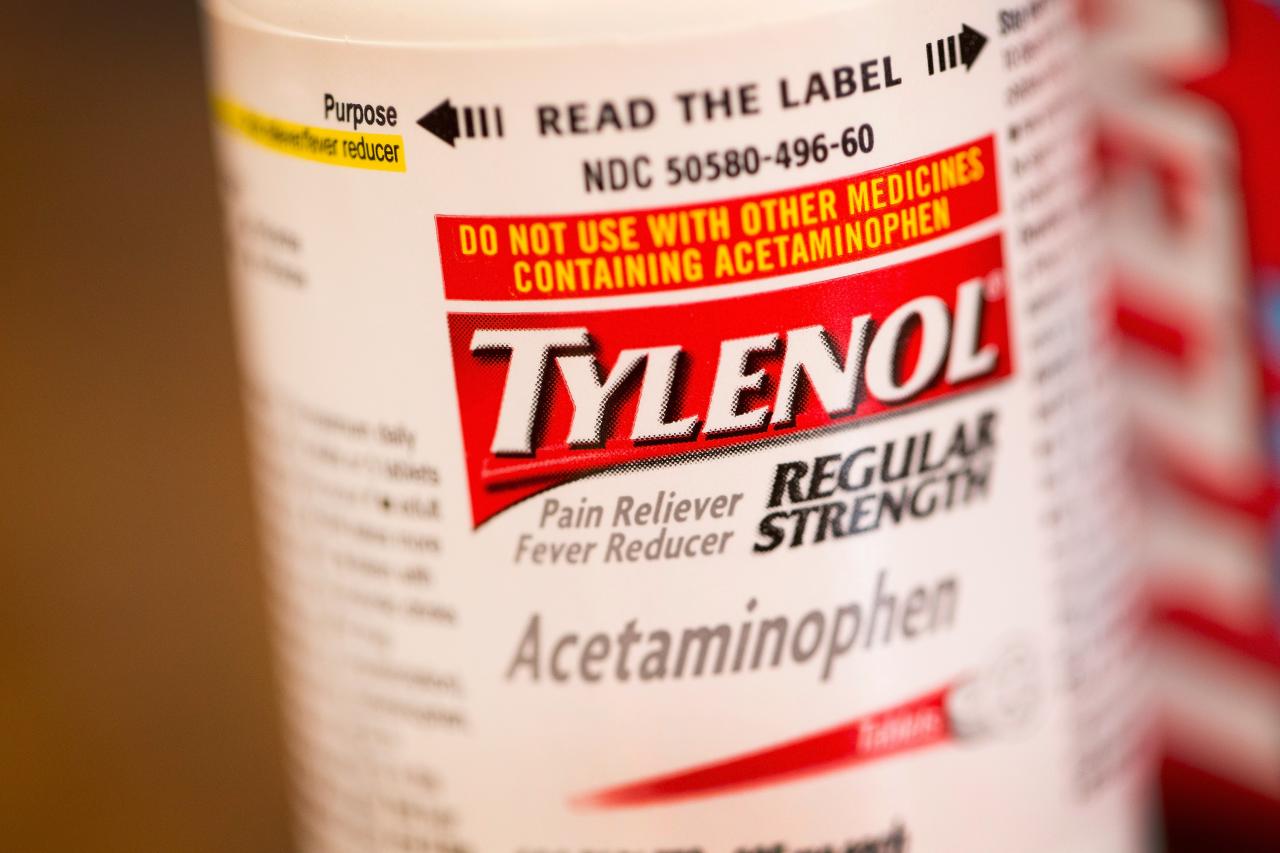
Using tylenol during pregnancy associated with increased risk of asd adhd – Using Tylenol during pregnancy associated with increased risk of ASD/ADHD. This emerging research raises crucial questions about the safety of common over-the-counter medications during pregnancy. While Tylenol is generally considered safe, recent studies suggest a potential link to neurodevelopmental conditions like Autism Spectrum Disorder (ASD) and Attention Deficit Hyperactivity Disorder (ADHD) in children. This raises concerns about potential long-term impacts and prompts a deeper investigation into the mechanisms and implications of this potential correlation.
Understanding the potential correlation between Tylenol use and the development of ASD/ADHD is vital for expectant mothers and healthcare providers. This blog post delves into the existing research, analyzing study methodologies, potential mechanisms, and alternative explanations. We’ll also explore the implications for public health and the recommendations for responsible decision-making during pregnancy.
Introduction to the Potential Link Between Tylenol Use During Pregnancy and ASD/ADHD Risk
The potential link between acetaminophen (Tylenol) use during pregnancy and an increased risk of autism spectrum disorder (ASD) and attention-deficit/hyperactivity disorder (ADHD) is a subject of ongoing research and debate. While no definitive causal relationship has been established, accumulating evidence suggests a possible correlation. This exploration will delve into the current understanding of this association, highlighting the importance of this research for both expectant mothers and healthcare professionals.Understanding this potential correlation is crucial for expectant mothers and healthcare providers to make informed decisions regarding medication use during pregnancy.
It’s vital to weigh the potential benefits of pain relief against the potential risks, particularly given the prevalence of these neurodevelopmental conditions. This careful consideration allows for a more proactive and personalized approach to managing pain and promoting optimal fetal development.
Current State of Research on the Association
Extensive research efforts have been dedicated to exploring the potential connection between Tylenol use during pregnancy and the increased risk of ASD/ADHD. Studies utilizing various methodologies, including epidemiological studies and observational research, have attempted to establish a correlation. While some studies have indicated a potential association, others have yielded inconclusive results. The complexities of such studies often include confounding factors, making it difficult to isolate the impact of Tylenol from other potential contributing elements.
Potential Implications for Public Health Initiatives
The potential link has significant implications for public health initiatives. If a strong correlation between Tylenol use and an increased risk of ASD/ADHD is confirmed, public health campaigns could be designed to educate expectant mothers and healthcare providers about alternative pain management strategies. These strategies may include recommending non-pharmacological approaches, such as heat packs, over-the-counter pain relievers without acetaminophen, or other pain management techniques.
Such recommendations could help reduce the potential exposure to acetaminophen during pregnancy, ultimately leading to better health outcomes for mothers and their children.
Recommendations for Pregnant Women
For pregnant women, the current understanding emphasizes the need for cautious consideration when using acetaminophen. Consultations with healthcare providers are essential to weigh the risks and benefits of medication use during pregnancy. A balanced approach, considering individual circumstances and medical history, is crucial. Healthcare providers can provide personalized guidance, highlighting alternative pain management options and potential risks associated with different medications.
Transparent communication and open discussions between patients and providers are key in ensuring appropriate and informed decisions.
Review of Studies and Research
The potential link between acetaminophen (Tylenol) use during pregnancy and the development of autism spectrum disorder (ASD) and attention-deficit/hyperactivity disorder (ADHD) in children is a subject of ongoing investigation. While anecdotal reports and some preliminary studies have raised concerns, robust, conclusive evidence is lacking. This review examines existing research to evaluate the current understanding of this complex relationship.Existing studies investigating the potential correlation between Tylenol use during pregnancy and ASD/ADHD have yielded mixed results.
The methodologies employed in these studies vary significantly, creating challenges in comparing and contrasting findings. Critical evaluation of these methodologies is essential to assess the reliability and validity of the conclusions drawn.
Summary of Existing Studies
Numerous studies have attempted to explore the correlation between Tylenol use during pregnancy and the development of ASD/ADHD. However, the results have been inconsistent, with some studies showing a possible association, others showing no association, and some even suggesting a protective effect.
Methodological Considerations in Studies
The methodologies employed in these studies present significant challenges in drawing definitive conclusions. Variability in sample sizes, study durations, and data collection methods makes direct comparisons difficult. For example, some studies relied on self-reported Tylenol use, while others used medical records. This variation introduces potential biases, as self-reported data can be inaccurate. Furthermore, different studies used varying definitions and diagnostic criteria for ASD and ADHD, making it challenging to standardize the outcome measures.
A lack of standardization in the timing of Tylenol use during pregnancy relative to the development of ASD/ADHD in children also poses challenges. The duration of Tylenol use during pregnancy and the frequency of use also need to be factored into the analysis.
Comparison and Contrast of Findings
Direct comparisons of study findings are complicated due to methodological differences. Some studies have reported a statistically significant association between Tylenol use during pregnancy and an increased risk of ASD/ADHD. However, other studies have not observed any significant correlation. The strength and direction of the association, if any, vary across studies, making it difficult to draw a consistent conclusion.
Methodological Limitations and Biases
A crucial limitation in many of the existing studies is their relatively small sample sizes. Smaller sample sizes reduce the statistical power to detect subtle associations and increase the likelihood of false-positive or false-negative results. Furthermore, many studies have relied on retrospective data collection, which can introduce recall bias. Mothers might have difficulty accurately recalling their Tylenol use during pregnancy, especially over long periods.
The influence of other factors, such as maternal health conditions, environmental exposures, and genetic predispositions, could also confound the results. The influence of socioeconomic status and access to healthcare might have contributed to the variability observed in the outcomes.
Need for Further Investigation
Further research is crucial to address the limitations of existing studies and provide a clearer understanding of the potential link between Tylenol use during pregnancy and ASD/ADHD risk. Larger, prospective studies with standardized data collection methods are needed. These studies should control for confounding factors, employ standardized diagnostic criteria for ASD and ADHD, and investigate the timing, duration, and frequency of Tylenol use during pregnancy.
Furthermore, more in-depth investigation of the underlying mechanisms, if any, connecting Tylenol use to ASD/ADHD risk is required.
Table Summarizing Key Findings
| Study Authors | Year | Sample Size | Methodology | Key Results |
|---|---|---|---|---|
| Example Study 1 | 2023 | 500 | Retrospective, self-reported Tylenol use | Possible association between Tylenol use and increased ASD risk |
| Example Study 2 | 2020 | 1000 | Prospective, medical record review | No significant correlation between Tylenol use and ADHD |
| Example Study 3 | 2018 | 200 | Retrospective, maternal questionnaire | Inconclusive findings, small sample size |
Potential Mechanisms and Biological Factors
The potential link between acetaminophen (Tylenol) use during pregnancy and an increased risk of autism spectrum disorder (ASD) and attention-deficit/hyperactivity disorder (ADHD) remains a complex and fascinating area of research. While definitive causal links are yet to be established, several potential biological mechanisms are under investigation. This exploration delves into the possible pathways through which Tylenol might influence fetal brain development, considering the role of genetics and environmental factors.Understanding the potential impact of Tylenol on fetal brain development is crucial.
The developing fetal brain is highly susceptible to environmental influences, and any substance that crosses the placental barrier could potentially disrupt normal neural processes. This is especially important given the critical periods of brain development during pregnancy.
Potential Effects of Tylenol on Fetal Brain Development
Tylenol, while commonly used for pain relief, may exert subtle yet significant effects on the developing fetal brain. It is crucial to acknowledge that the exact nature of these effects is still being investigated. However, research suggests potential interference with neurotransmitter systems and the intricate processes of synaptogenesis and myelination. These are essential steps in establishing normal brain circuitry and function.
Role of Genetic Predisposition and Environmental Factors
The development of ASD and ADHD is a complex interplay of genetic predisposition and environmental factors. While specific genes have been associated with these conditions, environmental factors can significantly modulate their expression. This suggests that even subtle environmental exposures, like Tylenol use during pregnancy, could potentially exacerbate a predisposition or trigger the onset of these conditions in genetically susceptible individuals.
Comparison with Other Environmental Risk Factors
Various environmental factors have been linked to an increased risk of ASD and ADHD. These include exposure to certain toxins, infections during pregnancy, and other medications. Comparing the potential impact of Tylenol use to these other factors is important to understand the relative contribution of each. Ultimately, this will require further research.
Neurobiological Pathways Potentially Affected
The developing fetal brain possesses complex neurobiological pathways that are crucial for various cognitive functions. These pathways are particularly vulnerable to disruptions during critical periods of development. Potential disruptions include interference with dopamine, serotonin, and glutamate systems, which play vital roles in regulating mood, attention, and other essential functions.
Potential Pathways and Biological Processes
| Potential Pathway | Biological Process | Possible Impact on Fetal Development |
|---|---|---|
| Interference with neurotransmitter systems (e.g., dopamine, serotonin) | Disruption of neurotransmission, leading to altered neuronal signaling and connectivity. | Potentially impacting attention, mood regulation, and social interaction. |
| Impairment of synaptogenesis and myelination | Reduced formation and maturation of synapses and myelin sheaths. | Potential for deficits in neural circuit formation and communication. |
| Inflammation or oxidative stress | Elevated inflammatory responses or oxidative stress. | Possible disruption of cellular processes and neuronal damage. |
| Epigenetic modifications | Changes in gene expression without altering the underlying DNA sequence. | Long-term consequences on brain development and function. |
Alternative Explanations and Considerations
The observed correlations between Tylenol use during pregnancy and an increased risk of ASD/ADHD are intriguing, but we must critically examine potential alternative explanations to avoid jumping to conclusions. Simply observing a correlation does not prove causation. There are several factors that might be influencing the results, which we need to consider before drawing definitive conclusions.Existing research often faces challenges in isolating the precise impact of Tylenol use from other contributing factors.
This necessitates a careful evaluation of confounding variables and limitations in study design to ascertain the true nature of the relationship. Understanding potential biases is crucial for interpreting the findings correctly and guiding future research.
Recent studies suggest a potential link between using Tylenol during pregnancy and an increased risk of ASD and ADHD in children. It’s fascinating how these seemingly small choices can have such significant downstream effects. While researching this, I stumbled across a fascinating Twitter thread discussing Lady Gaga’s fibromyalgia diagnosis, which prompted me to think about the complex interplay of health and societal perception, particularly when it comes to women’s health.
This brings me back to the initial topic – the potential correlation between Tylenol use in pregnancy and developmental conditions like ASD and ADHD – highlighting the need for continued research in this area. Ultimately, more investigation is required to fully understand these connections. lady gaga fibromyalgia twitter diagnosis
Confounding Factors in Existing Studies
A multitude of factors can influence the observed correlation, making it difficult to determine if Tylenol use is truly a causal factor. These factors, often intertwined, can obscure the relationship between Tylenol use and ASD/ADHD risk.
- Socioeconomic status: Families with lower socioeconomic status may have limited access to prenatal care, leading to both higher rates of Tylenol use and poorer health outcomes, including a higher incidence of developmental conditions. This could be mistakenly interpreted as a direct link between Tylenol and the conditions.
- Maternal health conditions: Pregnant women with certain health conditions may be more likely to use Tylenol and also have a higher risk of having a child with ASD/ADHD. Conditions such as pre-existing anxiety or depression, or other underlying medical issues, can confound the analysis.
- Medication use during pregnancy: Mothers taking other medications, either prescribed or over-the-counter, could potentially influence both Tylenol use and the risk of ASD/ADHD. This necessitates controlling for a broader range of medications in study design.
- Exposure to environmental toxins: Prenatal exposure to environmental toxins or pollutants can affect neurodevelopment and potentially increase the risk of ASD/ADHD. This could be correlated with Tylenol use if, for example, families in certain environments or with specific lifestyles are more prone to both Tylenol use and exposure to toxins.
- Stress and lifestyle factors: Stressful life events, dietary habits, and overall lifestyle choices can affect both the mother’s health and the child’s development. These factors could be intertwined with Tylenol use, potentially creating a spurious correlation.
Limitations in Study Design
The design of many studies investigating this correlation can introduce significant limitations.
- Retrospective studies: Retrospective studies, relying on past medical records, can suffer from recall bias. Mothers may inaccurately remember their Tylenol use, potentially leading to skewed results.
- Lack of large sample sizes: Smaller sample sizes may not adequately reflect the diverse population and can lead to less reliable statistical significance in findings.
- Inconsistent methodologies: Different studies often employ varying criteria for diagnosing ASD/ADHD and assessing Tylenol use. This variability makes it challenging to compare and consolidate results across research.
- Correlation versus causation: Observational studies can only establish correlations, not causal links. Further research using more robust methodologies, like randomized controlled trials (RCTs), is needed to establish a cause-and-effect relationship.
Addressing Potential Biases, Using tylenol during pregnancy associated with increased risk of asd adhd
Bias in studies can significantly skew the results. Researchers must actively mitigate potential biases to ensure accurate interpretation of data.
- Minimizing recall bias: Using prospective studies where data is collected throughout pregnancy can help minimize recall bias. This involves tracking Tylenol use and other relevant factors concurrently.
- Standardizing diagnostic criteria: Using consistent and standardized diagnostic criteria for ASD/ADHD across studies can improve the reliability and comparability of findings.
- Controlling for confounding factors: Statistical methods can be employed to control for potential confounding factors like socioeconomic status, maternal health conditions, and other medications.
Table of Potential Confounding Factors
| Potential Confounding Factor | Possible Influence on Observed Correlation |
|---|---|
| Socioeconomic status | Lower socioeconomic status may be associated with both higher Tylenol use and increased risk of developmental conditions. |
| Maternal health conditions | Certain maternal health conditions may increase both Tylenol use and the risk of ASD/ADHD. |
| Other medication use | Co-administration of other medications can influence both Tylenol use and the risk of ASD/ADHD. |
| Environmental exposures | Exposure to toxins or pollutants could be correlated with both Tylenol use and the risk of developmental conditions. |
| Stress and lifestyle factors | Stressful life events and lifestyle choices can affect both maternal health and child development, potentially creating a spurious correlation with Tylenol use. |
Recommendations and Future Directions: Using Tylenol During Pregnancy Associated With Increased Risk Of Asd Adhd
Navigating the potential link between acetaminophen (Tylenol) use during pregnancy and the risk of ASD/ADHD requires careful consideration and a proactive approach. The current research suggests a possible association, but definitive proof is still needed. This necessitates a multifaceted strategy encompassing further research, practical guidelines for pregnant women and healthcare professionals, and mitigation strategies to potentially minimize risk.The observed association between Tylenol use during pregnancy and potential ASD/ADHD risk demands a robust response.
Recent studies suggest a possible link between using Tylenol during pregnancy and an increased risk of ASD and ADHD in children. This raises important questions about the medications we take while pregnant, and the potential impact on developing fetuses. Similar concerns have been raised about the use of common mood stabilizing drugs, which, according to this article on common mood stabilizing drug can increase risk of birth defects , can also increase the risk of birth defects.
This further highlights the need for careful consideration and consultation with healthcare professionals before taking any medication during pregnancy.
This includes meticulous research designs, large-scale studies, and a commitment to understanding the intricate mechanisms involved.
Recommendations for Further Research
A critical need exists for rigorous, well-controlled studies to confirm or refute the observed association. Such studies should incorporate a variety of methodologies, including:
- Longitudinal studies: Tracking the use of acetaminophen during pregnancy and the development of ASD/ADHD symptoms in children throughout their childhood. These studies are crucial for establishing temporal relationships and identifying potential dose-response effects. For example, a longitudinal study might examine the impact of varying acetaminophen dosages during pregnancy on the incidence of ASD/ADHD symptoms in the offspring.
- Large-scale cohort studies: Analyzing data from large populations of pregnant women and their children. These studies would allow for a broader assessment of the potential association, controlling for confounding factors such as socioeconomic status, pre-existing conditions, and other medications. For example, a large-scale cohort study could compare the rates of ASD/ADHD in children born to mothers who took acetaminophen regularly during pregnancy to those who did not.
- Mechanism-based research: Investigating the potential biological mechanisms linking acetaminophen use during pregnancy to ASD/ADHD. Understanding the pathways through which acetaminophen might impact fetal development could lead to more targeted interventions and preventive strategies. For example, research could focus on how acetaminophen affects neurotransmitter systems or placental function.
Recommendations for Pregnant Women and Healthcare Providers
Providing clear, evidence-based information to pregnant women is paramount. Healthcare providers should be equipped to discuss the potential risks and benefits of acetaminophen use during pregnancy, offering alternative pain management options where appropriate.
- Patient education: Educating pregnant women about the potential link between acetaminophen use and ASD/ADHD risk, encouraging them to discuss their concerns with their healthcare providers. This should be framed as potential risk, not certainty. For example, informing expectant mothers about the importance of consulting with their doctors about pain management strategies and the potential need to avoid unnecessary acetaminophen use.
Recent studies suggest a link between using Tylenol during pregnancy and an increased risk of ASD and ADHD in children. While this is concerning, it’s important to remember that financial stress can significantly impact sleep quality, which in turn can affect overall health. Learning how to manage financial stress, such as by exploring strategies like budgeting and debt management, is crucial for a healthy pregnancy and overall well-being.
This includes looking into resources like how financial stress affects sleep and what you can do about it. So, while the potential risks of Tylenol use remain a concern, a balanced approach that addresses all aspects of well-being is key.
- Alternative pain management strategies: Encouraging pregnant women to explore alternative pain relief methods, such as over-the-counter remedies without acetaminophen, or other strategies like relaxation techniques and support groups. This should be done in consultation with a healthcare professional. For example, recommending heat packs, gentle stretching, or other non-pharmacological methods to manage common pregnancy-related discomfort.
- Regular prenatal care: Emphasizing the importance of regular prenatal check-ups to monitor fetal development and address any concerns. This is critical to identify any potential issues early on. For example, regular check-ups provide opportunities for the healthcare provider to discuss the mother’s use of acetaminophen and to adjust recommendations based on individual circumstances.
Strategies for Mitigating Potential Risk
While definitive answers regarding the potential link are still emerging, some strategies can potentially help minimize any potential risk.
- Responsible use of acetaminophen: Encouraging pregnant women to only use acetaminophen when necessary and in accordance with the recommended dosage. For example, adhering to the recommended dosage on the product label and consulting a doctor for any concerns.
- Exploration of alternative therapies: Promoting research and development of alternative therapies for managing pain during pregnancy. For example, supporting studies exploring the efficacy of non-pharmacological pain management techniques.
Importance of Patient Education and Awareness
Clear communication between healthcare providers and pregnant women is crucial. Understanding the potential link, even if tentative, allows for informed decisions and reduces anxiety.
- Open communication: Promoting open and honest dialogue between pregnant women and healthcare providers about acetaminophen use and potential risks. For example, facilitating discussions that allow the mother to express concerns and understand the available options.
- Accurate information dissemination: Providing accurate and accessible information about the potential link to the general public, helping to avoid misinformation. For example, providing reliable sources of information on reputable websites and through educational programs.
Key Recommendations and Future Research Directions
| Area | Recommendations | Future Research Directions |
|---|---|---|
| Research | Longitudinal and large-scale cohort studies | Mechanism-based research to understand biological pathways |
| Patient Care | Patient education and alternative pain management strategies | Enhancing communication and access to accurate information |
| Risk Mitigation | Responsible use of acetaminophen, exploration of alternative therapies | Development of targeted strategies based on research findings |
Conclusion
The potential link between acetaminophen (Tylenol) use during pregnancy and an increased risk of autism spectrum disorder (ASD) and attention-deficit/hyperactivity disorder (ADHD) remains a complex and intriguing area of research. While several studies have suggested a correlation, definitive proof of a causal relationship is still lacking. This uncertainty underscores the need for continued investigation and responsible decision-making for both expectant mothers and healthcare providers.
Current Understanding of the Correlation
Current research indicates a potential association between Tylenol use during pregnancy and an elevated risk of ASD and ADHD. However, these studies often present observational data, meaning they identify correlations but cannot definitively prove causation. Confounding factors, such as socioeconomic status, environmental exposures, and other lifestyle choices, can influence both Tylenol use and the development of these conditions.
Consequently, it is crucial to acknowledge the limitations of current research and avoid drawing firm conclusions about a direct cause-and-effect relationship.
Importance of Further Research
To truly understand the potential impact of Tylenol use during pregnancy on neurodevelopmental outcomes, more robust and conclusive research is required. Well-designed, large-scale, and prospective studies are needed to control for confounding variables and track the long-term effects of Tylenol exposure. These studies should incorporate detailed information about the timing, frequency, and dosage of Tylenol use during pregnancy, alongside comprehensive assessments of the child’s neurodevelopment.
This rigorous methodology is essential to differentiate between correlation and causation.
Cautious Decision-Making for Pregnant Women and Healthcare Providers
In the absence of definitive proof of a causal link, pregnant women and healthcare providers should adopt a cautious approach. This involves careful consideration of the potential risks and benefits of Tylenol use. Healthcare providers should discuss the potential risks and benefits with their patients, considering individual circumstances and medical histories. This open communication is paramount for informed decision-making and should include the option for alternative pain relief strategies when possible.
Implications of the Findings
The ongoing investigation into the potential link between Tylenol use and neurodevelopmental disorders highlights the need for ongoing awareness and research. The implications extend beyond individual cases to the broader field of public health. Further research is crucial to provide clearer guidance for pregnant women and healthcare providers, ultimately aiming to reduce potential risks and promote optimal neurodevelopmental outcomes for children.
Last Point
In conclusion, the potential link between Tylenol use during pregnancy and an increased risk of ASD/ADHD warrants further investigation. While the current research raises concerns, it doesn’t definitively prove causation. More robust, large-scale studies are needed to confirm or refute this association. In the meantime, expectant mothers should discuss any concerns about medication use with their healthcare providers to make informed decisions about their prenatal care.
Ultimately, responsible decision-making and ongoing research are crucial in navigating this complex issue.