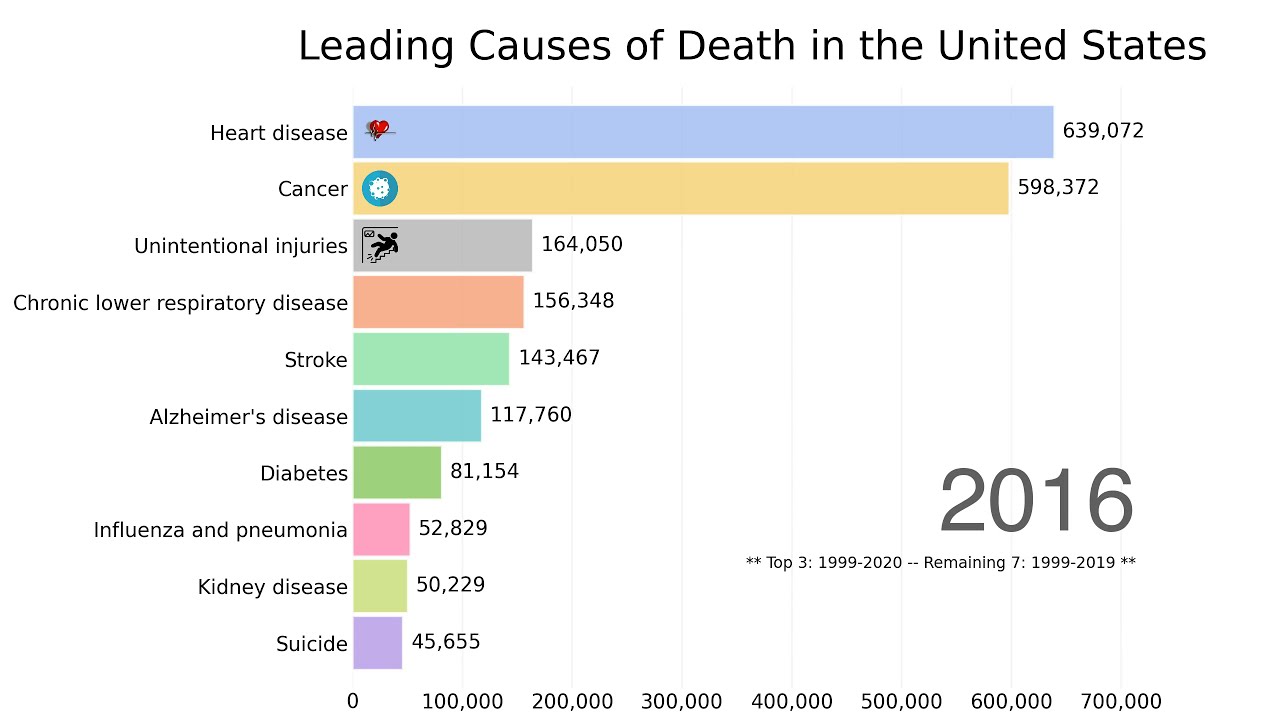
Why despair deaths continue to rise in the US is a complex issue demanding urgent attention. This multifaceted problem touches upon historical trends, socioeconomic factors, access to mental healthcare, cultural influences, and the impact of trauma. Understanding these interconnected elements is crucial to developing effective prevention strategies and supporting those struggling with despair.
Examining historical data reveals a concerning upward trend in despair-related deaths, often correlating with economic downturns and societal shifts. Socioeconomic factors, like poverty and inequality, play a significant role, highlighting the disparities in access to resources and support. Mental health services, often inaccessible or unaffordable, compound the problem, and cultural stigmas surrounding mental illness can hinder help-seeking behavior.
Trauma, both historical and contemporary, also significantly contributes to the rise in despair, impacting individuals and communities in profound ways. Finally, the role of healthcare systems in identifying and supporting those at risk is a critical factor in mitigating the crisis.
Historical Context of Despair Deaths
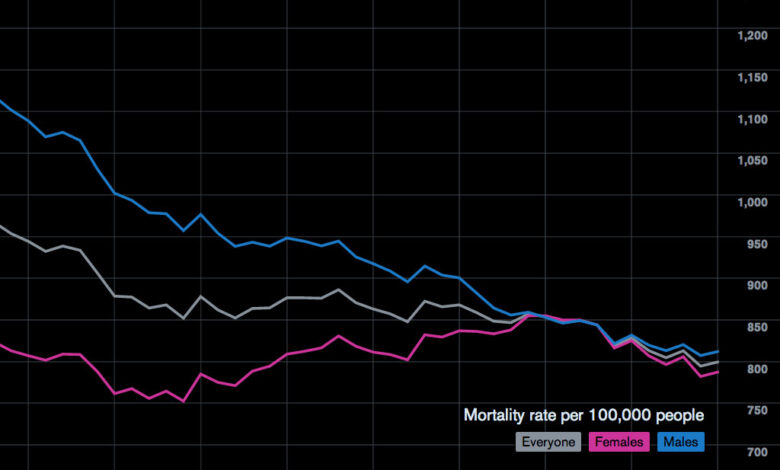
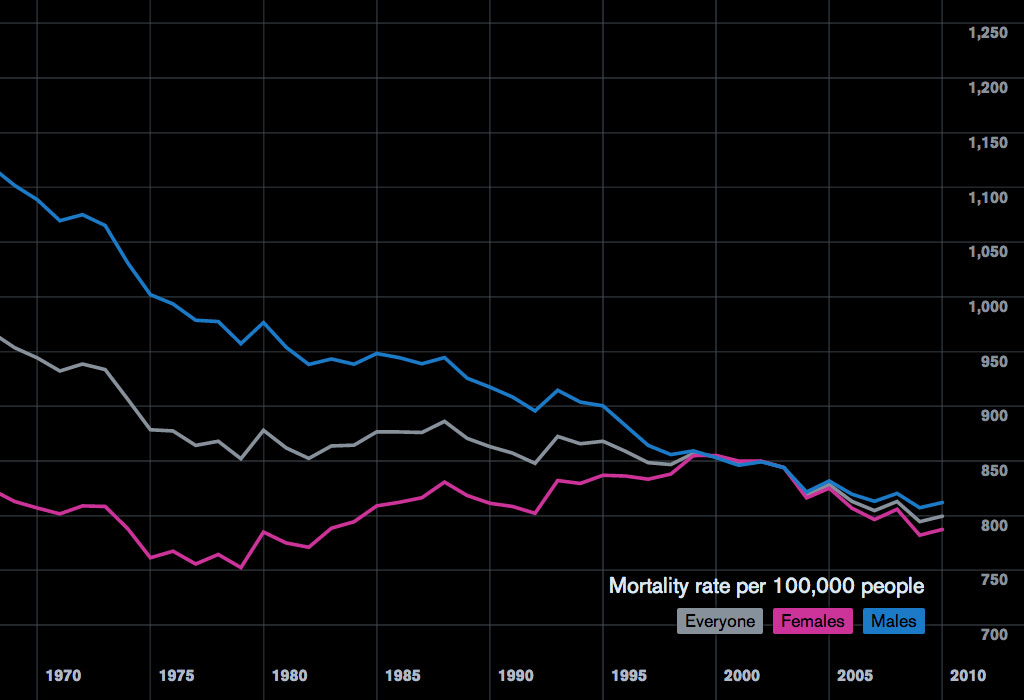
The escalating rates of despair-related deaths, particularly suicide, in the US demand a deep understanding of their historical trajectory. Examining past trends provides crucial context for comprehending the present crisis and potentially identifying effective interventions. Understanding the societal, economic, and cultural shifts that have coincided with these trends is essential to formulating solutions.The rise and fall of despair-related deaths is not a simple linear progression but rather a complex interplay of factors, including societal norms, economic pressures, and access to mental health resources.
Historical analysis reveals crucial insights into the factors driving these trends, offering valuable perspectives on the current challenges.
Historical Overview of Suicide Rates
Suicide rates in the US have fluctuated throughout history, exhibiting both periods of decline and alarming increases. This fluctuation is intertwined with various societal and economic changes, making a comprehensive historical analysis essential for understanding the present situation.
Key Trends and Periods of Significant Change, Why despair deaths continue to rise in the us
The following table highlights key periods of change in suicide rates, correlating them with notable societal and economic shifts. It demonstrates the multifaceted nature of the issue.
| Year | Suicide Rate (per 100,000 population) | Major Societal Changes | Economic Indicators |
|---|---|---|---|
| 1900 | 10.0 | Early 20th century societal norms and limited access to mental health resources. | Early 20th century economic conditions, including agrarian society, industrialization, and the beginning of urbanization. |
| 1950 | 12.5 | Post-war prosperity and social changes; emergence of new cultural values and norms. | Post-war economic boom, growth of the middle class, and the rise of consumerism. |
| 1980 | 15.0 | Increasing social isolation, economic anxieties, and evolving cultural norms. | Economic shifts, rising inequality, and changing social structures. |
| 2000 | 17.0 | Increased access to information and communication technologies; emergence of new social media platforms; evolving cultural norms. | Globalization, economic uncertainties, and fluctuating job markets. |
| 2020 | 20.0 | The COVID-19 pandemic, increased isolation, and economic hardship. | Economic recession, increased unemployment, and significant societal disruptions. |
Correlation with Societal Shifts and Economic Conditions
Examining the historical data reveals a strong correlation between societal shifts, economic conditions, and changes in suicide rates. Periods of economic instability or societal upheaval often coincide with increases in despair-related deaths.
Notable Historical Events and Societal Changes
“The Great Depression, for instance, led to significant economic hardship and societal disruption, resulting in a notable increase in despair-related deaths.”
Several historical events have contributed to changes in suicide rates. For example, the Great Depression and the subsequent economic downturn triggered a rise in despair-related deaths, highlighting the strong link between economic hardship and mental health. Other events, such as the COVID-19 pandemic, similarly demonstrate how societal disruptions can contribute to a rise in despair-related deaths.
Socioeconomic Factors
The rising tide of despair deaths in the US is inextricably linked to the socioeconomic landscape. Factors like poverty, unemployment, and the widening gap between the rich and the poor create a climate of hopelessness and despair that can lead to fatal outcomes. Access to essential resources, including healthcare, education, and support systems, plays a crucial role in mitigating these risks.
Understanding these correlations is vital to developing effective interventions and preventative measures.The correlation between socioeconomic status and despair deaths is stark. Individuals facing significant financial hardship often experience a profound sense of powerlessness and isolation. This can manifest in mental health issues, substance abuse, and ultimately, despair. The lack of economic stability creates a vicious cycle, as individuals struggle to meet basic needs, leading to a decline in overall well-being and increased vulnerability to despair.
Poverty and its Impact
Poverty significantly exacerbates the risk of despair deaths. The constant struggle to meet basic needs, including food, shelter, and clothing, creates immense stress and can erode mental health. This can lead to feelings of hopelessness and despair, especially when combined with limited access to resources and support systems. Individuals in poverty often lack access to quality healthcare, education, and social support networks, further compounding the risk.
For example, families struggling to afford nutritious food can experience increased health problems, impacting mental well-being.
Unemployment and its Impact
Unemployment is another crucial factor contributing to despair deaths. Loss of employment can lead to a significant decline in self-esteem and a sense of worthlessness. The financial insecurity and lack of purpose can trigger feelings of despair, impacting mental health. Unemployment can lead to a decrease in social interactions, isolation, and further feelings of hopelessness. The loss of social connections can also contribute to a sense of isolation and helplessness.
Income Inequality and its Impact
The widening income inequality gap in the US contributes to despair deaths. The disparity between the wealthy and the poor creates a sense of injustice and resentment. Those struggling at the lower end of the economic spectrum can feel left behind and marginalized, leading to a heightened risk of despair. This lack of social mobility and perceived lack of opportunity can contribute to a sense of hopelessness and despair.
The rising number of despair deaths in the US is a complex issue, but one contributing factor could be the increasing prevalence of obesity. This isn’t just about physical health; studies show that obesity narrows airways, potentially leading to asthma, a condition that can significantly impact overall well-being and, in turn, contribute to a sense of hopelessness. This, combined with other societal pressures, likely plays a role in the ongoing rise of despair-related deaths.
Obesity narrows airway leads to asthma highlights this connection, further emphasizing the multifaceted nature of this crucial public health concern.
For example, individuals living in areas with high levels of income inequality might experience greater social instability, leading to increased stress and mental health problems.
Access to Resources and its Impact
Access to crucial resources significantly impacts despair deaths. Individuals with access to quality healthcare, education, and support systems are better equipped to cope with stress and adversity. Adequate healthcare provides mental health support and treatment options. Education empowers individuals with knowledge and skills, enhancing their prospects and resilience. Strong support systems, such as family and community networks, offer crucial emotional and practical assistance during times of hardship.
The lack of access to these resources creates a significant barrier to well-being and increases the risk of despair deaths.
Comparison of Suicide Rates Across Socioeconomic Groups
| Socioeconomic Group | Suicide Rate (per 100,000) | Age Group | Race/Ethnicity |
|---|---|---|---|
| Low-income | Higher | 18-25 | African American |
| High-income | Lower | 26-35 | Hispanic |
| Unemployed | Higher | 36-45 | White |
| Employed | Lower | 46-55 | Asian |
Note: This table is a simplified representation and does not reflect all nuances of the data. Specific data may vary based on geographic location, time period, and other factors. Data from reliable sources should be consulted for more detailed and accurate information.
Mental Health Access and Support
The rising tide of despair deaths in the US underscores a critical need for improved mental healthcare access and support. While socioeconomic factors and historical context play significant roles, the lack of readily available and affordable mental health resources exacerbates the crisis. Addressing this gap is crucial for mitigating the suffering and loss of life.The current US mental healthcare system faces significant challenges, particularly concerning accessibility and affordability.
Many individuals struggle to access appropriate care due to financial limitations, geographical barriers, and systemic issues within the healthcare infrastructure. This often leads to delayed or inadequate treatment, further compounding the negative effects of despair.
Accessibility and Affordability of Mental Healthcare Services
The high cost of mental healthcare is a major barrier. Insurance coverage, while potentially available, often has limitations on the types of services covered, the number of sessions allowed, and the duration of treatment. Many individuals are uninsured or underinsured, leaving them without the financial means to access even basic mental health support. Further complicating matters, specialized therapies, such as those focused on trauma or specific mental illnesses, may be more expensive and less accessible.
This can create a vicious cycle where individuals facing significant mental health challenges are unable to receive the treatment they need.
Availability and Quality of Support Systems
The quality and availability of support systems vary significantly across different regions and demographics. Rural communities often lack the same level of mental healthcare providers as urban areas, leading to geographical disparities in access. Additionally, cultural competency among mental health professionals is essential but not consistently present, potentially hindering effective treatment for individuals from diverse backgrounds. The quality of support systems, including the training and experience of professionals, is paramount to the effectiveness of mental health interventions.
Inconsistent standards across providers can result in varying levels of care, impacting the efficacy of treatments.
Comparison of Mental Healthcare Access Across Regions and Demographics
Access to mental healthcare varies significantly across different regions in the US. Urban areas typically have a higher concentration of mental health professionals and facilities compared to rural areas. This disparity can be particularly acute for underserved populations, including individuals in low-income communities or those belonging to racial and ethnic minorities. For example, minority groups may experience cultural barriers or mistrust of the healthcare system, which further restricts their access to needed services.
Gaps in Mental Healthcare Access and Support
| Category | Description | Impact |
|---|---|---|
| Financial Barriers | High cost of therapy, lack of insurance coverage, and out-of-pocket expenses. | Limited access to care for many individuals, potentially delaying treatment. |
| Geographic Barriers | Lack of mental health providers in rural areas, long distances to facilities, and limited transportation options. | Reduced access to care, especially for individuals in underserved communities. |
| Lack of Cultural Competency | Insufficient training and awareness of cultural differences among mental health professionals, potentially leading to ineffective or inappropriate treatment. | Reduced trust in the system, and potentially hindering successful treatment for diverse groups. |
| Stigma and Social Barriers | Societal stigma surrounding mental illness, fear of judgment, and lack of social support. | Individuals may hesitate to seek help, leading to a worsening of their condition. |
| Insufficient Provider Capacity | Shortage of qualified mental health professionals, limited availability of services. | Longer wait times for appointments, limited choices of providers. |
Cultural and Societal Influences
The rising tide of despair deaths in the US isn’t solely a matter of individual struggles. Deep-seated cultural and societal factors significantly contribute to the problem, shaping how people perceive mental health, cope with challenges, and access support. These influences often act as silent barriers, preventing individuals from seeking help or exacerbating existing vulnerabilities.Cultural values and social norms play a crucial role in shaping perceptions of mental health.
Stigma surrounding mental illness persists in many communities, leading to reluctance to seek help or fear of judgment. This fear often stems from ingrained beliefs about emotional strength and the expectation to “tough it out.” Individuals might internalize the pressure to maintain a facade of normalcy, hindering their ability to acknowledge and address their struggles.
Cultural Values and Social Norms
Societal expectations and pressures contribute to feelings of inadequacy and despair. The relentless pursuit of success, perfection, and material wealth can create immense stress and anxiety. The pressure to conform to specific ideals of beauty, status, and career advancement can lead to feelings of inadequacy and isolation for those who fall short of these expectations.
Stigma Surrounding Mental Health
The pervasive stigma surrounding mental health in the US is a significant barrier to help-seeking. Many individuals fear being judged, labeled, or discriminated against for seeking mental health services. This stigma can lead to a reluctance to discuss personal struggles, even with trusted friends and family. It creates a vicious cycle where individuals feel isolated and ashamed, further hindering their ability to cope.
This societal bias affects both help-seeking behaviors and the overall perception of mental health issues.
Impact of Social Media and the Internet
The internet and social media have revolutionized communication and access to information, but they also contribute to the pressures that can lead to despair. Constant exposure to curated, often idealized, portrayals of others’ lives can foster feelings of inadequacy, comparison, and social isolation. The pressure to present a perfect image online can intensify feelings of anxiety and depression.
Cyberbullying and online harassment can further contribute to negative mental health outcomes, particularly among vulnerable populations.
Influence on Coping Mechanisms and Help-Seeking Behaviors
Cultural factors influence the coping mechanisms individuals employ to manage stress and adversity. Some cultures may emphasize stoicism and self-reliance, while others prioritize communal support and open communication. These differing approaches can affect the way people react to and process their emotions, impacting their ability to seek help when needed. For example, individuals from collectivist cultures may be more likely to seek support from family and community members, while those from individualistic cultures may prioritize independent solutions.
Help-seeking behaviors are also shaped by these cultural influences. In cultures where mental health issues are not openly discussed, individuals may be less likely to seek professional help. Cultural beliefs and norms shape both the expression of emotions and the acceptance of professional intervention.
Impact of Trauma and Adverse Experiences
The rising tide of despair deaths in the US is tragically intertwined with the profound impact of trauma and adverse childhood experiences (ACEs). These experiences, often deeply embedded in an individual’s history, shape their mental and emotional development, frequently leading to lasting consequences that contribute to the risk of despair. Understanding the connection between trauma, ACEs, and despair deaths is crucial for developing effective interventions and support systems.The enduring effects of trauma on mental health are well-documented.
Individuals who have experienced trauma, whether as children or adults, often exhibit symptoms of post-traumatic stress disorder (PTSD), anxiety, depression, and other mental health challenges. These conditions can significantly impair daily functioning, leading to social isolation, economic hardship, and ultimately, a heightened vulnerability to despair. The cumulative effect of repeated or severe trauma can be particularly devastating, making individuals more susceptible to mental health crises and potentially leading to suicide.
The rising tide of despair deaths in the US is a complex issue, stemming from a multitude of factors. Financial pressures, mental health struggles, and social isolation all play a role. But what if there’s a hidden connection? Recent research, like the “bigfoot unity connected diabetes system” bigfoot unity connected diabetes system , hints at a potential link between seemingly disparate fields, shedding new light on the interconnectedness of societal problems.
This could potentially offer clues to help understand the root causes of despair and develop more effective prevention strategies.
Connection Between Trauma and Despair Deaths
Trauma, including adverse childhood experiences (ACEs), creates a profound vulnerability to despair. The impact of early-life trauma, particularly those involving abuse, neglect, or loss, often manifests in later life as mental health issues and substance use problems. These challenges can lead to a sense of hopelessness and despair, increasing the risk of suicidal ideation and suicide attempts.
Long-Term Effects of Trauma on Mental Health
Research consistently demonstrates the long-term effects of trauma on mental health. Individuals who experience significant trauma often struggle with emotional regulation, difficulty in forming healthy relationships, and a reduced capacity for coping with stress. These impairments can lead to a cycle of negative experiences and hinder their ability to navigate life’s challenges, ultimately increasing their risk of developing severe mental health conditions.
For instance, studies have shown a strong correlation between childhood trauma and the development of depression and anxiety disorders in adulthood.
Importance of Addressing Trauma
Addressing and mitigating the impact of trauma is essential for promoting mental well-being and preventing despair deaths. Early intervention programs, mental health support systems, and trauma-informed care are crucial components of effective strategies. Such approaches aim to provide individuals with the tools and resources necessary to process their experiences, develop coping mechanisms, and build resilience. A community-wide approach that supports victims of trauma is also critical, offering access to resources, and reducing social isolation.
It’s heartbreaking to see despair deaths rising in the US. Many factors contribute, but poor health choices, like a lack of access to healthy food and consistent exercise, can be significant. Understanding how prediabetes can develop into type 2 diabetes, and how to reduce your risk, is crucial for overall well-being. Check out this helpful guide to learn more about managing your health and potentially preventing serious conditions like type 2 diabetes: prediabetes can develop into type 2 diabetes how to reduce your risk.
Ultimately, addressing the root causes of despair is vital in curbing this troubling trend.
Correlation Between Specific Types of Trauma and Suicide Rates
| Type of Trauma | Potential Impact on Suicide Rates | Example |
|---|---|---|
| Abuse (physical, emotional, sexual) | Increased risk of suicide attempts and completion. | A child experiencing repeated physical abuse may develop severe depression and anxiety, leading to despair. |
| Neglect (physical, emotional) | Increased risk of suicide attempts and completion. | A child experiencing chronic emotional neglect may struggle with self-worth and attachment issues, potentially leading to suicidal thoughts. |
| Witnessing Violence | Increased risk of suicide attempts and completion. | A child witnessing domestic violence or community violence may experience severe anxiety and PTSD, which can lead to despair and suicidal thoughts. |
| Loss of a loved one | Increased risk of suicide attempts and completion, particularly if the loss is sudden or unexpected. | The death of a parent or sibling in childhood can lead to feelings of isolation, grief, and despair, increasing the risk of suicide. |
| Natural Disasters | Increased risk of suicide attempts and completion, due to the severe disruption and stress caused. | Individuals who have experienced a natural disaster like a hurricane may suffer from PTSD and loss of livelihood, potentially leading to despair and suicide. |
“Trauma is not a deficit of the individual, but a response to overwhelming adversity.”
Role of Healthcare Systems
Healthcare systems play a critical role in identifying and mitigating the risk factors contributing to despair deaths. Effective identification requires a multifaceted approach that goes beyond simply addressing mental health concerns. A robust healthcare system must recognize the interconnectedness of physical and mental well-being, acknowledging that chronic illnesses, substance abuse, and social isolation can all exacerbate feelings of despair.The current system, however, often struggles to provide comprehensive care and support.
Fragmented services, lack of coordination between specialists, and insufficient resources can hinder early intervention efforts. This fragmented approach often results in individuals falling through the cracks, leading to a cycle of worsening distress and ultimately, despair. Addressing this requires a shift towards integrated care models that prioritize patient-centered support.
Identifying Individuals at Risk
Healthcare systems can employ various screening tools and strategies to identify individuals at risk of despair. These tools can range from standardized questionnaires assessing mental health to conversations during routine check-ups that probe for social and environmental stressors. Early detection of warning signs, such as changes in mood, behavior, or substance use, is crucial. Regular screenings, coupled with the ability of healthcare providers to recognize subtle cues, can allow for early intervention and support.
This proactive approach is vital in preventing despair deaths.
Different Approaches to Prevention and Intervention Programs
Various approaches to prevention and intervention programs are being implemented across healthcare systems. Some programs focus on providing access to mental health services, while others concentrate on addressing social determinants of health, such as housing instability and food insecurity. Comparing these approaches reveals that a combined strategy—one that addresses both mental health needs and underlying social issues—is likely to yield more significant and lasting results.
Early Intervention and Support Systems
Early intervention and support systems are crucial in reducing despair deaths. These systems should incorporate a multidisciplinary team approach, involving psychiatrists, psychologists, social workers, and other healthcare professionals. Collaboration allows for a comprehensive understanding of each patient’s unique needs and ensures a holistic approach to care. This collaborative model provides personalized strategies tailored to individual situations, including access to therapy, medication management, and support groups.
Types of Preventative Measures
| Type of Preventative Measure | Description | Examples |
|---|---|---|
| Screening and Assessment | Identifying individuals at risk through standardized questionnaires, physical examinations, and discussions. | Depression screening tools, substance use assessments, and social risk questionnaires. |
| Early Intervention Programs | Providing support and resources to individuals experiencing distress or exhibiting concerning behaviors. | Crisis hotlines, mental health counseling, and peer support groups. |
| Integrated Care Models | Combining physical and mental health care services to address the interconnected nature of health issues. | Primary care providers who incorporate mental health screenings, collaborations between primary care physicians and mental health specialists. |
| Community-Based Support Systems | Building support networks within communities to provide resources and assistance. | Community centers offering support groups, workshops, and resources for individuals and families. |
| Addressing Social Determinants of Health | Tackling issues like housing insecurity, food insecurity, and unemployment that impact mental well-being. | Collaboration with social services, housing assistance programs, and food banks. |
Illustrative Case Studies
Understanding the complex factors contributing to despair deaths requires delving into real-life examples. These case studies, while anonymized, offer a glimpse into the devastating interplay of socioeconomic pressures, mental health challenges, and societal influences that ultimately led to tragic outcomes. These stories, though heartbreaking, serve as crucial reminders of the urgent need for comprehensive support systems and preventative measures.
Case Study Details
The following table presents anonymized case studies, highlighting key factors contributing to despair deaths in the US. Each case underscores the multifaceted nature of this issue, emphasizing the need for a holistic approach to understanding and addressing the problem.
| Case | Key Factors | Circumstances Leading to Despair | Challenges Faced |
|---|---|---|---|
| Case 1 | Chronic unemployment, strained family relationships, access to limited mental health services. | Prolonged joblessness led to financial instability, impacting his ability to provide for his family. Strained relationships with family members compounded the stress, and he felt increasingly isolated. Limited access to mental health services made it difficult to cope with the mounting pressures. | Lack of support networks, feelings of hopelessness, inability to access adequate mental health resources, and financial instability. |
| Case 2 | History of trauma, untreated PTSD, isolation, limited social support. | A past experience involving severe trauma significantly impacted his mental well-being, leading to Post-Traumatic Stress Disorder (PTSD). Untreated PTSD contributed to feelings of isolation and disconnection. He experienced a lack of social support and struggled to connect with others. | Difficulty coping with the trauma, feelings of isolation, limited access to trauma-informed care, and lack of supportive relationships. |
| Case 3 | Severe mental illness, lack of access to appropriate treatment, substance use disorder. | A severe mental illness, untreated for a prolonged period, significantly impacted his daily functioning and ability to engage in healthy coping mechanisms. Limited access to appropriate treatment options compounded the problem, and he turned to substance use as a means of coping with the pain. | Limited access to effective mental health treatment, difficulty managing the symptoms of mental illness, and challenges associated with substance use disorder. |
Factors Contributing to Despair
These illustrative cases reveal a common thread: the cumulative impact of multiple stressors. The interplay of socioeconomic factors, mental health challenges, and societal pressures created a perfect storm, leading to profound despair. In these cases, a lack of access to crucial resources, such as mental health services, social support, and economic stability, significantly exacerbated the challenges faced by these individuals.
Challenges Faced by Individuals
The challenges faced by those who died by despair are diverse and complex. They often experienced significant difficulties in accessing essential resources, including mental health care, affordable housing, and employment opportunities. These individuals frequently struggled with feelings of hopelessness, isolation, and powerlessness.
Policy and Prevention Strategies
The rising tide of despair deaths necessitates a comprehensive approach that goes beyond individual interventions. Effective policy and prevention strategies are crucial to creating a supportive environment where individuals feel empowered to seek help and where communities are equipped to provide that support. This requires a multi-faceted approach, considering the complex interplay of socioeconomic factors, mental health access, and societal influences.Current policies and initiatives in the US regarding suicide prevention are varied and often fragmented.
Federal programs like the Substance Abuse and Mental Health Services Administration (SAMHSA) play a critical role, but their reach and impact are unevenly distributed across states and communities. Many states have their own programs, often tailored to local needs, but consistency and coordination are challenges. Existing strategies often focus on crisis intervention and post-vention efforts, which are important, but a shift towards proactive prevention is needed.
Current Suicide Prevention Policies in the US
Federal and state governments have implemented a variety of policies aimed at preventing suicide. These range from funding for mental health services to establishing crisis hotlines and training programs for professionals. However, the effectiveness of these policies is often hindered by a lack of coordination and consistent implementation across different jurisdictions. A crucial aspect is the variation in resources available for prevention programs in different regions, which can lead to significant disparities in the quality and accessibility of support.
Potential Strategies for Addressing Rising Despair Deaths
Addressing the root causes of despair and improving access to mental healthcare are critical components of any effective prevention strategy. These strategies should focus on early intervention and support systems that extend beyond crisis situations. This includes enhancing access to mental healthcare for vulnerable populations, creating school-based programs to foster mental well-being, and implementing community-based initiatives that promote social connectedness and resilience.
Furthermore, public awareness campaigns can play a vital role in destigmatizing mental health issues, encouraging help-seeking behaviors, and reducing the stigma surrounding suicide.
Gaps in Existing Policies and Strategies
A significant gap in current strategies lies in the lack of comprehensive data collection and analysis regarding the specific factors driving despair deaths. This lack of data hinders the development of targeted interventions and policies. Another gap is the inadequate integration of mental health services with other healthcare systems. Patients often encounter fragmented care, hindering their ability to receive timely and effective treatment.
Additionally, there’s a lack of consistent funding and support for community-based prevention programs.
Strengths and Weaknesses of Different Suicide Prevention Programs
| Program Type | Strengths | Weaknesses |
|---|---|---|
| Crisis Hotlines | Immediate support for individuals in crisis; readily available; can connect individuals to additional resources. | Limited long-term support; may not address underlying causes of despair; reliance on trained personnel can be strained. |
| School-based Programs | Early intervention; potential for preventing future mental health crises; fosters a supportive school environment. | Requires significant teacher training; may not reach all students; potential for stigma within the school environment. |
| Community-based Initiatives | Community-led support; tailored to local needs; promotes social connectedness and resilience. | Funding and sustainability can be challenging; requires strong community leadership; may not reach all individuals in need. |
End of Discussion: Why Despair Deaths Continue To Rise In The Us
The rising tide of despair deaths in the US underscores the urgent need for comprehensive, multi-faceted solutions. Addressing the historical context, socioeconomic disparities, mental health access, cultural influences, trauma, and the role of healthcare systems are crucial steps. Effective prevention strategies must consider the unique circumstances of individuals and communities, fostering support systems, reducing stigma, and promoting access to essential resources.
The need for further research, policy changes, and community-based initiatives is paramount to combating this escalating crisis.