Why men and women need different treatment guidelines for obesity hypertension and diabetes – Why men and women need different treatment guidelines for obesity, hypertension, and diabetes is a critical issue. These diseases affect men and women differently due to biological factors, treatment responses, lifestyle influences, diagnostic criteria, and mental health considerations. Understanding these nuances is essential for creating effective and equitable healthcare strategies.
This discussion delves into the biological underpinnings of these differences, examining how hormones, metabolism, and genetics impact disease development and response to treatment. We’ll explore potential variations in treatment efficacy, the role of lifestyle factors, and the unique challenges faced by men and women in managing these conditions. Finally, we’ll consider the broader public health implications of these insights and the importance of creating sex-specific guidelines for optimal care.
Biological Differences
Understanding the nuanced physiological differences between men and women is crucial for tailoring effective treatment guidelines for obesity, hypertension, and diabetes. These differences stem from variations in hormone levels, metabolic pathways, and even genetic predispositions, impacting how individuals respond to these conditions. Ignoring these variations can lead to suboptimal outcomes and potentially exacerbate health disparities.The intricate interplay of hormones and genetics significantly influences how men and women process and store energy, regulate blood pressure, and respond to insulin.
These differences are not simply qualitative but quantitative, meaning the actual amounts and effects of these processes can vary. This knowledge is essential for crafting personalized interventions that address the specific needs of each gender.
Hormonal Influences on Metabolism
Sex hormones, particularly estrogen and testosterone, play pivotal roles in regulating body composition and metabolic processes. Estrogen, prevalent in women, often promotes fat distribution in the hips and thighs, while testosterone, more prominent in men, tends to promote fat deposition around the abdomen. This difference in fat distribution is linked to varying levels of insulin sensitivity and susceptibility to metabolic disorders.For example, women often exhibit a higher level of insulin sensitivity in the presence of estrogen, which is a protective factor.
However, during menopause, the reduction in estrogen can lead to increased visceral fat and decreased insulin sensitivity, making women more vulnerable to developing type 2 diabetes. Men, with their predominantly testosterone-driven metabolism, tend to store more visceral fat, increasing their risk for metabolic syndrome.
Metabolic Pathways and Disease Development
Different metabolic pathways in men and women contribute to varying responses to obesity, hypertension, and diabetes. Women often have higher levels of adiponectin, a hormone that promotes insulin sensitivity, whereas men often have higher levels of inflammatory markers, potentially impacting blood pressure regulation. These differences can impact disease development and progression.Furthermore, women may experience unique hormonal fluctuations throughout their lives, such as during pregnancy and menopause, which can affect their metabolic profile and susceptibility to these diseases.
These hormonal fluctuations often influence the progression and severity of these conditions.
Different treatment guidelines for obesity, hypertension, and diabetes in men and women are crucial because of varying hormonal and physiological responses. Just like the complexities of healthcare disparities, the reasons behind why prison officials aren’t treating inmates for hepatitis C are equally troubling. This neglect, unfortunately, mirrors the lack of tailored treatment plans for conditions like these in different demographics, which underscores the need for personalized care in both situations.
Ultimately, personalized medicine remains essential for effective management of these conditions in all populations.
Genetic Variations and Disease Risk
Genetic variations between men and women can significantly impact their susceptibility to developing obesity, hypertension, and diabetes. Specific genes involved in metabolism, blood pressure regulation, and insulin sensitivity may exhibit different expression levels in men and women. This can lead to differing disease risks and progression rates.For example, research suggests that certain genetic polymorphisms associated with increased body fat may manifest differently in men and women, potentially impacting how they respond to dietary interventions.
Further investigation is needed to fully understand the role of these variations.
Body Composition Differences and Disease Susceptibility
| Characteristic | Men | Women | Impact on Disease Susceptibility |
|---|---|---|---|
| Fat Distribution | More abdominal fat | More subcutaneous fat | Increased risk of cardiovascular disease and type 2 diabetes in men due to central adiposity. Women may experience increased risk during and after menopause. |
| Muscle Mass | Generally higher | Generally lower | Higher muscle mass in men can buffer against some metabolic effects. Women may have a higher risk of sarcopenia (muscle loss) as they age. |
| Basal Metabolic Rate | Generally higher | Generally lower | Higher BMR in men means they might require more energy intake, potentially impacting weight management strategies. |
| Hormonal Influences | Predominantly testosterone | Predominantly estrogen | Varying hormonal profiles throughout the lifespan impact metabolism and susceptibility to diseases. |
These differences in body composition, coupled with varying hormonal and metabolic pathways, highlight the importance of considering sex-specific factors in the diagnosis, treatment, and prevention of obesity, hypertension, and diabetes. Individualized approaches are vital to achieve optimal health outcomes.
Treatment Response Variations
Understanding how men and women respond differently to obesity, hypertension, and diabetes treatments is crucial for tailoring effective and personalized care. While biological differences are a significant factor, treatment response variability also plays a key role in optimizing outcomes. This variability arises from several interconnected factors, including differences in medication absorption, metabolism, and the body’s physiological response to various interventions.The efficacy of treatments can vary significantly between men and women, necessitating adjustments to dosage and potentially different therapeutic approaches.
This personalized approach is vital to ensuring optimal health outcomes and minimizing adverse effects.
Medication Absorption and Metabolism Differences
Varied absorption and metabolism rates of medications can lead to different treatment responses in men and women. Hormonal differences, specifically estrogen levels, can affect the liver’s ability to process certain drugs. This can influence the concentration of the active compound in the bloodstream, potentially impacting treatment effectiveness and safety. For example, some medications might require higher doses in women due to faster metabolism, leading to suboptimal outcomes if dosages aren’t adjusted accordingly.
Treatment Efficacy in Different Sexes
Different medications and lifestyle interventions show varying efficacy in men and women. For instance, some blood pressure medications might be more effective in women than in men, while others might exhibit a more pronounced effect in men. Lifestyle modifications, such as dietary changes and exercise, also show varying responses depending on sex. Individualized approaches are crucial to maximize treatment outcomes.
Factors Influencing Treatment Response
Several factors influence treatment response variability. These factors include, but are not limited to, age, weight, overall health status, concurrent medical conditions, and genetic predisposition. These factors can interact with gender-specific differences in medication metabolism and response, resulting in unpredictable outcomes if treatment plans aren’t adjusted accordingly. This underscores the need for careful monitoring and personalized treatment strategies.
Medication Dosage Adjustments
| Condition | Potential Dosage Differences (Men vs. Women) | Rationale |
|---|---|---|
| Hypertension | Some blood pressure medications might require higher doses in women to achieve similar blood pressure control | Estrogen can influence the metabolism of certain drugs, affecting their effectiveness. |
| Diabetes | Insulin sensitivity and response to oral hypoglycemic agents might differ. | Hormonal differences and varying body composition can influence glucose regulation and medication response. |
| Obesity | Weight loss medications might have varying efficacy and side effect profiles. | Differences in body composition and fat distribution may affect the effectiveness of weight loss strategies. |
Note that these are potential differences and individual responses vary widely. Close monitoring and adjustment of treatment plans are crucial to achieve desired outcomes.
Treatment Adherence and Gender
Gender-related factors, including social expectations, cultural norms, and emotional responses, can impact treatment adherence. For instance, women might experience greater stress related to treatment regimens or side effects, impacting their ability to adhere to prescribed therapies. Conversely, men may be less likely to engage in self-care activities or seek support systems, which can also hinder adherence. Understanding these social and psychological factors is crucial for developing interventions that support successful treatment adherence in both men and women.
Lifestyle Factors
Beyond the biological differences, societal and environmental factors play a crucial role in shaping health disparities between men and women regarding obesity, hypertension, and diabetes. These conditions are not solely determined by genetics; lifestyle choices, deeply intertwined with social and cultural contexts, significantly impact risk and outcomes. Understanding these influences is critical for developing effective and equitable treatment strategies.Lifestyle factors, encompassing diet, exercise, stress management, and socioeconomic factors, interact in complex ways to influence the prevalence and management of these chronic diseases.
The differing experiences and priorities of men and women within their respective social and cultural environments lead to distinct patterns of disease development and management.
Social and Cultural Influences on Prevalence, Why men and women need different treatment guidelines for obesity hypertension and diabetes
Cultural norms and societal expectations often dictate dietary habits and activity levels, which can contribute to differing prevalence rates between men and women. For instance, some cultures may encourage higher consumption of processed foods or limit physical activity for women, increasing their risk for obesity and related conditions. Conversely, certain cultural norms may encourage strenuous physical activity in men, but may not offer the same support for women in maintaining those levels of activity.
This can be a factor in hypertension development.
Impact of Lifestyle Choices on Disease Risk
Men and women may respond differently to dietary interventions. Women might experience greater challenges in maintaining dietary restrictions due to family responsibilities or societal pressures to conform to specific beauty standards. Similarly, access to resources for stress management may vary, impacting their ability to cope with chronic stress and the subsequent effects on their blood pressure and blood sugar regulation.
Role of Socioeconomic Status, Healthcare Access, and Cultural Norms
Socioeconomic status significantly impacts access to healthy foods, safe environments for physical activity, and quality healthcare. Lower socioeconomic status often correlates with limited access to nutritious foods, leading to higher rates of obesity and related diseases in both men and women. Additionally, cultural norms regarding healthcare utilization and preventative measures can affect seeking medical attention for these conditions.
For example, some cultures might emphasize self-reliance and discourage seeking medical help for non-acute conditions, which could result in delayed diagnosis and treatment.
Understanding why men and women need different treatment guidelines for obesity, hypertension, and diabetes is crucial for effective care. Recent research highlights the varying physiological responses in men and women to these conditions, making personalized approaches essential. This is further complicated by the fact that new brain cells continue to form even as you age, as shown by recent studies , impacting how our bodies process and react to treatments.
Ultimately, acknowledging these differences in biological makeup remains key to developing successful, individualized strategies for managing these conditions in men and women.
Unique Challenges and Support Needs
Men often face unique barriers in seeking help for chronic conditions like hypertension and diabetes. Societal pressures may discourage men from expressing emotional vulnerability or discussing health concerns, leading to delayed or inadequate treatment. Women, on the other hand, may face time constraints and emotional stress from family and work responsibilities, hindering their ability to adhere to prescribed treatment plans.
Potential Lifestyle Interventions Tailored for Men and Women
| Lifestyle Intervention | Specific Needs for Men | Specific Needs for Women | Strategies |
|---|---|---|---|
| Dietary Modifications | Focus on reducing processed foods and increasing lean protein intake, with clear guidelines for portion sizes. | Address concerns related to body image and societal pressures, focusing on balanced meal planning, mindful eating, and healthy portion control. | Individualized meal plans, cooking demonstrations, support groups, and access to affordable healthy foods. |
| Exercise Programs | Tailor programs to accommodate work schedules and social commitments, emphasizing the importance of physical activity for overall well-being. | Offer programs that acknowledge the potential for time constraints and family responsibilities, including activities that can be incorporated into daily routines. | Gym memberships, community-based exercise programs, and flexible workout schedules. |
| Stress Management Techniques | Encourage the exploration of stress-reducing activities like sports, mindfulness exercises, or hobbies, fostering a supportive environment for stress management. | Provide access to resources that address specific stressors related to family and work responsibilities, including counseling and support groups. | Workshops on mindfulness, meditation, and relaxation techniques, and access to mental health professionals. |
Diagnostic Differences

The path to effective treatment for obesity, hypertension, and diabetes often starts with accurate diagnosis. However, existing diagnostic criteria and testing protocols sometimes fail to account for the biological differences between men and women. This can lead to delayed or misdiagnosis, impacting treatment efficacy and potentially exacerbating health disparities. Understanding sex-specific nuances in these conditions is crucial for personalized medicine.Diagnostic approaches frequently rely on standardized reference ranges developed predominantly from male populations.
Consequently, these ranges may not accurately reflect the physiological norms of women, leading to inconsistencies in diagnosis and treatment decisions. This underscores the critical need for sex-specific diagnostic criteria and testing protocols. A significant challenge lies in identifying and addressing potential biases embedded within current approaches.
Sex-Specific Diagnostic Criteria for Obesity
Differences in body composition and fat distribution between men and women often influence the interpretation of body mass index (BMI). Women tend to have a higher percentage of body fat compared to men at the same BMI. Using BMI alone to diagnose obesity in women may lead to misclassification, as it doesn’t account for these biological variations. Clinical assessment, including waist circumference and body fat percentage, becomes crucial for a more comprehensive evaluation.
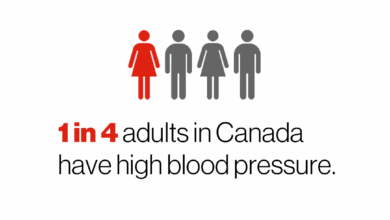
Sex-Specific Diagnostic Criteria for Hypertension
Hypertension, or high blood pressure, can present differently in men and women. Women may experience a higher risk of developing hypertension during pregnancy or in association with certain hormonal fluctuations. Diagnostic protocols should account for these variations, considering potential hormonal influences and the specific context of a woman’s health history. The importance of identifying and addressing underlying causes of hypertension in women cannot be overstated.
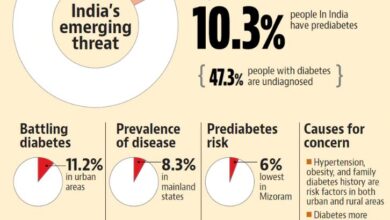
Sex-Specific Diagnostic Criteria for Diabetes
The presentation of diabetes mellitus also varies between men and women. Women may exhibit different symptoms and experience a different response to treatment. This is partly due to hormonal factors, and variations in the disease’s pathophysiology. The presence of comorbidities, like polycystic ovary syndrome (PCOS), can influence the diagnosis and management of diabetes in women.
Potential Biases and Gaps in Existing Diagnostic Approaches
Existing diagnostic approaches often rely on data primarily derived from male populations. This can lead to diagnostic biases and inaccuracies when applied to women. For instance, reference ranges for blood pressure, glucose levels, and other markers might not reflect the physiological norms of women. Furthermore, the focus on symptomatic presentation may not be equally comprehensive for men and women, resulting in missed diagnoses or delayed interventions.
Importance of Sex-Specific Reference Ranges for Diagnostic Tests
Establishing sex-specific reference ranges for diagnostic tests is essential for accurate diagnosis. These ranges would better reflect the physiological differences between men and women. This approach would enhance diagnostic precision and reduce the likelihood of misdiagnosis or delayed interventions. By incorporating sex-specific data, medical professionals can provide more targeted and effective treatments.
Potential Impact of Gender on Disease Presentation and Symptom Expression
The way men and women experience symptoms can vary significantly, impacting the likelihood of early detection. For instance, women may experience different symptoms or different degrees of severity for a particular condition compared to men. This difference in symptom expression may lead to delayed diagnosis, as healthcare providers might not be aware of these variations. Therefore, comprehensive assessments should consider gender-specific factors and symptoms to ensure timely and accurate diagnoses.
Table: Diagnostic Criteria for Obesity, Hypertension, and Diabetes (Sex-Specific Considerations)
| Condition | Men | Women | Sex-Specific Considerations |
|---|---|---|---|
| Obesity | BMI ≥ 30 kg/m2 | BMI ≥ 30 kg/m2; consider waist circumference and body fat percentage | Women tend to have higher body fat percentage at a given BMI. |
| Hypertension | Systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg | Systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg; consider hormonal fluctuations and pregnancy. | Hormonal fluctuations and pregnancy can influence hypertension development in women. |
| Diabetes | Fasting blood glucose ≥ 126 mg/dL or HbA1c ≥ 6.5% | Fasting blood glucose ≥ 126 mg/dL or HbA1c ≥ 6.5%; consider hormonal factors and comorbidities like PCOS. | Hormonal factors and associated comorbidities can influence the presentation and management of diabetes in women. |
Mental Health Considerations
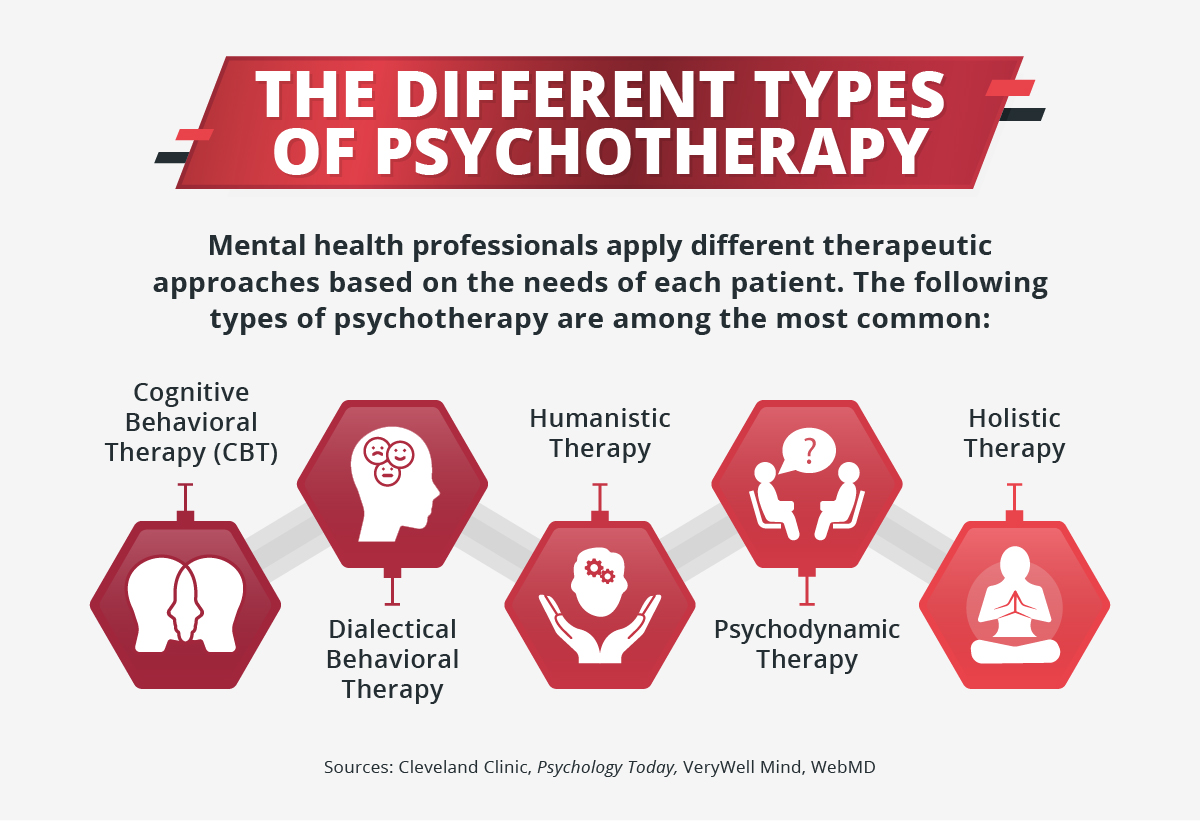
The interplay between mental well-being and chronic conditions like obesity, hypertension, and diabetes is profound and often overlooked. Addressing the emotional and psychological aspects of these diseases is crucial for effective management and improved patient outcomes. The relationship extends beyond simple correlation; mental health issues can significantly impact the development and progression of these conditions, while the conditions themselves can exacerbate existing mental health concerns.
This complex interplay warrants tailored treatment strategies that consider gender-specific nuances.Understanding the mental health landscape surrounding these conditions necessitates acknowledging potential differences in how men and women experience and cope with these challenges. Societal expectations and gender roles play a pivotal role in shaping these experiences, often leading to disparate mental health outcomes. Furthermore, culturally sensitive approaches to mental health interventions are essential to ensure equitable care and support for all individuals.
Relationship Between Mental Health and Chronic Conditions
Mental health significantly influences the development and management of obesity, hypertension, and diabetes. Stress, anxiety, and depression can impact dietary choices, physical activity levels, and medication adherence, ultimately affecting the progression of these conditions. Conversely, the chronic stress associated with managing these conditions can contribute to the development or exacerbation of mental health issues. This cyclical relationship underscores the need for integrated care models that address both physical and mental health needs simultaneously.
Gender Differences in Mental Health Challenges
Men and women may face different mental health challenges when dealing with obesity, hypertension, and diabetes. Societal expectations regarding masculinity often discourage men from seeking help for mental health concerns, leading to a potential underdiagnosis and delayed intervention. Women, on the other hand, may experience increased stress related to managing multiple roles and responsibilities, potentially leading to higher rates of anxiety and depression.
Different treatment guidelines for obesity, hypertension, and diabetes in men and women are crucial because their bodies react differently to various factors. Just as understanding how our internal body clocks impact treatment, like in using your body clock to treat cancer , is becoming increasingly important, hormonal differences, metabolic rates, and other biological variations mean personalized approaches are essential.
This tailored care ensures the best outcomes for each gender, addressing the unique needs of both men and women.
These gendered experiences highlight the importance of tailoring interventions to address specific needs and vulnerabilities.
Influence of Gender Roles and Societal Expectations
Gender roles and societal expectations significantly impact mental health outcomes. Traditional gender roles often dictate that men suppress emotions and avoid seeking help, potentially exacerbating existing mental health issues related to chronic conditions. Women, often burdened with multiple roles and responsibilities, may experience increased stress, which can contribute to heightened levels of anxiety and depression. These expectations must be acknowledged and addressed in treatment strategies.
Importance of Culturally Sensitive Mental Health Interventions
Culturally sensitive mental health interventions are critical for effective care. Cultural norms and beliefs significantly influence how individuals perceive and respond to mental health challenges. Treatment strategies must consider these cultural factors to ensure that interventions are not only effective but also culturally appropriate and acceptable. For example, interventions in certain cultures might require incorporating traditional healing practices alongside Western medicine.
Addressing Mental Health Needs in Treatment Plans
Integrating mental health considerations into treatment plans for obesity, hypertension, and diabetes is crucial for achieving optimal outcomes. Treatment plans should include screening for mental health issues, offering counseling or therapy, and connecting patients with appropriate support services. This approach recognizes the interconnectedness of physical and mental health and acknowledges the significant impact of mental health on disease management.
Regular assessment and adjustment of treatment plans, based on patient feedback and progress, are key to addressing mental health needs effectively.
Public Health Implications: Why Men And Women Need Different Treatment Guidelines For Obesity Hypertension And Diabetes
Recognizing and addressing the unique health needs of men and women is crucial for effective public health initiatives. Ignoring these differences can lead to disparities in treatment outcomes and hinder overall progress in combating chronic diseases like obesity, hypertension, and diabetes. A gender-sensitive approach, incorporating sex-specific treatment guidelines, promises a more equitable and impactful approach to public health.Understanding the disparities in disease prevalence, progression, and response to treatment between men and women is essential for developing targeted and effective public health interventions.
This requires not only a nuanced understanding of biological factors but also the consideration of socioeconomic, cultural, and environmental influences that shape health behaviors and access to care.
Sex-Disaggregated Data Collection and Analysis
Effective public health interventions demand accurate and comprehensive data. Collecting and analyzing health data with a focus on sex-disaggregated information is crucial for understanding the specific burden of chronic diseases in different genders. This data-driven approach enables public health officials to tailor interventions, resource allocation, and preventive strategies to address the unique needs of both men and women.
By analyzing trends and patterns in disease prevalence, progression, and treatment response across genders, public health initiatives can be optimized for greater impact. This also helps to identify specific populations at higher risk and allows for the development of targeted programs.
Tailoring Public Health Campaigns
Public health campaigns should be designed to resonate with the specific needs and experiences of both men and women. For instance, campaigns focusing on weight management might use different messaging and imagery for men and women, acknowledging diverse cultural backgrounds and social norms. Tailored campaigns can improve engagement and adherence to recommended health practices. A public awareness campaign focused on diabetes prevention, for example, could include specific messages targeting men and women, addressing their unique concerns and lifestyle factors.
Role of Public Health Professionals
Public health professionals play a critical role in promoting gender-sensitive healthcare. Their responsibility extends beyond awareness campaigns to include advocacy, education, and collaboration with healthcare providers. Public health professionals should actively participate in developing and implementing sex-specific treatment guidelines and promoting their use in clinical practice. They also need to ensure healthcare providers have the training and resources to provide gender-sensitive care.
Public health professionals should collaborate with community organizations to create culturally relevant health initiatives that address the specific challenges faced by men and women in their respective communities.
Public Health Strategies
| Strategy | Gender-Specific Considerations for Obesity, Hypertension, and Diabetes |
|---|---|
| Prevention Programs | Tailor programs to address unique risk factors for men and women. For example, programs targeting stress management might incorporate different approaches for men and women, considering their respective social and cultural contexts. |
| Early Detection and Screening | Ensure that screening guidelines are adapted for both genders. For example, the appropriate age and frequency of hypertension screening might differ for men and women due to variations in disease presentation. |
| Access to Care and Support | Develop strategies to improve access to healthcare services for both men and women, taking into account potential barriers like affordability, geographic location, and cultural norms. This might involve establishing mobile health clinics or partnering with community organizations. |
| Community-Based Interventions | Design community-based interventions that reflect the diverse needs and circumstances of men and women within specific communities. For example, community health workers could be trained to provide culturally appropriate health education and support to specific genders. |
Final Wrap-Up
In conclusion, recognizing the biological, behavioral, and societal factors that influence the presentation and management of obesity, hypertension, and diabetes in men and women is paramount. Tailoring treatment guidelines to address these sex-specific differences is not just beneficial but essential for improving health outcomes. This approach acknowledges the complex interplay of biology, lifestyle, and mental well-being, ultimately leading to more effective and equitable care for all.