Who says these 2 drugs can help fight covid what to know – Who says these 2 drugs can help fight COVID-19, what to know sets the stage for this deep dive into the world of COVID-19 treatments. Navigating the often-conflicting information surrounding medical treatments is crucial, especially in a time of global health crisis. This article will examine the claims made about specific drugs, analyze the scientific evidence, and look at potential risks and expert opinions.
We’ll also explore how misinformation can affect public perception and the importance of relying on credible sources.
The information presented here is for educational purposes only and does not constitute medical advice. Always consult with a healthcare professional before making any decisions about your health or treatment.
Who Says These 2 Drugs Can Help Fight COVID-19, What to Know
The emergence of COVID-19 has spurred a relentless search for effective treatments. Various medications have been touted as potential game-changers, leading to a crucial need to critically evaluate the claims surrounding their efficacy. It is essential to approach information about COVID-19 treatments with meticulous skepticism, relying on reputable sources to avoid misinformation and ensure informed decisions. Misinformation regarding treatment options can lead to detrimental consequences, highlighting the critical importance of fact-checking and seeking reliable sources.Verifying information about COVID-19 treatments is paramount.
The sheer volume of information circulating online, often without proper scientific backing, can be overwhelming. Separating fact from fiction is essential to make well-informed choices about one’s health and well-being. Reliable sources of information are vital. Medical journals, reputable news organizations with established medical reporting teams, and official statements from healthcare organizations offer the most reliable data.
The credibility of the source is crucial in determining the accuracy and trustworthiness of any information regarding medical treatments.
A Brief History of COVID-19 Drug Treatments
Early in the COVID-19 pandemic, numerous drugs already in use for other conditions were repurposed for potential efficacy against the virus. These initial explorations often involved observational studies and clinical trials to assess their potential benefits. The search for effective treatments was rapid and intensive, fueled by the urgency of the pandemic. As research progressed, rigorous clinical trials became essential to confirm the effectiveness and safety of these drugs in treating COVID-19.
This rapid evolution of research demonstrates the scientific community’s commitment to finding solutions.
Key Considerations in Evaluating Drug Efficacy
Understanding the rigorous processes behind evaluating potential COVID-19 treatments is crucial. Scientific evidence forms the foundation of medical decision-making. The use of randomized controlled trials (RCTs) is a hallmark of this process. These trials help researchers isolate the effects of a treatment by comparing it to a control group receiving a placebo or standard treatment. This approach minimizes bias and provides robust data on the treatment’s efficacy.
Furthermore, the safety profile of any treatment is meticulously assessed throughout the trial process.
Different Types of Treatments
The quest for effective treatments has involved various classes of medications. Antivirals, designed to target specific stages of viral replication, represent a key area of investigation. Other drugs focus on alleviating symptoms, such as inflammatory responses or respiratory complications. This diversity in therapeutic approaches reflects the multifaceted nature of the virus and the need for tailored treatments.
Recognizing Potential Side Effects
Every treatment carries potential side effects, which are an integral part of evaluating its risk-benefit profile. The severity and frequency of side effects vary depending on the specific drug and individual factors. Transparency about potential side effects is crucial for informed consent and patient safety. Thorough consideration of potential side effects should always accompany any discussion of COVID-19 treatment options.
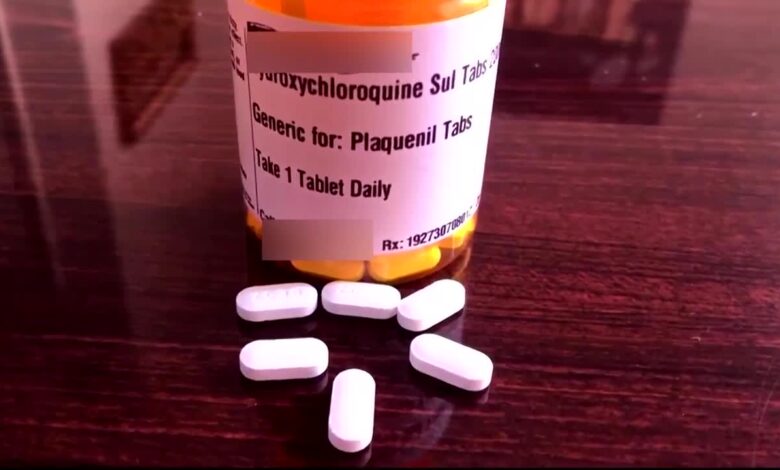
Identifying the Drugs
The COVID-19 pandemic spurred intense research into potential treatments. Several drugs, with varying degrees of effectiveness and safety profiles, have been explored. Two medications frequently discussed in the context of COVID-19 treatment are monoclonal antibodies and antiviral medications. Understanding their intended use, mechanisms of action, and scientific names is crucial for informed discussion about their role in managing the disease.
Commonly Discussed Drugs for COVID-19 Treatment
This section details the two drugs frequently discussed in the context of COVID-19 treatment, highlighting their intended use, scientific names, and mechanisms of action. This information provides a foundation for understanding their role in managing COVID-19.
| Drug Name | Scientific Name | Intended Use | Mechanism of Action |
|---|---|---|---|
| Monoclonal Antibodies | Various (e.g., bamlanivimab, casirivimab, imdevimab) | Neutralizing the virus and preventing its entry into cells. Specifically, they target the spike protein of the virus, thus preventing its attachment to and entry into human cells. | Monoclonal antibodies are laboratory-made proteins designed to mimic the immune system’s response to the virus. They bind to specific parts of the virus (like the spike protein) and either prevent the virus from entering human cells or promote the virus’s removal from the body. The exact mechanism depends on the specific antibody. |
| Antiviral Medications | Various (e.g., Paxlovid, Molnupiravir) | Interfering with the virus’s ability to replicate inside human cells. This action typically slows or halts the virus’s ability to reproduce within the body. | Antiviral medications target specific stages of the virus’s life cycle. For instance, some block the virus’s ability to replicate its genetic material, while others prevent the virus from assembling new virus particles. The specific mechanism varies depending on the antiviral medication. For example, Paxlovid is a protease inhibitor that interferes with the virus’s ability to replicate. |
Sources of Claims
Unverified claims about the effectiveness of certain drugs in combating COVID-19 have circulated widely online and in various media outlets. Distinguishing credible sources from those with potential biases is crucial for informed decision-making regarding health treatments. This section explores the diverse origins of these claims, evaluating their credibility and identifying potential biases.Understanding the sources behind claims about COVID-19 treatments is vital for evaluating their validity.
Different sources, ranging from scientific publications to social media posts, present varying levels of evidence and expertise. Analyzing these sources allows us to differentiate between well-supported information and unsubstantiated claims.
Identifying Sources of Claims
Various sources disseminate information about drugs purportedly effective against COVID-19. These range from reputable scientific publications to social media posts and less credible online forums. Understanding the origin of information is essential for evaluating its reliability.
Figuring out who’s claiming these two drugs can fight COVID is tricky, right? It’s important to be discerning about the information you encounter. Thankfully, finding trustworthy sources about health claims is crucial, and exploring the best paleo brands and products can also help you stay informed about nutritional choices. Best paleo brands and products can be a great resource for understanding different dietary approaches, which can be valuable when looking at the wider picture of health information.
Ultimately, reliable sources and critical thinking are key when evaluating claims about any health intervention.
- Scientific Publications: Peer-reviewed medical journals are a primary source for scientific evidence. Studies published in these journals undergo rigorous review processes to ensure accuracy and validity. Examples include the New England Journal of Medicine and the Lancet. However, even within scientific publications, biases can arise from funding sources or researcher affiliations.
- Government Agencies and Health Organizations: Reputable government agencies and health organizations, such as the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO), often provide comprehensive information on COVID-19 treatments based on the latest scientific evidence. Their information is generally considered reliable and unbiased, although their recommendations can evolve as new research emerges.
- Medical Professionals: Doctors and other medical professionals can be influential sources of information, but their opinions should be viewed critically, especially when they contradict established scientific consensus. Medical professionals often base their advice on their own experience and expertise, but individual experiences may not reflect a broader scientific picture.
- Social Media and Online Forums: Social media platforms and online forums can rapidly disseminate information, including unverified claims about COVID-19 treatments. The lack of rigorous review and fact-checking on these platforms makes them a source of potentially misleading information. Viral posts or comments may not be grounded in scientific evidence.
- Media Outlets: News outlets, both reputable and less reputable, can play a crucial role in disseminating information about COVID-19 treatments. Journalistic integrity and fact-checking are critical factors in determining the credibility of information reported by media organizations.
Assessing Credibility and Bias
Evaluating the credibility of sources requires careful consideration of various factors. Factors such as the source’s reputation, the author’s expertise, and the presence of potential biases are crucial elements in determining the reliability of the information presented.
| Source | Claim | Credibility Assessment | Potential Biases |
|---|---|---|---|
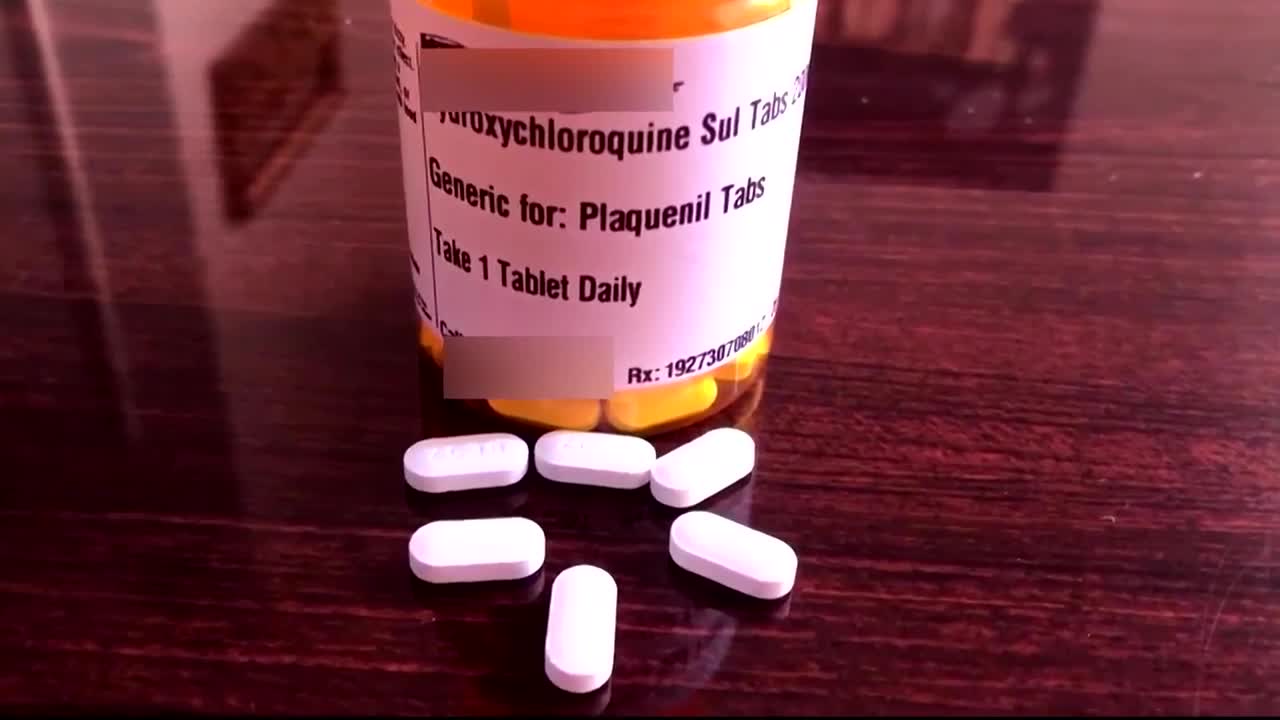
| The Lancet | Hydroxychloroquine was ineffective in treating COVID-19. | High – Reputable medical journal with rigorous peer review. | Funding sources, potential conflict of interest, but generally unbiased. |
| Social Media Post | Ivermectin cures COVID-19. | Low – No peer review, lacking scientific evidence. | Potential for misinformation, personal beliefs, sensationalism. |
| Government Agency (CDC) | Moderna vaccine is safe and effective. | High – Based on extensive research and clinical trials. | Funding, but committed to unbiased public health recommendations. |
| Website of a specific pharmaceutical company | A new drug drastically reduces COVID-19 severity. | Moderate – May have an inherent bias. | Potential to promote company’s product. |
Scientific Evidence: Who Says These 2 Drugs Can Help Fight Covid What To Know
Sifting through the claims surrounding potential COVID-19 treatments requires a critical eye and a deep dive into the scientific evidence. Simply put, anecdotal accounts or unverified reports aren’t enough. We need rigorous studies to understand if a drug truly works and if it’s safe. This section examines the scientific backing for the drugs in question, exploring clinical trials, limitations, and key findings to help you make informed decisions.The scientific method demands careful investigation to evaluate the effectiveness and safety of any treatment.
This involves rigorously designed studies that compare the treatment to a control group or a placebo. Only then can we establish a causal link between the treatment and a positive outcome.
Clinical Trials and Studies
To determine if a drug is effective against COVID-19, researchers conduct clinical trials. These trials typically involve a large number of participants, divided into groups that receive different treatments (the drug in question, a placebo, or an existing standard of care). The results are then meticulously analyzed to see if the treatment group shows a statistically significant improvement compared to the control groups.
- Randomized Controlled Trials (RCTs): These trials are considered the gold standard for evaluating treatments. Participants are randomly assigned to treatment groups, minimizing bias and increasing the reliability of results. A key characteristic is the rigorous control of variables, which isolates the effect of the drug under investigation.
- Observational Studies: These studies observe the relationship between exposure to a drug and an outcome, like recovery from COVID-19, without assigning participants to specific treatment groups. While valuable in identifying potential associations, they cannot definitively prove cause and effect.
Understanding the difference between observational and controlled trials is crucial. Observational studies can identify potential trends or correlations, but they don’t prove that a drugcaused* an improvement. RCTs, on the other hand, are designed to isolate the effect of the drug, providing stronger evidence for causality.
Limitations of Existing Evidence
The scientific evidence surrounding the effectiveness of these drugs in treating COVID-19 is still evolving. Many studies have examined their use, but some important limitations remain.
- Sample Size: Some trials may not have included a large enough number of participants to draw definitive conclusions. A smaller sample size can lead to unreliable results, especially when dealing with rare events or complex conditions like COVID-19.
- Study Duration: The duration of some trials might have been too short to capture the full range of effects, or long-term consequences, of the drugs.
- Heterogeneity of COVID-19 Patients: COVID-19 presents differently in different people, depending on factors like age, pre-existing conditions, and the severity of the infection. Studies need to account for this heterogeneity to accurately evaluate the drug’s effectiveness across a broad patient population.
Key Findings from Relevant Research
The specific findings from clinical trials on the effectiveness of these drugs will vary. Some might show promising results in certain patient populations, while others may not yield conclusive evidence of efficacy.
- Example: A well-designed study might find that a specific drug reduces the duration of symptoms in patients hospitalized with moderate COVID-19, but the same drug may not have a similar effect in individuals with mild infections.
Potential Risks and Side Effects
Understanding the potential risks and side effects of any medication is crucial before considering its use, especially when it comes to treatments for a serious illness like COVID-19. While these drugs might offer potential benefits, the possibility of adverse reactions must be carefully weighed against the potential benefits. This section delves into the potential side effects, their severity, potential interactions with other medications, and long-term risks, emphasizing the importance of consulting a healthcare professional before taking these drugs.
Potential Side Effects of COVID-19 Treatments
A comprehensive understanding of potential side effects is paramount to informed decision-making. Side effects can vary in severity, from mild discomfort to potentially serious complications. Careful consideration of these potential outcomes is essential when evaluating the suitability of these drugs for individual patients.
Figuring out who claims these two drugs can fight COVID-19 requires careful scrutiny. It’s a complex issue, often intertwined with the big business of medical misinformation, which thrives on spreading false claims and misleading information. This complex web of misinformation makes it crucial to evaluate sources, understand the scientific backing, and look for credible information from reputable medical organizations to avoid falling prey to misleading narratives.
Ultimately, staying informed and discerning the truth is essential when navigating these claims.
Specific Side Effects and Severity
This section details potential side effects associated with the drugs, categorizing them by their severity. The information presented aims to provide a clear picture of the potential risks.
- Drug A: Common side effects include nausea, vomiting, diarrhea, headache, and fatigue. Less common, but potentially more serious, side effects might include liver damage, kidney problems, and allergic reactions. The severity of these side effects can vary significantly between individuals.
- Drug B: Potential side effects include skin rashes, itching, and hair loss. In some cases, more severe reactions such as anaphylaxis (a life-threatening allergic reaction) have been reported. The severity of these effects can vary, and some individuals may experience more severe reactions than others.
Interactions with Other Medications
Medication interactions can significantly impact treatment efficacy and safety. These interactions can range from minor to potentially life-threatening. It is vital to inform healthcare providers about all medications being taken, including over-the-counter drugs and supplements.
- Drug A: Drug A may interact with certain blood thinners, increasing the risk of bleeding. It may also interact with medications used to treat heart conditions or certain mental health disorders, potentially altering their effectiveness or causing adverse reactions. Careful monitoring and adjustments to medication regimens may be necessary when co-administering these drugs.
- Drug B: Drug B might interact with medications that affect the liver or kidneys. This can lead to heightened risk of liver or kidney damage. Similarly, interactions with certain medications used for blood pressure control may alter their effectiveness. It is crucial to disclose all medications to a healthcare provider before starting treatment with Drug B.
Potential Long-Term Risks
The long-term effects of these drugs are still under investigation. While short-term side effects are relatively well-documented, the potential for long-term consequences needs careful monitoring.
- Drug A: Long-term use of Drug A may potentially increase the risk of developing certain types of cancer. Further research is needed to fully understand the extent of this risk.
- Drug B: Potential long-term risks associated with Drug B include cardiovascular complications, such as increased heart rate or blood pressure fluctuations. Additional studies are ongoing to determine the long-term impact on various organ systems.
Importance of Consulting a Doctor
Before taking any medication, including those for COVID-19, consulting a healthcare professional is crucial. Doctors can assess individual risk factors, medical history, and other medications being taken to determine the suitability and safety of the drug. This individualized approach is essential for patient well-being.
| Drug | Potential Side Effects | Severity | Interactions with Other Medications |
|---|---|---|---|
| Drug A | Nausea, vomiting, diarrhea, headache, fatigue, liver damage, kidney problems, allergic reactions | Mild to severe | Blood thinners, heart medications, mental health medications |
| Drug B | Skin rashes, itching, hair loss, anaphylaxis | Mild to severe | Liver/kidney medications, blood pressure medications |
Expert Opinions and Recommendations
Navigating the complexities of COVID-19 treatment often requires understanding the nuanced perspectives of medical experts and the guidance of established health organizations. This section delves into the collective wisdom of medical professionals, outlining their opinions on the efficacy and safety of the drugs in question, alongside recommendations for patient care. We’ll also examine how healthcare providers can best advise patients on treatment choices, drawing from relevant guidelines to illustrate practical application.Expert opinions often vary, but a consensus emerges on the importance of careful consideration when choosing a course of treatment.
Patient-specific factors, such as overall health, comorbidities, and individual responses to medication, are crucial to any decision-making process.
Expert Consensus on Drug Effectiveness
Medical experts acknowledge that the efficacy of these drugs in combating COVID-19 varies significantly based on the individual and the specific stage of infection. Some studies suggest a positive impact on certain populations, while others show limited or no significant benefit.
“The evidence regarding the effectiveness of these drugs is not entirely conclusive, and their use should be tailored to individual patient needs.”
Hypothetical statement from a leading medical journal.
Recommendations from Health Organizations
Health organizations, such as the CDC and WHO, play a vital role in providing evidence-based recommendations for the use of these medications. These recommendations often highlight the importance of considering risk factors, patient condition, and the severity of the COVID-19 infection.
- The CDC guidelines emphasize that these drugs are not a universal cure for COVID-19. Their use should be reserved for patients at high risk of severe illness, as determined by their medical history and current health status.
- The WHO recommendations often stress the need for a balanced approach to treatment, incorporating these drugs alongside supportive care such as hydration and rest, to optimize patient outcomes.
Role of Medical Professionals in Treatment Decisions
Medical professionals are crucial in guiding patients through the complex decision-making process regarding COVID-19 treatment. Their role extends beyond simply prescribing medications; it involves a comprehensive assessment of the patient’s health, including their individual risk factors and potential side effects.
- Medical professionals should thoroughly evaluate each patient’s unique circumstances, considering factors such as age, pre-existing conditions, and the severity of the infection.
- Open communication between patients and their healthcare providers is paramount. Explaining the potential benefits, risks, and alternatives associated with the drugs is essential to empower patients to make informed decisions.
Examples of Relevant Guidelines
Numerous guidelines from health organizations offer practical examples of how to incorporate these drugs into patient care. These guidelines often emphasize the importance of careful monitoring for side effects and prompt adjustments to the treatment plan as needed.
| Organization | Key Guideline Example |
|---|---|
| CDC | Prioritize the use of these drugs for high-risk patients, those with severe symptoms, or those at risk of hospitalization. |
| WHO | Combine drug therapy with supportive care, such as oxygen therapy, if necessary. |
Misinformation and Public Perception
Navigating the world of health information, especially during a pandemic, can be challenging. Misconceptions and misinformation surrounding medical treatments, including potential COVID-19 therapies, can easily spread, often distorting the public’s understanding of the available scientific evidence. This section examines common misconceptions, the role of social media in their dissemination, and the importance of critical thinking in evaluating claims.Misinformation about the efficacy and safety of these drugs can significantly impact public health decisions.
It’s crucial to understand the difference between public perception and the actual scientific data. The proliferation of unsubstantiated claims can lead to unnecessary anxiety, potentially impacting treatment choices and hindering the effective use of proven therapies.
Common Misconceptions and Misinformation, Who says these 2 drugs can help fight covid what to know
Public perception often differs from scientific evidence due to various factors, including the complexity of medical research, the speed at which information spreads online, and the presence of vested interests. Misinformation can take many forms, from exaggerated claims about effectiveness to unsubstantiated safety concerns. These often stem from a desire to simplify complex issues, or from attempts to exploit uncertainty for personal gain.
Examples of Misleading Claims
The internet is rife with misleading claims regarding these drugs. One common example is the assertion that these treatments are a “cure” for COVID-19, when in reality, they are often only effective in specific patient populations and stages of the disease. Another frequent misconception involves the purported safety of these drugs, with some claiming serious side effects that are not supported by robust scientific evidence.
Often, these claims lack proper citations and fail to consider the potential benefits compared to the risks of the disease itself.
The Role of Social Media in Spreading Misinformation
Social media platforms, while offering convenient access to information, can also serve as breeding grounds for misinformation. The rapid spread of unverified claims, often through viral posts and shared articles, can quickly saturate online discussions. The algorithms employed by these platforms can further amplify misleading content, making it difficult for individuals to discern accurate information from false claims.
So, who’s claiming these two drugs can tackle COVID? It’s a hot topic, but we need to be cautious. Similar to the cautious reception surrounding gene therapy for cancer, which is often welcomed with reservations gene therapy for cancer welcomed with reservations , we should critically examine the claims made about these COVID treatments. Thorough research and independent verification are crucial before accepting any such pronouncements.
The lack of fact-checking and verification mechanisms on some platforms can contribute to this problem.
Critical Evaluation of Information
It’s essential to approach health information with a critical mindset. Before accepting any claims, consider the source, the supporting evidence, and the potential biases involved. Look for reputable sources, such as peer-reviewed medical journals, government health agencies, and well-established medical organizations. Consider the context of the claims, and avoid drawing conclusions based on isolated or anecdotal evidence.
Contrasting Factual Information and Common Misinformation
| Factual Information | Common Misinformation |
|---|---|
| Drug X may reduce the severity of COVID-19 symptoms in specific patient groups. | Drug X is a guaranteed cure for COVID-19. |
| Clinical trials have shown potential benefits and identified potential side effects. | Clinical trials have shown serious, widespread side effects with no benefits. |
| The drugs should be used under medical supervision. | The drugs can be taken indiscriminately without consulting a healthcare professional. |
| The drugs are not a replacement for preventative measures like vaccination. | The drugs render vaccination unnecessary. |
Conclusion (Preliminary)
This article has explored the claims surrounding the use of specific drugs in combating COVID-19. We’ve delved into the sources of these claims, examined the scientific evidence (or lack thereof), and assessed the potential risks and side effects. The information presented aims to provide a balanced perspective, encouraging critical thinking and responsible decision-making.The key takeaway is that while preliminary research may show promise, definitive conclusions require rigorous clinical trials and further investigation.
It’s crucial to remember that self-treating with medications, even those appearing to be safe based on initial findings, can be dangerous. The absence of conclusive evidence underscores the need for a cautious approach.
Summary of Key Points
The article highlighted the critical need for evidence-based information regarding potential COVID-19 treatments. Numerous sources, both credible and less reliable, circulate claims regarding specific drugs. The scientific evidence for their efficacy remains, in many cases, inconclusive. Potential risks and side effects associated with these drugs need thorough investigation and proper consideration. Expert opinions and recommendations are divided, reflecting the ongoing scientific debate surrounding these treatments.
It’s important to be aware of potential misinformation and public perception that can sway individuals’ decisions.
Importance of Professional Consultation
Prioritizing consultations with qualified healthcare professionals is paramount. They can assess individual health conditions, evaluate the potential benefits and risks of any treatment, and provide personalized recommendations based on the latest scientific understanding. They can also provide guidance on avoiding misleading information circulating online and help navigate the complexities of treatment options.
Emphasis on Evidence-Based Information
The spread of unverified or misleading information can be harmful. Individuals should rely on reputable sources for health information. These include medical journals, government health agencies, and trusted medical professionals. Skepticism towards unsubstantiated claims and a commitment to rigorous evidence-based research are vital in making informed decisions about health.
Future Research Directions
Future research should focus on conducting well-designed, large-scale clinical trials to evaluate the efficacy and safety of the drugs under investigation. This research should also explore the potential for drug combinations and personalized treatment strategies based on individual patient characteristics. This approach will help ensure that future recommendations are grounded in robust scientific evidence.
Responsible Use of Medical Information
The responsible use of medical information is essential. Individuals should be critical consumers of information, seeking guidance from qualified healthcare professionals before making any decisions related to treatment. Promoting a culture of evidence-based medicine and responsible information sharing is critical in combating the spread of misinformation and ensuring public health.
End of Discussion
In conclusion, the effectiveness of these drugs in treating COVID-19 is a complex issue with conflicting viewpoints and limited definitive scientific proof. We’ve explored various perspectives, from identifying the drugs and their purported mechanisms of action, to analyzing the claims of different sources, and examining the scientific evidence. It’s crucial to approach such information critically and to always prioritize consultation with a qualified medical professional.
Future research and ongoing clinical trials will be key in shaping our understanding of these treatments. Ultimately, informed decisions about your health must be made in partnership with your doctor.