Vaccine preventable diseases are on the rise what to know. This alarming trend highlights a critical need for understanding the factors driving this resurgence and the steps we can take to mitigate its impact. Decreased vaccination rates, the spread of misinformation, and accessibility issues are all contributing to this concerning increase. This blog post will delve into the complexities of this public health crisis, examining specific diseases experiencing resurgences, exploring public health strategies, addressing misinformation, and considering the global and long-term implications.
We’ll explore the specific details of measles outbreaks, the recent resurgence of whooping cough, and the long-term effects of preventable diseases like polio. We’ll also discuss the public health measures being implemented, the role of healthcare providers, and effective communication strategies to promote vaccination. This is a critical time to arm ourselves with knowledge and take action to protect ourselves and our communities.
Understanding the Trend
The resurgence of vaccine-preventable diseases is a concerning global health issue. This trend demands our attention and necessitates a deeper understanding of the contributing factors. The consequences for public health are significant, highlighting the importance of maintaining high vaccination coverage.The increasing incidence of vaccine-preventable diseases is not a new phenomenon. Historical patterns show a cyclical relationship between vaccination rates and disease outbreaks.
A drop in vaccination rates, whether due to misinformation, accessibility issues, or other factors, invariably leads to a rise in the number of cases. This underscores the critical link between vaccination and public health.
Factors Contributing to the Increase
Several factors contribute to the rise in vaccine-preventable diseases. Decreased vaccination rates are a primary driver, often fueled by misinformation and hesitancy. This can manifest in various forms, such as reluctance to vaccinate children, or skepticism about the efficacy and safety of vaccines. Furthermore, accessibility issues, such as limited access to healthcare services, particularly in underserved communities, can also hinder vaccination efforts.
These factors are not isolated occurrences; they often intertwine and exacerbate the problem.
Impact on Public Health
The resurgence of vaccine-preventable diseases has a profound impact on public health. Increased hospitalizations and deaths are common outcomes. The strain on healthcare systems can be substantial, diverting resources from other critical health needs. Moreover, outbreaks can lead to economic losses due to lost productivity and increased healthcare costs. This impact underscores the need for proactive measures to address the issue.
Examples of Resurging Diseases
Measles, pertussis (whooping cough), and polio are among the diseases experiencing resurgence in various parts of the world. The resurgence of these diseases is a clear indication of the consequences of declining vaccination rates. These outbreaks can have severe implications for individuals, families, and communities.
It’s alarming how vaccine-preventable diseases are surging. Making sure kids are up-to-date on their shots is crucial, but sometimes, getting them to eat healthy foods can be a challenge. For parents facing picky eaters, picky eating advice on what parents should do offers helpful strategies to navigate this common hurdle. Ultimately, healthy eating habits and vaccinations are both vital to bolstering a child’s overall well-being, and protecting them from preventable illnesses.
Vaccination Rates Over Time and Regions
Vaccination rates vary significantly across different regions and over time. Data from the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) provides valuable insights into these trends. Significant fluctuations can be observed, often reflecting the effectiveness of vaccination programs, public health campaigns, and the impact of factors like misinformation and accessibility.
| Region | Year | Vaccination Rate (%) |
|---|---|---|
| North America | 2010 | 90 |
| North America | 2020 | 85 |
| Sub-Saharan Africa | 2010 | 70 |
| Sub-Saharan Africa | 2020 | 65 |
The table above presents a simplified illustration. Comprehensive data requires a deeper analysis and consideration of various factors. More detailed information on vaccination rates can be found on the WHO and CDC websites.
Examining Specific Diseases
The resurgence of vaccine-preventable diseases demands a closer look at the specific illnesses driving this troubling trend. Understanding the details of outbreaks, including transmission patterns, long-term effects, and vulnerable populations, is crucial for developing effective strategies to mitigate their impact. This examination focuses on measles, whooping cough, and polio, highlighting the severity and complexities of each.
Measles Outbreaks: Severity and Transmission
Measles, a highly contagious viral illness, poses a significant public health threat. Its characteristic symptoms, including fever, cough, runny nose, and a distinctive rash, can lead to severe complications, such as pneumonia, encephalitis (inflammation of the brain), and even death. Transmission occurs primarily through direct contact with respiratory droplets from an infected individual, emphasizing the importance of proper hygiene and vaccination.
With vaccine-preventable diseases on the rise, it’s important to understand what precautions we should take. As we move past the Omicron wave, the potential for resurgence of other illnesses, like measles and whooping cough, is something we need to be mindful of. Understanding what happens after the Omicron wave passes is crucial to anticipating potential health challenges.
Check out this article to learn more about the long-term implications of the wave what happens after the omicron wave passes. Ultimately, staying informed about vaccination schedules and potential outbreaks is key to preventing the resurgence of these diseases.
Outbreaks often occur in communities with low vaccination rates, highlighting the critical role vaccination plays in preventing widespread transmission. The severity of measles outbreaks varies, depending on factors like the population’s overall health and the presence of underlying conditions.
Whooping Cough Resurgence: Contributing Factors
The recent resurgence of whooping cough, or pertussis, underscores the importance of maintaining vaccination schedules. This highly contagious bacterial infection primarily affects infants and young children, manifesting with severe coughing fits, often followed by a “whooping” sound. Factors contributing to the resurgence include waning immunity in previously vaccinated individuals, decreasing vaccination rates in some populations, and the potential for antibiotic resistance in some strains.
These factors highlight the need for ongoing vaccination efforts and public health campaigns to address this resurgence effectively.
Long-Term Effects of Polio: Impact on Individuals and Communities
Polio, a crippling disease caused by a virus, can result in long-term disabilities. Paralysis, muscle weakness, and breathing difficulties are potential consequences. The long-term effects can significantly impact individuals’ quality of life, affecting their ability to work, participate in social activities, and maintain their independence. Polio’s impact on communities extends beyond individual suffering; it can lead to economic hardship and strain healthcare systems.
Communities with high rates of polio cases often experience decreased productivity and increased healthcare costs. A notable example is the lasting impact on communities in the past, where polio outbreaks led to significant social and economic challenges.
Vulnerable Populations at Risk
Certain populations are disproportionately vulnerable to vaccine-preventable diseases. Infants and young children, who have not yet developed full immunity, are at high risk. Individuals with weakened immune systems, such as those undergoing chemotherapy or with certain chronic illnesses, are also particularly susceptible. Furthermore, marginalized communities, often facing socioeconomic disparities and limited access to healthcare, may experience higher rates of infection.
This vulnerability highlights the importance of equitable access to vaccination programs.
It’s concerning how vaccine-preventable diseases are making a comeback. Understanding the reasons behind this rise is crucial. This often involves looking at factors like vaccination hesitancy and the spread of misinformation, much like the recent controversies surrounding performance-enhancing drugs in sports, such as the Olympic figure skating scandal involving a banned drug. This recent scandal highlights the importance of responsible drug use and adherence to rules.
Ultimately, staying informed about preventable diseases is key to protecting public health.
Regional Outbreak Severity and Socioeconomic Factors
The severity of outbreaks can vary considerably across different regions, influenced by socioeconomic factors. Areas with limited access to healthcare, inadequate sanitation, and lower vaccination rates tend to experience more severe outbreaks. For instance, a region with a weaker healthcare infrastructure might struggle to contain an outbreak effectively, leading to a higher number of cases and complications. In contrast, regions with robust healthcare systems and high vaccination coverage often experience milder outbreaks.
These differences highlight the need for tailored interventions and targeted vaccination campaigns based on regional socioeconomic realities.
Public Health Strategies: Vaccine Preventable Diseases Are On The Rise What To Know
Combating the resurgence of vaccine-preventable diseases necessitates a multifaceted approach encompassing robust public health measures, targeted communication, and equitable access. These strategies must address the root causes of vaccine hesitancy and ensure that all communities have access to the life-saving protection vaccines provide. Effective implementation of these strategies is crucial to curtailing the increasing trend and safeguarding public health.Public health strategies play a pivotal role in mitigating the rising incidence of vaccine-preventable diseases.
These strategies encompass various components, from implementing effective communication campaigns to improving access to vaccines in underserved communities. By understanding and addressing the specific challenges faced by different populations, we can effectively enhance vaccination rates and bolster community immunity.
Public Health Measures to Address the Rise
A comprehensive approach to tackling the rise in vaccine-preventable diseases involves several key public health measures. These measures include strengthening surveillance systems to identify outbreaks promptly, implementing targeted vaccination campaigns, and bolstering public health infrastructure. Effective communication and education campaigns play a vital role in changing attitudes and promoting vaccination.
- Strengthening Surveillance Systems: Real-time monitoring of disease incidence allows for rapid response to outbreaks, enabling prompt interventions and preventing further spread. Early detection through robust surveillance systems is critical to controlling outbreaks effectively and minimizing their impact.
- Targeted Vaccination Campaigns: Tailoring vaccination campaigns to specific populations and communities with low vaccination rates can significantly increase immunization coverage. These campaigns must consider the cultural and social factors influencing vaccination decisions in different communities. Identifying and addressing specific concerns or misinformation is essential to maximizing the impact of vaccination campaigns.
- Boosting Public Health Infrastructure: Sufficient resources and trained personnel are essential to support vaccination efforts. Adequate funding for public health programs, including outreach, education, and vaccination clinics, is crucial to effective implementation.
Effective Communication Strategies for Promoting Vaccination
Effective communication plays a vital role in promoting vaccination. These strategies should emphasize the benefits of vaccination while addressing concerns and misconceptions surrounding vaccines. Transparency, clear information, and engagement are key elements of successful communication.
- Addressing Concerns and Misconceptions: Open dialogue and evidence-based information can address vaccine hesitancy. Actively listening to and responding to concerns with factual data and trusted sources can build trust and encourage vaccination.
- Utilizing Trusted Channels: Leveraging community leaders, healthcare providers, and social media platforms to disseminate information can improve vaccine uptake. Emphasizing the benefits of vaccination through trusted channels, while addressing concerns and misconceptions, is crucial for successful communication campaigns.
- Tailoring Messages to Different Audiences: Messages must be adapted to resonate with various cultural backgrounds and demographics. Effective communication campaigns must consider the specific needs and concerns of different communities.
Strategies for Improving Vaccination Access in Underserved Communities
Improving access to vaccination for underserved communities is essential to achieving equitable protection against vaccine-preventable diseases. These strategies must address the barriers to access faced by these communities.
- Targeted Outreach Programs: Developing targeted outreach programs to underserved communities can ensure that individuals have access to vaccination services. Community engagement and culturally appropriate outreach methods are essential for improving vaccination rates in underserved areas.
- Mobile Vaccination Clinics: Mobile clinics can bring vaccination services directly to remote or underserved areas. Making vaccination services more accessible through mobile clinics can significantly improve vaccination rates in these populations.
- Addressing Socioeconomic Barriers: Financial constraints and transportation difficulties can hinder access to vaccination services. Addressing these barriers by providing financial assistance and transportation options can improve vaccine uptake in underserved communities.
The Role of Healthcare Providers in Educating Patients, Vaccine preventable diseases are on the rise what to know
Healthcare providers play a crucial role in educating patients about the importance of vaccines. Building trust and providing accurate information are vital aspects of their role.
- Building Trust and Open Communication: Creating a supportive environment for open communication between healthcare providers and patients fosters trust. This trust can lead to improved vaccination rates and increased confidence in the safety and efficacy of vaccines.
- Providing Accurate Information: Healthcare providers should be well-informed about vaccines and their safety profiles. Delivering accurate information to patients can effectively address concerns and dispel misinformation.
- Addressing Individual Concerns: Healthcare providers should be prepared to address any concerns or questions patients may have about vaccines. Open dialogue can alleviate anxieties and encourage vaccination.
Examples of Successful Vaccination Campaigns
Successful vaccination campaigns have demonstrated the effectiveness of these strategies. These campaigns showcase the impact of targeted outreach, clear communication, and robust public health measures.
- Measles Eradication Campaigns: Global efforts to eradicate measles highlight the success of large-scale vaccination campaigns. The elimination of measles in many countries demonstrates the power of consistent vaccination efforts.
- Polio Eradication Initiatives: Polio eradication initiatives exemplify the importance of sustained efforts and targeted outreach to achieve widespread vaccination. These campaigns have demonstrated the impact of global collaboration and sustained community engagement.
Misinformation and Public Perception
The rise of vaccine-preventable diseases is unfortunately intertwined with the spread of misinformation. This fabricated information, often amplified by social media, significantly impacts public perception and, consequently, vaccination rates. Understanding the factors behind this phenomenon and developing effective countermeasures are crucial to protecting public health.The spread of misinformation, particularly regarding vaccines, has a profound impact on individual decisions.
This can range from hesitancy to outright refusal, leading to preventable outbreaks and endangering vulnerable populations. It is imperative that public health officials and communicators understand the mechanisms of misinformation and implement strategies to combat its detrimental effects.
The Role of Misinformation in Vaccine Hesitancy
Misinformation regarding vaccines often centers on unsubstantiated claims of adverse effects, spurious correlations, and distrust in institutions. This fabricated information can create an environment of fear and uncertainty, ultimately leading to vaccine hesitancy. For instance, false claims of autism links to vaccines, despite extensive scientific studies disproving such connections, have had a significant impact on vaccination rates in some regions.
Impact of Social Media on Public Perception
Social media platforms, while valuable tools for communication, can also be breeding grounds for the rapid spread of misinformation. The algorithms of these platforms often prioritize engagement, which can inadvertently amplify false narratives and make them more accessible to susceptible individuals. The rapid dissemination of misleading information can shape public perception and create an environment where trust in established scientific consensus is undermined.
Strategies for Countering Vaccine Misinformation
Effective strategies to combat misinformation require a multi-faceted approach. This includes fact-checking, providing clear and accessible information, and engaging with those who spread misinformation in a constructive manner. Furthermore, emphasizing the safety and efficacy of vaccines through transparent and credible channels is crucial.
Effectiveness of Communication Approaches
Different communication approaches can have varying degrees of effectiveness in addressing vaccine hesitancy. Approaches that focus on building trust and rapport, addressing concerns directly, and providing accurate scientific information are often more successful than those that rely solely on scare tactics or accusations. These effective approaches are based on building a genuine connection with the audience and emphasizing the positive aspects of vaccination.
Key Sources of Misinformation and Debunking Methods
Identifying and debunking the sources of misinformation is essential for combating its spread. This often includes examining the origins of false claims and scrutinizing the credentials of individuals or groups disseminating misleading information. Reputable scientific organizations, medical professionals, and government health agencies play a crucial role in providing accurate and trustworthy information. By proactively addressing the concerns of vaccine hesitant individuals and promoting factual information through trusted channels, we can help mitigate the impact of misinformation and foster informed decisions about vaccination.
Global Perspective
The rising tide of vaccine-preventable diseases isn’t confined to any single nation. It’s a global challenge demanding a comprehensive understanding of the disparities and collaborative efforts needed to stem the tide. A global perspective reveals complex factors influencing vaccination rates and disease prevalence, highlighting the interconnectedness of health across borders.International collaborations are crucial in addressing these challenges, extending beyond individual country initiatives.
Effective strategies require a shared commitment to vaccine development, equitable distribution, and robust public health infrastructure, which are not limited to one country’s borders. This shared responsibility underscores the importance of global health organizations and initiatives in coordinating efforts to achieve universal health coverage.
Vaccination Rates and Disease Prevalence Comparisons
Vaccination rates and disease prevalence vary significantly across countries. Factors such as socioeconomic status, access to healthcare, and public health infrastructure play a role in these disparities. Understanding these variations is critical for developing targeted interventions.
International Collaborations in Vaccine Development and Distribution
International collaborations are vital for accelerating vaccine development and ensuring equitable distribution. These partnerships facilitate knowledge sharing, resource pooling, and coordinated efforts to address emerging threats. Examples include initiatives involving pharmaceutical companies, research institutions, and global health organizations.
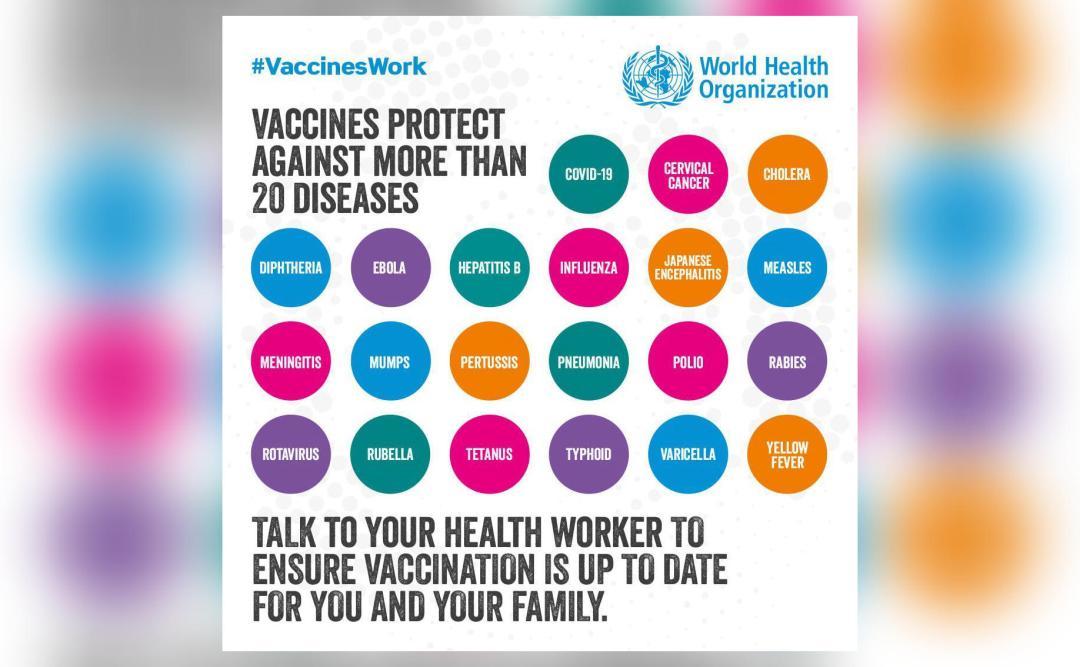
Role of Global Health Organizations in Addressing Vaccine-Preventable Diseases
Global health organizations, such as the World Health Organization (WHO), play a pivotal role in coordinating efforts to combat vaccine-preventable diseases. Their activities encompass surveillance, data collection, technical support to countries, and advocacy for improved vaccination programs.
Vaccine Coverage Disparities Globally
Significant disparities exist in vaccine coverage across different regions and populations globally. Factors such as poverty, conflict, and limited access to healthcare contribute to these inequalities. Data on these disparities are crucial for targeting resources and developing effective interventions. For instance, some regions may have lower vaccination rates due to limited access to healthcare facilities or transportation, hindering the timely administration of vaccinations.
Examples of Successful Global Initiatives to Improve Vaccination Rates
Several global initiatives have successfully improved vaccination rates, demonstrating the efficacy of targeted strategies. These initiatives often involve community engagement, education campaigns, and strengthening healthcare infrastructure. For example, the Gavi, the Vaccine Alliance, has played a crucial role in increasing vaccine access in developing countries, saving millions of lives.
Long-Term Impacts
The resurgence of vaccine-preventable diseases has profound and far-reaching consequences extending far beyond immediate health concerns. These diseases impose a significant economic burden on healthcare systems, disrupt social structures, and inflict substantial societal costs. Understanding these long-term impacts is crucial for developing effective prevention and mitigation strategies.The financial and social consequences of preventable illnesses are often underestimated. Beyond the direct costs of treatment, these diseases have ripple effects impacting productivity, education, and community well-being.
Proactive measures, such as vaccination campaigns and public health initiatives, are not just about individual health; they safeguard the collective well-being of communities and nations.
Economic Burden on Healthcare Systems
The increasing incidence of vaccine-preventable diseases places a substantial strain on healthcare resources. Treatment costs, including hospitalization, intensive care, and long-term rehabilitation, can escalate dramatically. This strain is particularly pronounced in resource-limited settings where healthcare infrastructure may not be equipped to handle surges in cases. For instance, outbreaks of measles can overwhelm hospitals, leading to delays in treatment for other critical illnesses.
Social Impact on Individuals and Communities
Vaccine-preventable diseases can inflict profound social impacts on individuals and communities. Long-term health complications can lead to disability, reduced quality of life, and diminished opportunities for education and employment. These diseases can also create social stigma and discrimination, isolating affected individuals and families. The psychological toll on families grappling with the illness and its aftermath is also substantial.
For example, the social isolation and reduced educational opportunities experienced by children with polio can have lasting repercussions.
Societal Costs
The societal costs associated with vaccine-preventable diseases extend beyond direct healthcare expenses. Lost productivity due to illness and disability represents a significant economic loss to individuals, families, and the broader economy. Furthermore, the need for increased healthcare expenses and social support services, such as home healthcare and disability assistance, adds further to the overall societal burden. Measles outbreaks, for example, can lead to widespread school closures, impacting the education of countless children and disrupting community activities.
Potential Long-Term Health Consequences
Certain vaccine-preventable diseases can result in long-term health complications, impacting individuals’ well-being and quality of life. These consequences can include neurological impairments, organ damage, and chronic health conditions. For example, individuals who contract rubella during pregnancy may experience adverse outcomes for the developing fetus. The long-term effects can be debilitating, requiring ongoing medical care and support.
Comparison of Costs
| Category | Cost of Treating Vaccine-Preventable Disease | Cost of Vaccination Programs |
|---|---|---|
| Direct Healthcare Costs (hospitalization, medication, etc.) | High, potentially escalating with severity and duration of illness | Relatively low, spread over a large population |
| Lost Productivity (school, work absences) | Significant, impacting individual and national economies | Minimal, focused on preventing disease occurrence |
| Long-term Care Costs (rehabilitation, disability assistance) | Potentially substantial, especially for severe cases | Insignificant, averted by preventing disease onset |
| Indirect Costs (social support, stigma) | Substantial, impacting social fabric and individual well-being | Minimal, fostering healthy communities |
| Public Health Costs (outbreak response, surveillance) | High during outbreaks | Low, focused on prevention |
The cost of preventing a vaccine-preventable disease is significantly lower than the cost of treating the disease itself. Investing in vaccination programs is a cost-effective strategy for safeguarding public health and mitigating long-term societal impacts.
Future Implications
The resurgence of vaccine-preventable diseases underscores the critical need for proactive measures to safeguard global health in the future. Predicting future trends requires careful consideration of evolving factors, including emerging infectious diseases, the impact of climate change, and the ever-present threat of vaccine hesitancy. Understanding these potential challenges is crucial for developing effective strategies to prevent future outbreaks.
Predicting Future Trends in Vaccine-Preventable Diseases
Future trends in vaccine-preventable diseases will likely be shaped by several interconnected factors. Antimicrobial resistance, a growing concern, could lead to the emergence of drug-resistant strains of existing pathogens, making current vaccines less effective. Climate change may alter the geographical distribution of disease vectors, potentially expanding the range of diseases and increasing their transmission rates. Increased global travel and interconnectedness facilitate the rapid spread of infectious agents across continents.
Potential Impact of Emerging Diseases on Global Health
The emergence of novel pathogens poses a significant threat to global health. The emergence of previously unknown viruses or bacteria, potentially zoonotic in origin, could lead to pandemics with devastating consequences. The 2009 H1N1 influenza pandemic, for example, highlighted the vulnerability of populations to novel pathogens. The rapid development and deployment of vaccines, coupled with robust public health infrastructure, are essential to mitigate the impact of such outbreaks.
Strategies to Prevent the Spread of New Vaccine-Preventable Diseases
A proactive approach to preventing the spread of new vaccine-preventable diseases hinges on a multi-faceted strategy. This includes strengthening global surveillance systems to quickly identify emerging threats. International collaboration and data sharing are crucial for responding to emerging outbreaks effectively. Investment in research and development for new vaccines and preventative measures is essential. Early detection and rapid response protocols should be implemented.
Importance of Ongoing Research in Vaccine Development and Prevention Strategies
Continued research in vaccine development and prevention strategies is paramount. This includes developing vaccines for emerging pathogens, refining existing vaccine formulations to enhance efficacy, and investigating new delivery methods for vaccines. Investing in research to better understand the immune response to various pathogens will also lead to the development of more effective preventive measures. The development of new diagnostic tools and therapies for treating infections is equally important.
Potential Impact of Different Preventative Strategies on Future Disease Prevalence
| Preventative Strategy | Potential Impact on Future Disease Prevalence | Examples |
|---|---|---|
| Improved global surveillance and early detection | Reduced disease transmission time and potential severity of outbreaks. | Rapid identification and containment of outbreaks through robust surveillance systems. |
| Increased investment in vaccine research and development | Creation of vaccines to address emerging pathogens and improvement in existing vaccines. | Development of new vaccines for influenza, HIV, or emerging viruses, and refinement of existing vaccines to improve effectiveness. |
| Strengthening public health infrastructure | Improved capacity to manage outbreaks and implement public health measures. | Investment in resources for contact tracing, vaccination campaigns, and isolation protocols. |
| Promoting vaccine acceptance and adherence | Increased vaccine coverage and reduced disease incidence. | Public awareness campaigns, targeted education programs, and addressing misinformation surrounding vaccines. |
“Proactive strategies, research investment, and global collaboration are vital to mitigating the future threat of vaccine-preventable diseases.”
Closing Summary
In conclusion, the rise of vaccine-preventable diseases underscores the importance of vaccination and the urgent need for comprehensive strategies to address this public health crisis. We’ve examined the contributing factors, analyzed specific diseases, and explored public health strategies. Understanding the role of misinformation, the global perspective, and the long-term impacts is essential for developing effective interventions. Ultimately, proactive measures are crucial to prevent future outbreaks and safeguard public health.
By working together, we can reverse this trend and ensure a healthier future for all.