What are the first signs of endometriosis? This deep dive explores the often subtle and sometimes overlooked symptoms, helping you understand the early indicators of this condition. We’ll look at a range of potential signs, from pain and menstrual cycle changes to gastrointestinal issues and pelvic discomfort, and how they can vary from person to person. Understanding these early clues can be crucial for early diagnosis and treatment.
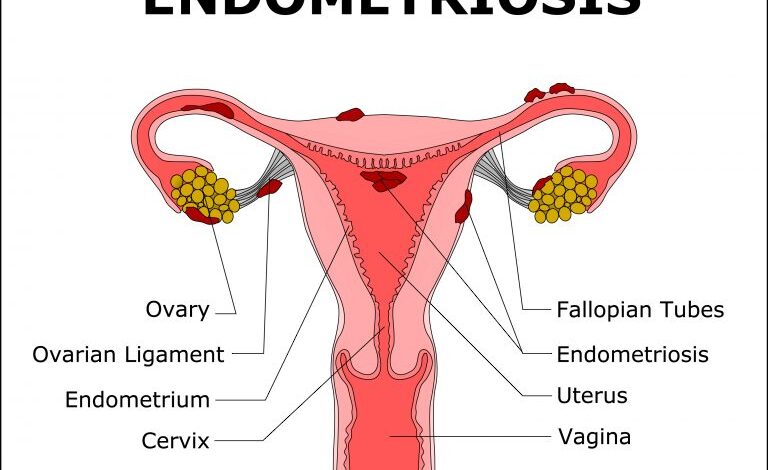
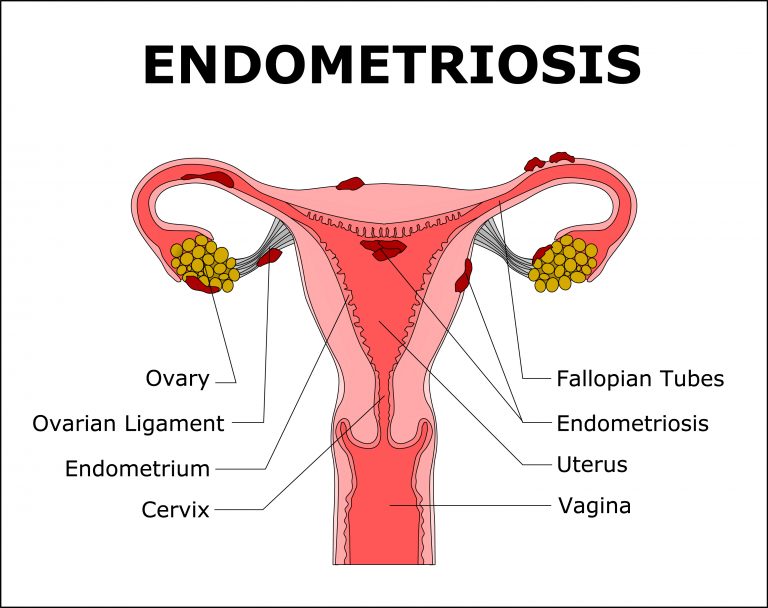
Endometriosis is a condition where tissue similar to the lining of the uterus grows outside of it. This can lead to a wide range of symptoms, many of which are easily misinterpreted as other issues. Early detection is vital, and this article aims to provide a comprehensive overview of the potential early signs to help you recognize the possibility of endometriosis.
Introduction to Endometriosis
Endometriosis is a chronic condition affecting women of reproductive age. It’s characterized by the presence of endometrial-like tissue outside the uterus. This misplaced tissue behaves similarly to normal endometrial tissue, responding to hormonal fluctuations and causing inflammation and pain. Understanding the mechanisms and types of endometriosis is crucial for diagnosis and treatment.The underlying mechanisms of endometriosis are complex and not fully understood.
Current research suggests that a combination of genetic predisposition, hormonal imbalances, immune system dysfunction, and environmental factors may play a role. The abnormal growth of endometrial tissue outside the uterus is thought to occur through various pathways, including retrograde menstruation (the flow of menstrual blood backward into the fallopian tubes), implantation of endometrial cells, and metaplasia (transformation of other tissues into endometrial-like tissue).
Types of Endometriosis
Endometriosis can manifest in various locations throughout the body. The different types are categorized based on their location and characteristics. Understanding these distinctions aids in tailoring treatment plans to the specific needs of each patient.
Classification of Endometriosis Types
| Type | Location | Symptoms | Impact |
|---|---|---|---|
| Peritoneal Endometriosis | The surface of the pelvic organs (ovaries, fallopian tubes, peritoneum) | Pelvic pain, particularly during menstruation, dysmenorrhea, dyspareunia, infertility | Can lead to adhesions, scarring, and chronic pelvic pain. Often the most common type, and frequently presents with a range of symptoms. |
| Ovarian Endometriomas (Endometriomas) | Ovaries | Pelvic pain, often severe and persistent, bloating, heavy bleeding, irregular periods, infertility | Can cause cysts (endometriomas) to form on the ovaries, potentially leading to significant pain and complications. Frequently associated with infertility issues. |
| Deep Infiltrating Endometriosis (DIE) | Deep tissues of the pelvis, including the bowel, bladder, and surrounding tissues | Deep pelvic pain, bowel or bladder dysfunction (e.g., painful bowel movements, painful urination, rectal bleeding), dyspareunia | Can lead to significant and chronic pain, and potentially more complex surgeries. Requires specialized care due to its deeper penetration. |
| Diffuse Peritoneal Endometriosis | Throughout the pelvic cavity and other organs | Diffuse pelvic pain, pain during intercourse, heavy or irregular periods, infertility | Causes a widespread and diffuse inflammatory response, impacting multiple areas. Potentially more challenging to treat due to its extensive nature. |
Early Signs and Symptoms
Navigating the complexities of endometriosis can be challenging, particularly in its early stages. Many women experience a range of symptoms that are often dismissed as normal menstrual discomfort or attributed to other conditions. Understanding these subtle clues is crucial for early diagnosis and effective management.Early endometriosis symptoms often mimic other, more common conditions, making identification difficult. This can lead to delayed diagnosis and treatment, impacting the quality of life for those affected.
It’s important to be aware of the wide spectrum of potential symptoms and to trust your instincts if something feels “off.”
Common Early Symptoms
Early endometriosis symptoms frequently overlap with typical menstrual cramps. This overlap can make it hard to distinguish between the two. Symptoms can include pelvic pain, cramping, and lower back pain, often worsening during menstruation. Some individuals experience painful intercourse (dyspareunia). Furthermore, persistent fatigue and general discomfort are also common early signs.
Subtle and Often Overlooked Symptoms
Beyond the more obvious symptoms, there are often subtle signs that are frequently overlooked. These include unusual digestive issues, such as bloating, constipation, or diarrhea, which can occur around the time of menstruation. Changes in bowel or bladder habits, like increased frequency or urgency, can also be indicators. Additionally, some women experience pain during urination, especially during menstruation.
Comparing Early Endometriosis Symptoms with Other Conditions
Differentiating endometriosis from other conditions can be tricky. For instance, pelvic inflammatory disease (PID) and ovarian cysts can produce similar symptoms. Careful medical history, physical examination, and potentially diagnostic tests are necessary to pinpoint the cause of the symptoms. It’s crucial to consult with a healthcare professional for accurate diagnosis.
Symptom Variability
The experience of endometriosis symptoms varies significantly from person to person. Some women experience intense pain, while others may have milder discomfort. The location and intensity of the pain can also fluctuate. Some individuals might primarily experience digestive issues, while others experience primarily pelvic pain. This variability emphasizes the need for personalized healthcare strategies.
Symptom Severity Table
| Symptom | Frequency | Severity | Impact |
|---|---|---|---|
| Pelvic pain | Often, especially before and during menstruation | Mild to severe, intermittent to constant | Discomfort, difficulty with daily activities, potential for missed work or school |
| Cramping | Often, especially before and during menstruation | Mild to severe | Discomfort, potential for missed work or school |
| Digestive issues (bloating, constipation, diarrhea) | Variable, often around menstruation | Mild to moderate | Discomfort, potential for digestive distress |
| Painful intercourse (dyspareunia) | Variable | Mild to severe | Discomfort during sexual activity, potential for relationship strain |
| Fatigue | Variable, often fluctuating | Mild to severe | Reduced energy levels, difficulty concentrating, impact on daily activities |
Pain as a Leading Indicator
Understanding the pain associated with endometriosis is crucial for early diagnosis and effective management. This chronic condition often presents with a complex array of symptoms, and pain frequently serves as a primary and persistent indicator. Pain can vary significantly from person to person, making recognition challenging.Pain in endometriosis stems from the endometrial tissue growing outside the uterus, which can irritate surrounding tissues, nerves, and organs.
This irritation triggers inflammatory responses and can lead to the release of chemicals that cause pain signals to be transmitted to the brain. The presence of endometriosis lesions in various locations contributes to the diverse pain experiences.
Types of Endometriosis Pain
Endometriosis pain can manifest in different forms, ranging from mild discomfort to severe debilitating agony. This variety of pain experiences highlights the complexity of the condition. The intensity and location of the pain can fluctuate depending on factors like hormonal cycles, stress levels, and physical activity.
Pain Location and Manifestations
Endometriosis pain is not confined to a single area. It can present in several locations, with varying degrees of intensity. Pelvic pain is a common manifestation, often described as cramping, aching, or stabbing. This pain can radiate to the lower back, thighs, or even the rectum.
Pain Intensity and Duration
The intensity of endometriosis pain can range from a mild ache to severe, debilitating cramps. Pain can also fluctuate throughout the menstrual cycle, intensifying during menstruation. Some women experience constant, low-grade pain, while others experience intermittent, sharp pain episodes. The duration of pain episodes can also vary. Some women experience pain for a few hours, while others experience it for days or even weeks.
Impact on Daily Activities
Endometriosis pain can significantly impact a woman’s daily activities. Simple tasks, such as walking, standing, or engaging in physical activity, can become challenging. The pain can interfere with work, school, social activities, and personal relationships. This impact underscores the importance of recognizing and managing the pain effectively.
Categorization of Pain Types
The following table provides a categorization of endometriosis pain types based on location, description, and frequency:
| Pain Type | Location | Description | Frequency |
|---|---|---|---|
| Pelvic Cramps | Pelvic region | Aching, cramping, stabbing pain; often worse during menstruation | Frequent, especially during menses |
| Deep Pelvic Pain | Pelvic region, extending to lower back/thighs | Deep, throbbing, or sharp pain; often described as a dull ache | Variable; can be constant or intermittent |
| Back Pain | Lower back | Aching, dull, or sharp pain, often radiating to the buttocks or thighs | Variable; can be constant or intermittent, often coinciding with pelvic pain |
| Rectal Pain | Rectum | Pressure, aching, or sharp pain in the rectal area | Variable; can be constant or intermittent, often worsening during bowel movements |
| Abdominal Pain | Abdomen | Generalized cramping or aching pain; can be sharp or dull | Variable; can be constant or intermittent, potentially related to location of endometriosis implants |
Menstrual Cycle Disruptions
Understanding your menstrual cycle is crucial for overall well-being. Knowing the typical patterns allows you to recognize deviations that could signal underlying conditions. Paying attention to changes in your cycle, even subtle ones, can be a vital first step in identifying potential issues like endometriosis.
How Menstrual Cycle Changes Indicate Endometriosis
Menstrual cycle irregularities are a common symptom of endometriosis. The condition affects the lining of the uterus, causing endometrial tissue to grow outside of it. This can lead to a variety of changes in the menstrual cycle, including pain, bleeding irregularities, and changes in cycle length. Recognizing these changes is key to early detection and treatment.
Different Ways the Cycle Might Be Affected
Endometriosis can disrupt the normal flow of the menstrual cycle in several ways. Changes in cycle length, from shorter to longer periods, are frequently reported. The intensity and duration of bleeding can also be altered, ranging from excessively heavy bleeding (menorrhagia) to spotting or bleeding between periods. In some cases, periods may be completely absent (amenorrhea).
Impact of Abnormal Bleeding on the Body
Abnormal bleeding can have a significant impact on the body. Heavy bleeding can lead to anemia, characterized by fatigue, weakness, and shortness of breath. Irregular bleeding can cause discomfort and disrupt daily life. Pain associated with heavy bleeding can be severe and may require medical attention.
Figuring out the first signs of endometriosis can be tricky, as symptoms often mimic other conditions. While some experience debilitating pain, others might not notice anything at all. Interestingly, a recent article highlighted how the keto diet is seemingly falling out of favor compared to the DASH diet, keto ranked low dash ranked high on new diet list , but that’s a whole other rabbit hole.
Regardless of dietary trends, persistent pelvic pain, heavy bleeding, and painful periods are potential early indicators, but it’s always best to consult a doctor for proper diagnosis.
Examples of Subtle Cycle Changes
Recognizing subtle changes is vital. A few extra days of bleeding, a slightly shorter or longer cycle than usual, or a change in the consistency of the flow can all be early indicators. These minor shifts, though seemingly insignificant, might signal a larger issue.
Relation Between Cycle Irregularities and Other Symptoms
Endometriosis symptoms often present in conjunction. For example, a change in cycle length might be accompanied by pelvic pain, cramping, or discomfort during intercourse. Paying attention to the totality of symptoms, not just cycle changes, is important for accurate diagnosis.
Comparison of Normal and Abnormal Menstrual Cycles
| Characteristic | Normal Cycle | Abnormal Cycle |
|---|---|---|
| Cycle Length (days) | 21-35 days | Significantly shorter or longer than 21-35 days |
| Bleeding Duration (days) | 3-7 days | Significantly shorter or longer than 3-7 days |
| Bleeding Intensity | Moderate, consistent flow | Extremely heavy (menorrhagia), spotting, or bleeding between periods |
| Pain | Minimal or mild cramping | Significant pelvic pain, cramping, or pain during intercourse |
| Overall Well-being | No significant impact on daily activities | Fatigue, anemia, discomfort, disruption of daily life |
Gastrointestinal Issues
Endometriosis, often characterized by pain, can also manifest in unexpected ways, including through the digestive system. This connection isn’t always immediately apparent, leading to delays in diagnosis and frustration for those experiencing these symptoms. Understanding the potential links between endometriosis and gastrointestinal issues is crucial for navigating these challenges.Gastrointestinal symptoms in endometriosis are often dismissed as typical digestive problems, or attributed to other factors, delaying appropriate medical attention.
However, the underlying inflammation and tissue growth associated with endometriosis can impact the digestive tract, causing a range of discomfort and sometimes mimicking other conditions. Identifying these symptoms as potentially linked to endometriosis is essential for prompt and accurate diagnosis.
Early signs of endometriosis can be tricky to spot, often mimicking other conditions. While some people experience debilitating pain, others might not notice anything at all until later. A crucial aspect of managing potential symptoms, like persistent pelvic pain, is also understanding the importance of a healthy diet, especially as we age. For example, quality of diet for older adults has declined heres how to fix it can have a significant impact on overall health, potentially affecting symptoms like fatigue or cramping.
Ultimately, paying attention to your body and discussing any unusual discomfort with a doctor is key to early diagnosis.
Connection Between Endometriosis and Gastrointestinal Symptoms
Endometriosis can affect various organs within the body, including those of the digestive system. The presence of endometrial tissue outside the uterus can lead to inflammation, scarring, and adhesions within the intestines, stomach, and other digestive structures. These changes can interfere with the normal functioning of the digestive system, causing a range of symptoms.
Common Gastrointestinal Issues
Common gastrointestinal issues associated with endometriosis include abdominal pain, bloating, diarrhea, constipation, nausea, and vomiting. These symptoms can vary in severity and frequency, and they can occur at any point during the menstrual cycle.
Possible Reasons for Gastrointestinal Symptoms
Several factors can contribute to the gastrointestinal symptoms experienced by individuals with endometriosis. The presence of endometrial implants in the digestive tract can cause inflammation, leading to pain and discomfort. Scar tissue formation can obstruct the intestines, further contributing to digestive problems. Hormonal fluctuations associated with endometriosis can also trigger changes in bowel habits.
Link to Other Symptoms
Gastrointestinal symptoms in endometriosis can be linked to other symptoms, such as pelvic pain, heavy bleeding, and fatigue. The interconnectedness of these symptoms highlights the complex nature of endometriosis and the importance of a holistic approach to diagnosis and management.
Potential for Misdiagnosis
Gastrointestinal symptoms associated with endometriosis can easily be mistaken for other conditions, such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), or food sensitivities. The similarity in symptoms can make accurate diagnosis challenging, necessitating a thorough evaluation by a healthcare professional.
Figuring out the first signs of endometriosis can be tricky, as symptoms often mimic other conditions. While exploring various culinary delights, like those found in Franco Noriega’s Peruvian cooking, Franco Noriega Peru cooking offers a fantastic array of flavors, it’s important to remember that persistent pelvic pain, heavy bleeding, or pain during sex could be early indicators.
Ultimately, consulting a doctor is crucial for proper diagnosis and treatment.
Gastrointestinal Symptoms and Potential Connection to Endometriosis
| Symptom | Description | Potential Link to Endo |
|---|---|---|
| Abdominal Pain | Recurring or cyclical pain in the abdomen, often worsening before or during menstruation. | Inflammation and/or adhesions in the digestive tract. |
| Bloating | Feeling of fullness or distension in the abdomen. | Potential interference with bowel motility and fluid retention. |
| Diarrhea | Frequent bowel movements with loose or watery stool. | Inflammation and/or irritation of the digestive tract. |
| Constipation | Difficulty passing stool, often with hard, dry stools. | Inflammation and/or obstruction of the digestive tract. |
| Nausea and Vomiting | Feeling of sickness in the stomach, sometimes leading to vomiting. | Potential irritation of the digestive system or hormonal fluctuations. |
| Pelvic Pain | Pain in the lower pelvis, often worsened during menstruation. | Can be present in both the pelvic and gastrointestinal areas due to endometriosis. |
| Heavy Bleeding | Excessively heavy menstrual bleeding. | Both pelvic and gastrointestinal symptoms are connected to the hormonal changes associated with endometriosis. |
Pelvic Pain and Discomfort: What Are The First Signs Of Endometriosis
Pelvic pain, a common symptom of endometriosis, often presents as a dull ache or sharp cramps, varying in intensity and location. Understanding its specific characteristics and how it differs from other conditions is crucial for accurate diagnosis and effective management. This section will delve into the nuances of pelvic pain associated with endometriosis, providing insights into its manifestations, potential distinctions from other conditions, and influencing factors.Endometriosis-related pelvic pain can manifest in a multitude of ways, ranging from mild discomfort to debilitating agony.
It’s not always consistent and can fluctuate depending on the individual’s hormonal cycle, physical activity, and stress levels. The intensity and location of pain are not always predictable and can vary significantly from person to person.
Characteristics of Endometriosis Pelvic Pain
Endometriosis-related pelvic pain is often described as a deep, cramping pain, sometimes accompanied by pressure or throbbing sensations. The pain may radiate to other areas, including the lower back, abdomen, or thighs. Its intensity can range from mild to severe, with some experiencing debilitating pain that significantly impacts daily life. Pain can be cyclical, worsening during menstruation, or it may be persistent and chronic.
Examples of Pelvic Pain Manifestations
Pelvic pain can manifest in various ways, affecting different parts of the pelvis. It can be felt as a dull ache in the lower abdomen, a sharp stabbing pain, or a throbbing sensation. Some individuals might experience intense cramping, particularly during menstruation. Pain can also radiate to the lower back, buttocks, or even the groin area. In some cases, pain might be localized to one side of the pelvis.
Distinguishing Endometriosis Pelvic Pain from Other Conditions
Differentiating endometriosis pelvic pain from other conditions can be challenging. Other conditions like ovarian cysts, pelvic inflammatory disease (PID), or uterine fibroids can also cause pelvic pain. A thorough medical history, physical examination, and potentially diagnostic imaging (like ultrasound or MRI) are often necessary to accurately determine the underlying cause. The presence of other symptoms, such as irregular periods, painful intercourse, or bowel/bladder issues, can provide clues for diagnosis.
Factors Influencing Pelvic Pain Intensity
Several factors can influence the intensity of pelvic pain associated with endometriosis. These include the severity and location of the endometrial implants, the hormonal fluctuations throughout the menstrual cycle, and the presence of other conditions like adenomyosis. Stress, physical activity, and certain foods can also exacerbate the pain.
Impact of Pelvic Discomfort on Daily Life
Pelvic pain and discomfort from endometriosis can significantly impact daily life. Activities like walking, exercising, or even sitting for extended periods can become challenging. The pain can affect social activities, work productivity, and overall well-being. In severe cases, it can lead to limitations in daily routines and an overall reduced quality of life.
Comparing Pelvic Pain Causes
| Cause | Symptom Description | Location | Intensity |
|---|---|---|---|
| Endometriosis | Deep, cramping, pressure, or throbbing pain, may radiate; cyclical, worsening during menstruation | Lower abdomen, pelvis, lower back, thighs | Mild to severe |
| Ovarian Cysts | Sharp, sudden pain, often localized to one side; may be associated with bloating or nausea | Lower abdomen, pelvis | Mild to moderate, potentially severe |
| Pelvic Inflammatory Disease (PID) | Deep, aching pain; may be accompanied by fever, chills, abnormal vaginal discharge | Lower abdomen, pelvis | Moderate to severe |
| Uterine Fibroids | Aching, cramping pain; may be associated with heavy bleeding | Lower abdomen, pelvis | Mild to moderate |
Physical Examination Findings
Physical examinations play a crucial role in assessing potential endometriosis, but they often reveal subtle signs. A thorough evaluation, including a detailed medical history, is essential for identifying patterns and potential indicators of the condition. It’s important to remember that physical exams alone are rarely definitive for diagnosing endometriosis; they usually serve to support or raise suspicion, which then warrants further investigation.Physical examination findings for endometriosis can be subtle and variable, often mimicking other conditions.
Careful palpation and assessment are necessary to differentiate potential symptoms from other causes. The presence of specific findings, when considered alongside a comprehensive medical history, can help healthcare providers form a more complete picture of the patient’s condition.
Potential Physical Examination Findings
A thorough physical examination can reveal certain findings that might suggest the presence of endometriosis. These findings are often subtle and require careful assessment by a healthcare professional experienced in recognizing these subtle signs. The examination usually involves a careful palpation of the pelvic region, focusing on tenderness, nodules, or masses. A detailed medical history helps in interpreting the findings in the context of the patient’s specific symptoms and cycle patterns.
Specific Physical Exam Maneuvers
Certain physical exam maneuvers can help detect potential signs of endometriosis. These include:
- Pelvic palpation: Careful palpation of the pelvic region, including the uterus, ovaries, and surrounding tissues, can reveal tenderness, nodules, or masses that may be indicative of endometriosis implants. This requires a skilled examiner who can discern subtle differences in tissue consistency and tenderness.
- Rectovaginal examination: This examination, conducted with the patient in a lithotomy position, involves inserting fingers into the rectum and vagina simultaneously. This allows for a deeper assessment of the pelvic organs and tissues. Tenderness, scarring, or adhesions in the rectovaginal septum may be indicative of endometriosis.
- Tenderness: Specific areas of tenderness in the lower abdomen or pelvis can sometimes indicate the presence of endometriosis implants. The location and intensity of tenderness are important factors to consider.
- Adhesions: Significant adhesions between organs in the pelvic cavity can result from endometriosis and may be revealed during examination. This can be indicated by restricted movement or fixation of certain organs.
Limitations of Physical Examinations
Physical examinations have limitations in definitively diagnosing endometriosis. The condition’s location, severity, and extent of involvement can make detection challenging. Endometriosis implants can sometimes be small and deeply embedded, making them difficult to detect during a physical examination. The presence of other conditions can also mimic the symptoms of endometriosis, making accurate differentiation difficult. It’s essential to remember that a negative physical examination does not rule out the possibility of endometriosis.
Importance of a Detailed Medical History
A detailed medical history is crucial for evaluating potential endometriosis. The history should include information about the patient’s menstrual cycle, pain patterns, and any previous surgeries or medical conditions. Understanding the patient’s specific symptoms, such as pain intensity, duration, and location, helps to contextualize any physical examination findings. The history provides crucial information for determining if the patient’s presentation warrants further diagnostic investigations.
Summary Table of Potential Physical Exam Findings, What are the first signs of endometriosis
| Finding | Description | Potential Significance |
|---|---|---|
| Tenderness in the lower abdomen/pelvis | Pain or discomfort upon palpation in specific areas | May indicate the presence of endometriosis implants or lesions |
| Nodules or masses | Palpable lumps or growths in the pelvic region | May suggest the presence of endometriosis implants or adhesions |
| Adhesions | Restricted movement or fixation of pelvic organs | May result from chronic endometriosis inflammation and scarring |
| Fixation of the uterus or ovaries | Inability to move the uterus or ovaries easily during examination | May indicate the presence of adhesions caused by endometriosis |
| Deep dyspareunia | Pain during sexual intercourse | May indicate endometriosis implants in the pelvic region |
| Rectovaginal tenderness | Pain or discomfort upon palpation in the rectovaginal septum | Suggests potential endometriosis implants in the rectovaginal space |
Imaging Techniques and Diagnostic Tools
Pinpointing endometriosis can be a challenge, as its symptoms can mimic other conditions. Accurate diagnosis often relies on a combination of patient history, physical examination, and imaging techniques. These methods play a crucial role in identifying the location, extent, and characteristics of endometrial tissue growth outside the uterus.Precise imaging techniques are essential to visualize and confirm the presence of endometriosis lesions, aiding in the formulation of a comprehensive treatment plan.
This is particularly vital in early detection, as early intervention can potentially improve long-term outcomes.
Common Imaging Techniques
Various imaging techniques contribute to the diagnostic process. These methods provide different levels of detail and have varying degrees of effectiveness in detecting endometriosis. The choice of technique often depends on the specific clinical situation and the suspected location of the lesions.
Ultrasound
Ultrasound, a non-invasive imaging technique, is frequently employed in the initial assessment of suspected endometriosis. Transvaginal ultrasound, in particular, offers a detailed view of the pelvic organs, enabling visualization of endometrial implants in the ovaries, fallopian tubes, and surrounding tissues. This method is particularly useful for detecting ovarian cysts, a common feature associated with endometriosis.
Magnetic Resonance Imaging (MRI)
MRI provides more comprehensive anatomical information compared to ultrasound. Its ability to distinguish between different tissues allows for a more precise evaluation of the extent and location of endometriosis implants. This detailed view is especially valuable in complex cases or when lesions are deep within the pelvis. MRI can also aid in distinguishing endometriosis from other conditions, such as uterine fibroids.
Other Imaging Methods
While ultrasound and MRI are the most commonly used imaging methods for endometriosis, other techniques might be employed depending on the circumstances. For instance, Computed Tomography (CT) scans, though less frequently used, can offer valuable information about the extent of disease if ultrasound or MRI are inconclusive or unavailable. However, CT scans involve exposure to ionizing radiation, making them less suitable for routine use.
Limitations and Benefits of Different Imaging Methods
Each imaging technique possesses its own set of limitations and benefits. Ultrasound, for example, is excellent for superficial lesions but may not be as effective in detecting deep infiltrations. MRI, while providing detailed anatomical information, might not be readily available in all settings. The choice of technique should always be tailored to the specific needs of the patient and the information required to support diagnosis and treatment.
Role of Imaging in Early Detection
Early detection of endometriosis is crucial for timely intervention and potentially reducing the long-term impact of the condition. Imaging plays a critical role in this process by visualizing endometrial implants, which might not be evident through physical examination alone. Early diagnosis allows for prompt initiation of treatment, potentially minimizing the progression of the disease and its associated symptoms.
Comparison of Imaging Techniques
| Technique | Description | Advantages | Disadvantages |
|---|---|---|---|
| Transvaginal Ultrasound | Uses sound waves to create images of the pelvic organs. | Non-invasive, relatively inexpensive, readily available. | Limited ability to visualize deep lesions, may not differentiate between endometriosis and other conditions. |
| MRI | Uses strong magnetic fields and radio waves to produce detailed images of the body. | Excellent soft tissue contrast, allows visualization of deep infiltrations, can differentiate between different tissues. | More expensive, longer examination time, may not be readily available in all settings, can be contraindicated in certain patients (e.g., those with pacemakers). |
| CT Scan | Uses X-rays to create cross-sectional images of the body. | Good for evaluating bone structures and identifying large masses. | Involves exposure to ionizing radiation, less effective for visualizing soft tissues compared to MRI. |
Closure
In summary, recognizing the first signs of endometriosis is a multifaceted process that requires understanding the diverse range of potential symptoms. From pain and menstrual irregularities to gastrointestinal issues and pelvic discomfort, the condition manifests differently in each individual. While these signs can sometimes be subtle and easily overlooked, awareness and a detailed discussion with your healthcare provider are crucial for early diagnosis and effective management.
Remember, this information is not a substitute for professional medical advice. Always consult with a doctor for proper evaluation and treatment.
