
Whats the difference between atopic and contact dermatitis – What’s the difference between atopic and contact dermatitis? This guide delves into the nuances of these skin conditions, exploring their unique characteristics, causes, and treatments.
Dermatitis, broadly speaking, encompasses various skin inflammations. Atopic and contact dermatitis, while both impacting skin health, arise from distinct mechanisms. Understanding these differences is key to effective diagnosis and treatment.
Introduction to Dermatitis
Dermatitis is a general term for skin inflammation, encompassing a wide range of conditions that cause redness, itching, swelling, and sometimes blistering. It’s a common skin problem affecting people of all ages and can significantly impact quality of life. The specific cause and presentation of dermatitis vary greatly, leading to diverse treatment approaches. Understanding the different types of dermatitis is crucial for accurate diagnosis and effective management.Skin inflammation, a key feature of dermatitis, involves the body’s immune system reacting to a stimulus, either internal or external.
This response leads to increased blood flow to the affected area, resulting in redness and warmth. The release of inflammatory mediators causes swelling, itching, and discomfort. In some cases, the skin may become blistered or ooze fluid. Different triggers, such as allergens, irritants, or infections, can initiate this inflammatory cascade, resulting in varying degrees of severity.
The two types of dermatitis we’ll discuss, atopic and contact dermatitis, differ in their underlying causes and clinical presentations.
General Characteristics of Skin Inflammation
Skin inflammation, a crucial aspect of dermatitis, involves a complex interplay of cellular and chemical processes. The inflammatory response is triggered by various stimuli, including allergens, irritants, infections, and even autoimmune reactions. The initial response typically involves the dilation of blood vessels, leading to increased blood flow and redness in the affected area. This increased blood flow brings immune cells to the site of inflammation, further contributing to the inflammatory cascade.
The release of inflammatory mediators, such as histamine and cytokines, leads to swelling, itching, and pain. In more severe cases, blisters or oozing may occur.
Common Causes of Skin Inflammation
Skin inflammation can be triggered by a multitude of factors. These include allergens, such as certain foods, pollen, or chemicals. Irritants, such as harsh soaps, detergents, or solvents, can also cause inflammation. Infections, both bacterial and fungal, can lead to skin irritation and inflammation. Underlying medical conditions, such as eczema or psoriasis, can also contribute to inflammation.
Environmental factors, such as extreme temperatures or prolonged sun exposure, can also trigger inflammation. Genetic predisposition can also play a role in the development of inflammatory skin conditions.
Comparison of Atopic and Contact Dermatitis
Atopic and contact dermatitis, while both forms of skin inflammation, have distinct characteristics. They share some similarities, as Artikeld in the table below:
| Feature | Description |
|---|---|
| Inflammation | Both types involve skin inflammation, characterized by redness, itching, and swelling. |
| Skin Barrier Dysfunction | In both cases, the skin’s protective barrier may be compromised, allowing irritants and allergens to penetrate more easily. |
| Pruritus (Itching) | Itching is a common symptom in both types, often contributing to skin damage due to scratching. |
Atopic Dermatitis
Atopic dermatitis, often called eczema, is a chronic inflammatory skin condition characterized by dry, itchy skin. It’s a significant health concern affecting individuals of all ages, impacting their quality of life due to the discomfort and potential complications. Understanding the underlying mechanisms, predisposing factors, and presentation across different age groups is crucial for effective management and treatment.Atopic dermatitis is a complex disorder resulting from a combination of genetic susceptibility and environmental triggers.
It’s believed to be an immune system dysfunction, where the skin barrier is compromised, allowing allergens and irritants to penetrate more easily and triggering an inflammatory response. This leads to the characteristic symptoms like redness, itching, and skin dryness. Recognizing the specific presentation in different age groups can aid in prompt diagnosis and appropriate intervention.
Underlying Mechanisms
Atopic dermatitis arises from a complex interplay of genetic and environmental factors. The skin barrier dysfunction plays a crucial role. Defects in the skin’s lipid composition and structure allow for increased transepidermal water loss, making the skin dry and vulnerable to irritants. An overactive immune response, particularly involving T-helper cells, contributes to inflammation and the characteristic itch-scratch cycle.
Figuring out the difference between atopic and contact dermatitis can be tricky, but it’s important for proper treatment. While researching the causes of skin irritation, I stumbled across some interesting research about how experiencing hot flashes at a younger age could increase your risk of heart disease, as detailed in this article: younger you get hot flashes higher heart disease risk.
This got me thinking about how seemingly unrelated health issues can be interconnected, and how understanding the underlying mechanisms of skin conditions like atopic and contact dermatitis is crucial for effective management.
Genetic Predisposition
A strong genetic predisposition contributes significantly to the development of atopic dermatitis. Family history of atopic conditions like asthma, hay fever, and eczema increases the risk. Specific genes associated with immune response, skin barrier function, and inflammation are implicated. This genetic component means that individuals with a family history of these conditions are more likely to develop atopic dermatitis themselves.
Environmental Factors
Environmental factors also play a crucial role in triggering and exacerbating atopic dermatitis. Irritants like harsh soaps, detergents, and wool clothing can worsen symptoms. Allergens, such as dust mites, pollen, and pet dander, can also trigger or aggravate the condition. Exposure to certain foods can also be a trigger for some individuals. It is important to note that these environmental factors can interact with the genetic predisposition, making some individuals more susceptible to developing atopic dermatitis.
Presentation Across Age Groups, Whats the difference between atopic and contact dermatitis
The presentation of atopic dermatitis varies significantly across different age groups. Understanding these differences is crucial for proper diagnosis and management.
Typical Presentation of Atopic Dermatitis by Age
| Age Group | Location | Symptoms | Treatment Options |
|---|---|---|---|
| Infants (0-2 years) | Face, scalp, extensor surfaces of extremities | Erythematous, weeping, crusted lesions; often in flexural areas; intense itching | Moisturizers, topical corticosteroids, emollients, avoidance of triggers |
| Children (3-12 years) | Flexural areas (elbows, knees, wrists, ankles); face | Dry, itchy, red, and scaly skin; sometimes with excoriations; lichenification (thickening) may occur | Topical corticosteroids, moisturizers, antihistamines, phototherapy, avoidance of triggers |
| Adolescents and Adults (13+) | Flexural areas (elbows, knees, wrists, ankles); hands, feet, neck, and lower legs; often in the creases | Dry, itchy, and thickened skin; often with lichenification and excoriations; chronic skin folds | Topical corticosteroids, moisturizers, antihistamines, immunosuppressants, phototherapy, avoidance of triggers |
Common Triggers for Atopic Dermatitis
A variety of factors can trigger or worsen atopic dermatitis. Identifying these triggers is essential for managing the condition effectively.
| Trigger | Symptoms | Description | Management |
|---|---|---|---|
| Dry Skin | Dry, itchy, and cracked skin | A common trigger, especially in winter; low humidity can also be a factor. | Frequent moisturizing with emollients, avoiding harsh soaps and detergents. |
| Allergens (Dust mites, pollen, pet dander) | Redness, itching, and inflammation | Exposure to these allergens can trigger a reaction. | Avoiding exposure, using allergen-specific immunotherapy (allergy shots), environmental controls. |
| Irritants (Soaps, detergents, wool) | Redness, itching, and burning | Harsh chemicals can irritate the skin, exacerbating the condition. | Avoiding contact with irritants, using mild cleansers, and choosing appropriate fabrics. |
| Stress | Increased itching and inflammation | Stress can trigger a significant flare-up in some individuals. | Stress management techniques (yoga, meditation, relaxation exercises), seeking support groups. |
Contact Dermatitis
Contact dermatitis is a common skin condition characterized by inflammation and irritation of the skin, often appearing as redness, itching, and sometimes blistering. It’s typically triggered by direct contact with specific substances, either allergens or irritants. Understanding the different types of contact dermatitis is crucial for proper diagnosis and treatment.
Ever wondered about the difference between atopic and contact dermatitis? It’s basically this: atopic is often inherited, while contact is triggered by external factors. This can be similar to how certain environmental factors can worsen asthma, especially during the summer months. For instance, increased pollen counts and humidity can make asthma symptoms flare up. You can find out more about why asthma can be worse during the summer here.
Ultimately, understanding these triggers is key to managing both conditions effectively, and knowing the distinctions between atopic and contact dermatitis is a good starting point.
Types of Contact Dermatitis
Contact dermatitis manifests in two primary forms: allergic and irritant. These distinct types stem from different mechanisms, leading to varying symptoms and treatment approaches. Recognizing the difference is essential for effective management.
Allergic Contact Dermatitis
Allergic contact dermatitis (ACD) occurs when the immune system mistakenly identifies a harmless substance (an allergen) as a threat. The initial exposure to the allergen, often a chemical or plant extract, triggers a sensitization process, which is the development of an immune response. This initial exposure doesn’t typically cause noticeable symptoms. However, subsequent exposures to the same allergen can result in an inflammatory skin reaction.
Sensitization is a crucial step in ACD, where the immune system’s T cells become primed to react to the allergen.
The mechanism involves the following key steps:
- Exposure to allergen: Initial contact with the substance.
- Sensitization: The immune system’s T cells are activated and primed to recognize the allergen.
- Subsequent exposure: Contact with the same allergen triggers a reaction from the sensitized T cells.
- Inflammatory response: The immune system releases chemicals that cause inflammation, leading to skin symptoms.
Irritant Contact Dermatitis
Irritant contact dermatitis (ICD) differs from ACD in its mechanism. Unlike ACD, which involves an immune response, ICD arises from the direct damaging effect of a substance on the skin’s barrier. The irritant itself directly harms the skin, causing inflammation and irritation. The intensity of the reaction is often correlated with the concentration and duration of the irritant’s contact with the skin.
No prior sensitization is required.
A strong acid, for example, will directly damage the skin’s protective layers regardless of prior exposure.
The skin’s reaction is typically immediate and proportional to the irritant’s strength and duration of contact.
Common Allergens and Irritants
Numerous substances can trigger contact dermatitis. Allergens frequently implicated in ACD include nickel (often found in jewelry), fragrances, preservatives, and certain plant resins (like poison ivy). Irritants commonly causing ICD include strong detergents, solvents, acids, alkalis, and certain fabrics.
Comparison of Allergic and Irritant Contact Dermatitis
| Feature | Allergic Contact | Irritant Contact | Key Differences |
|---|---|---|---|
| Mechanism | Immune system response (sensitization) | Direct damage to skin barrier | ACD involves an immune response, while ICD is a direct physical harm. |
| Initial exposure | Often asymptomatic | Immediate and noticeable irritation | ACD may not cause symptoms initially, while ICD shows symptoms immediately. |
| Subsequent exposures | Reaction becomes stronger | Reaction severity depends on irritant strength | ACD shows a more significant reaction upon subsequent exposure, while ICD depends on the irritant. |
| Sensitization | Required | Not required | ACD requires a sensitization phase before a reaction. |
Comparing Atopic and Contact Dermatitis
Atopic dermatitis (AD) and contact dermatitis (CD) are both common inflammatory skin conditions, often causing significant discomfort and impacting quality of life. While both manifest as skin rashes, they differ significantly in their underlying causes, clinical presentation, and management strategies. Understanding these differences is crucial for accurate diagnosis and effective treatment.Differentiating between atopic and contact dermatitis can be challenging, particularly in cases where the clinical features overlap.
Careful consideration of the patient’s history, the distribution and morphology of the lesions, and the potential triggers is essential for appropriate diagnosis and tailored treatment.
Clinical Presentation Comparison
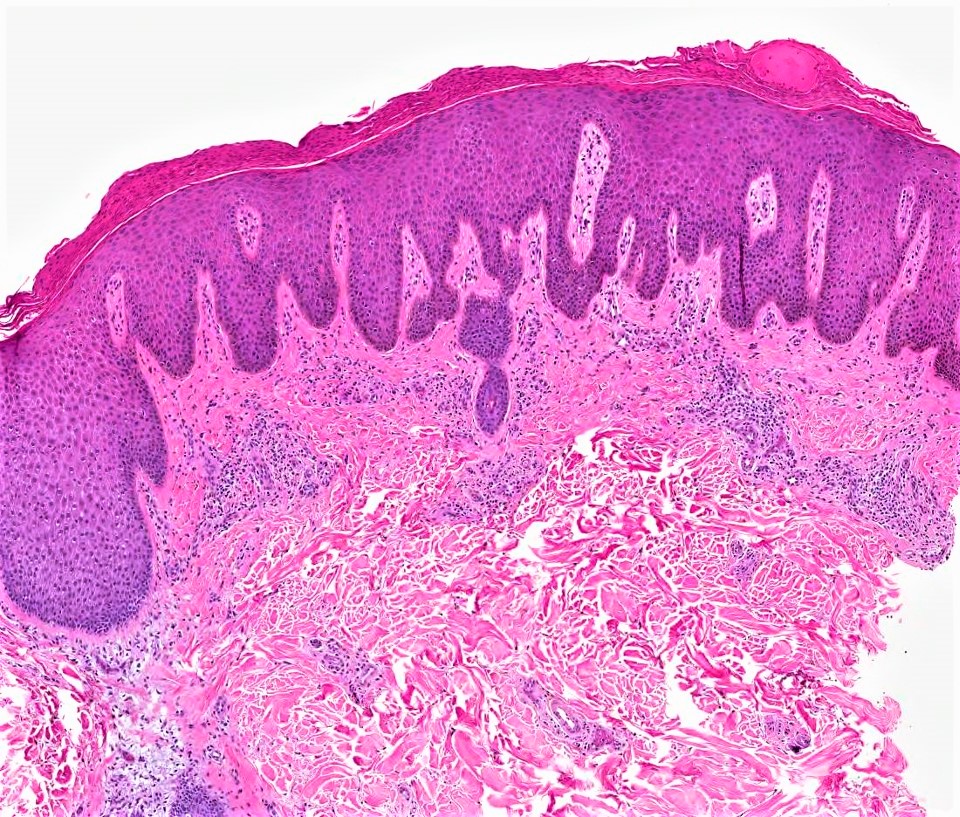
Atopic dermatitis typically presents with chronic, relapsing, and itchy skin inflammation. The characteristic lesions are erythematous, often excoriated, and can be weeping or crusted. They frequently exhibit a characteristic distribution, often involving the flexural areas of the extremities (e.g., antecubital and popliteal fossae) and the face in children. The skin may also appear dry and thickened. In contrast, contact dermatitis is typically an acute or subacute reaction to a specific irritant or allergen.
The lesions are often well-demarcated and confined to the area of contact with the triggering agent. The skin may exhibit redness, swelling, blistering, or oozing, depending on the severity of the reaction.
Diagnostic Approaches
Accurate diagnosis relies on a thorough patient history, physical examination, and potentially, diagnostic testing. The history should focus on potential triggers, the temporal relationship between exposure to a substance and the onset of symptoms, and the pattern of skin involvement. For contact dermatitis, patch testing may be necessary to identify the specific allergen. This involves applying small amounts of suspected allergens to the skin and monitoring for a reaction.
In cases of atopic dermatitis, skin biopsy is rarely required unless there is a suspicion of another underlying condition. However, exclusion of other conditions like psoriasis or fungal infections is important.
Typical Lesions
The lesions in atopic dermatitis often have a characteristic appearance. They are often intensely itchy, erythematous, and may display excoriations due to scratching. The location is typically flexural areas, but can be widespread. Contact dermatitis, conversely, typically presents with lesions that are confined to the area of contact with the offending agent. The lesions can vary from erythema and mild swelling to blistering and oozing, depending on the severity of the reaction and the nature of the irritant.
The morphology may vary from papules and plaques to vesicles and bullae.
History of the Condition
Atopic dermatitis often has a chronic course, with periods of remission and exacerbation. A personal or family history of atopy (e.g., asthma, allergic rhinitis) is frequently observed in patients with atopic dermatitis. In contrast, contact dermatitis typically presents with a clear temporal relationship between exposure to a specific irritant or allergen and the onset of skin symptoms. This relationship is crucial for diagnosis and identification of the causative agent.
Figuring out the difference between atopic and contact dermatitis can be tricky, but it boils down to the cause. Atopic dermatitis often has a genetic component, while contact dermatitis is usually triggered by an external irritant. Interestingly, while we’re on the topic of skin conditions, did you know that there’s a potential link between certain blood cancers like leukemia and stroke?
For a deeper dive into that, check out this article on can leukemia cause a stroke. Regardless, understanding the triggers for different skin conditions, like atopic and contact dermatitis, is key to effective treatment.
Summary Table
| Feature | Atopic Dermatitis | Contact Dermatitis | Key Differences |
|---|---|---|---|
| Clinical Presentation | Chronic, relapsing, itchy inflammation; dry, thickened skin; flexural involvement | Acute or subacute reaction; well-demarcated; confined to contact area; may blister or ooze | Atopic dermatitis is chronic and widespread, while contact dermatitis is typically acute and localized. |
| Triggers | Unknown, but often associated with atopy (asthma, hay fever); environmental factors (stress, allergens) | Specific irritant or allergen; direct contact | Atopic dermatitis triggers are complex and often unknown, while contact dermatitis has a clear trigger. |
| Management | Moisturizing, topical corticosteroids, antihistamines, immunomodulators | Avoidance of trigger; topical corticosteroids; antihistamines | Management strategies reflect the different underlying causes. |
Management and Treatment Strategies
Managing both atopic and contact dermatitis effectively involves a multifaceted approach focusing on symptom relief and preventing future flare-ups. A crucial aspect of this management is understanding the triggers specific to each individual. Early intervention and consistent adherence to treatment plans are vital for achieving optimal outcomes and minimizing long-term complications.
General Principles of Management
Effective management of both atopic and contact dermatitis necessitates a patient-centered approach. This entails close collaboration between the patient, healthcare provider, and potentially a dermatologist. Individualized strategies are paramount, as the severity and triggers of these conditions vary significantly. This involves regular monitoring of symptoms, identifying and avoiding triggers, and consistent application of prescribed treatments.
Importance of Avoiding Triggers
Identifying and meticulously avoiding triggers is fundamental to managing both atopic and contact dermatitis. For atopic dermatitis, common triggers include stress, certain foods, and environmental factors such as dry air and wool clothing. For contact dermatitis, triggers are specific allergens, like nickel, fragrances, or certain chemicals. Keeping a detailed log of potential triggers and reactions can be invaluable in pinpointing and subsequently avoiding these irritants.
Role of Topical Corticosteroids and Other Treatments
Topical corticosteroids are frequently used in managing both atopic and contact dermatitis, particularly for inflammation reduction. However, their use should be carefully considered, and the lowest effective dose should be applied for the shortest duration possible. Other topical treatments like moisturizers, calcineurin inhibitors, and antihistamines may also be employed depending on the severity and type of dermatitis.
Table of Topical and Systemic Treatments
| Treatment Type | Mechanism | Effectiveness | Potential Side Effects |
|---|---|---|---|
| Topical Corticosteroids | Reduce inflammation by suppressing the immune response | Generally effective for short-term relief of inflammation and itching | Skin thinning, striae (stretch marks), atrophy, skin infections, and, with prolonged use, adrenal suppression |
| Topical Calcineurin Inhibitors | Inhibit the activation of immune cells | Effective for managing both atopic and contact dermatitis, often as an alternative to corticosteroids | Skin irritation, burning sensation, and rarely, skin infections |
| Moisturizers | Maintain skin hydration and barrier function | Crucial in managing both atopic and contact dermatitis, particularly in preventing dryness and irritation | Minimal, if any, side effects. Potential for skin reactions in some individuals |
| Antihistamines | Block the action of histamine, a chemical released during inflammation | Can be helpful in managing itching associated with both conditions | Drowsiness, dry mouth, and dizziness (particularly with older antihistamines) |
| Systemic Medications (e.g., oral corticosteroids) | Reduce inflammation throughout the body | Reserved for severe cases that don’t respond to topical treatments | Significant potential for side effects, including adrenal suppression, osteoporosis, and increased risk of infections. Should be used only under strict medical supervision |
Lifestyle Modifications
Implementing lifestyle modifications can significantly aid in managing both atopic and contact dermatitis. Maintaining a regular sleep schedule, practicing stress-reducing techniques, and wearing appropriate clothing can help. For example, individuals with atopic dermatitis might find that avoiding harsh soaps and using hypoallergenic detergents reduces skin irritation. Similarly, individuals with contact dermatitis should carefully examine their environment for potential irritants.
These strategies, along with consistent treatment, can help manage flare-ups and improve overall well-being.
Prevention and Prognosis: Whats The Difference Between Atopic And Contact Dermatitis

Understanding the long-term outlook and preventative measures for both atopic and contact dermatitis is crucial for effective management. These skin conditions, while often treatable, can significantly impact quality of life if not properly addressed. This section delves into strategies for preventing flare-ups and explores the potential long-term implications of each type of dermatitis.Effective prevention and a favorable prognosis depend heavily on lifestyle choices and environmental factors.
Understanding these influences is key to developing personalized management plans and achieving better long-term outcomes.
Strategies for Preventing Atopic Dermatitis
Maintaining a consistent skin care routine is vital for preventing flare-ups. This includes using fragrance-free, hypoallergenic cleansers and moisturizers, and avoiding harsh soaps. Regular, gentle moisturizing, particularly after bathing, helps maintain skin hydration and protects against dryness. Identifying and avoiding triggers, such as specific foods, allergens, or environmental factors, is also essential. Strict avoidance of known allergens and irritants is critical in preventing atopic dermatitis flare-ups.
Strategies for Preventing Contact Dermatitis
Preventing contact dermatitis revolves around identifying and avoiding the specific triggers that cause the allergic or irritant reaction. This often involves meticulous attention to personal care products, household items, and occupational exposures. If a specific irritant or allergen is identified, minimizing or eliminating contact with it is crucial. Using protective gloves when handling potential irritants, like cleaning products, is a key preventative measure.
Proper hand hygiene and the use of protective clothing can prevent occupational contact dermatitis in individuals exposed to certain chemicals or substances.
Prognosis of Atopic Dermatitis
Atopic dermatitis often persists throughout childhood and adolescence, but the severity and frequency of flare-ups can vary significantly. Many individuals experience periods of remission, where symptoms are significantly reduced or absent. However, atopic dermatitis can persist into adulthood, although symptoms may lessen in severity. For example, some individuals experience milder, less frequent flares as they get older.
Prognosis of Contact Dermatitis
The prognosis for contact dermatitis is generally favorable, as it’s often a reaction to a specific trigger. Once the trigger is identified and avoided, the condition typically resolves completely. However, persistent or repeated exposure to the irritant can lead to chronic or recurring issues. For example, chronic hand dermatitis can develop in individuals who repeatedly expose their hands to harsh chemicals or detergents.
Factors Influencing Prognosis
Understanding the factors that influence the prognosis of atopic and contact dermatitis is vital for developing personalized management strategies.
| Factor | Atopic Dermatitis | Contact Dermatitis | Comparison |
|---|---|---|---|
| Age of Onset | Typically begins in infancy or early childhood. | Can occur at any age, but may be more prevalent in specific occupations. | Early onset often leads to longer duration and potentially more severe chronic symptoms in atopic dermatitis. |
| Trigger Identification and Avoidance | Identifying triggers can be challenging and may involve extensive testing. | Identifying triggers is often straightforward once a pattern is established. | Early and accurate trigger identification is crucial for both types to prevent future flare-ups. |
| Severity of Initial Flare-ups | Initial severity can vary significantly. | Severity depends on the concentration and duration of exposure to the trigger. | Severity and frequency of initial flare-ups can influence long-term prognosis and potential for chronic symptoms. |
| Compliance with Treatment Plan | Requires ongoing monitoring and adherence to treatment recommendations. | Compliance focuses on avoiding the specific trigger. | Both conditions necessitate consistent effort to manage and prevent future flare-ups. |
Concluding Remarks
In conclusion, while both atopic and contact dermatitis affect the skin, they differ significantly in their underlying causes, symptoms, and management strategies. Recognizing these key distinctions is essential for appropriate medical care. Consulting a dermatologist is crucial for accurate diagnosis and personalized treatment plans.
