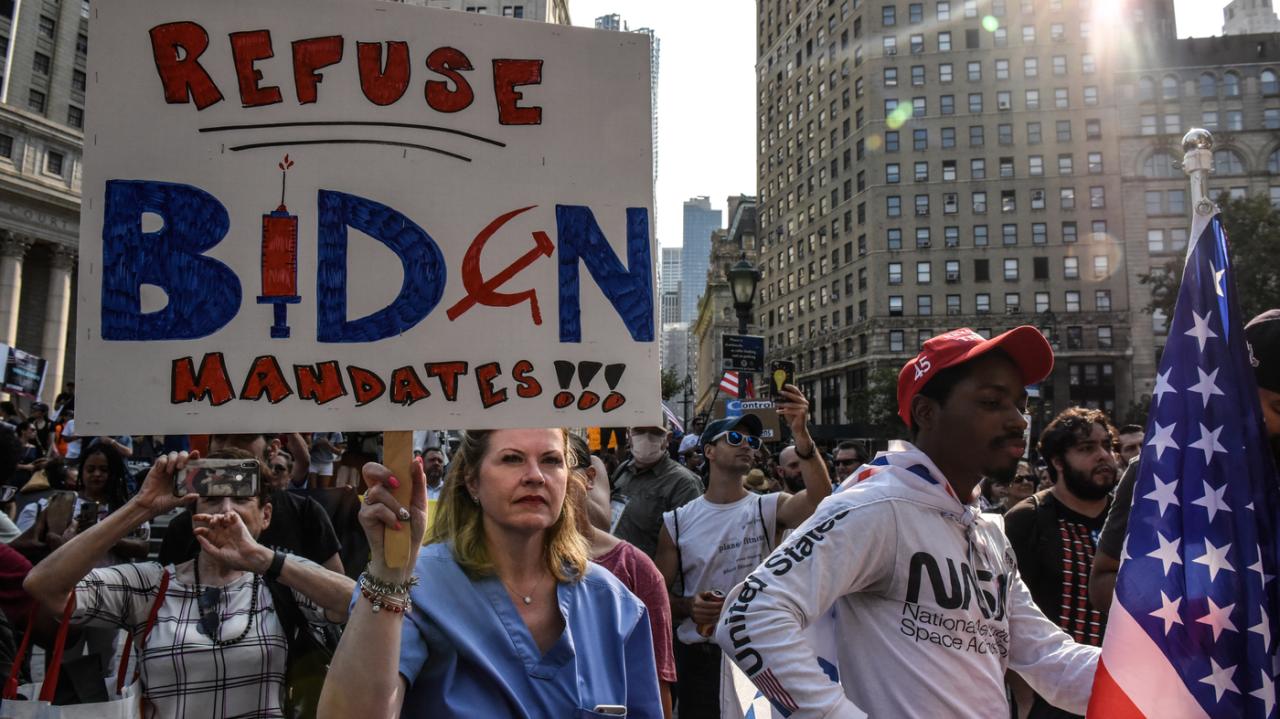
Will unvaccinated people face barriers to medical care? This complex question explores the potential for different types of medical care – from preventative checkups to emergency room visits – to be affected by vaccination status. The discussion delves into potential access, affordability, and perceived risk factors, while also considering societal attitudes and how these factors may impact treatment protocols.
The potential ramifications of restricting medical care for unvaccinated individuals extend far beyond individual health, affecting public health measures, vaccination rates, and potentially vulnerable populations. A comprehensive analysis examines historical precedents, international experiences, and alternative solutions, ultimately aiming to foster a balanced understanding of this sensitive issue.
Defining the Scope of “Barriers”

The question of whether unvaccinated individuals face barriers to medical care is multifaceted. It’s not a simple yes or no answer but rather a complex interplay of access, affordability, perceived risk, and societal attitudes. This exploration delves into the various types of medical care and how vaccination status might impact each.The spectrum of medical care is broad, ranging from preventative measures like vaccinations and check-ups to emergency interventions and elective procedures.
While the question of whether unvaccinated individuals will face barriers to medical care is complex, it’s important to remember that overall health choices, like opting for sugary drinks like fruit juice flavored coffee, can significantly impact your well-being. Recent research, as highlighted in this insightful article on how fruit juice flavored coffee doesn’t matter—drinking any sugary beverage increases diabetes risk , demonstrates the crucial link between lifestyle and health outcomes.
Ultimately, prioritizing healthy habits could potentially lessen any future obstacles to care for anyone.
Understanding the specific types of care and the potential barriers associated with each is crucial to a comprehensive assessment.
While the question of whether unvaccinated individuals will face barriers to medical care remains a hot topic, it’s interesting to consider the parallels with other seemingly ‘alternative’ health approaches. For example, nutritionists are now saying that the science behind the blood type diet, a popular but unsubstantiated method, isn’t supported by research. Nutritionists say science doesn’t back blood type diet.
This highlights the importance of relying on credible scientific evidence, regardless of whether it’s about vaccination status or dietary choices. Ultimately, access to quality medical care should be based on sound medical practice, not on personal beliefs.
Types of Medical Care and Potential Barriers
Different types of medical care necessitate varying levels of access and resources. Preventative care, designed to maintain health and prevent illness, often involves routine check-ups, screenings, and vaccinations. Emergency care, responding to sudden and serious health issues, requires immediate access to resources. Elective care, such as surgeries and procedures not considered urgent, requires a different set of considerations.
- Preventative Care: This category includes vaccinations, routine check-ups, and screenings. Barriers to access might include geographical limitations, lack of transportation, or limited availability of healthcare providers specializing in preventative care. Affordability issues can arise from the cost of these services, particularly for those without insurance. Perceived risk, influenced by misinformation or mistrust of healthcare providers, might lead some to forgo preventative measures.
Societal attitudes can affect the willingness of healthcare facilities to accommodate those with differing vaccination statuses, potentially leading to refusal of service.
- Emergency Care: This involves situations requiring immediate medical attention, such as accidents, strokes, or severe allergic reactions. Barriers to access include delayed response times, lack of readily available emergency medical services in remote areas, and potential discrimination based on vaccination status. Affordability concerns could arise if emergency services or treatments require significant out-of-pocket expenses. Perceived risk, often amplified in emergency situations, could affect the willingness of healthcare professionals to treat unvaccinated individuals.
Societal attitudes, particularly in high-stress situations, could influence how emergency services are allocated or provided.
- Elective Care: This encompasses procedures and surgeries not considered urgent, such as cosmetic procedures, joint replacements, or specific surgeries. Barriers to access might include scheduling delays, limited availability of specialized healthcare providers, and potential discrimination by medical facilities. Affordability concerns center on the significant costs associated with these procedures. Perceived risk could play a role in a patient’s decision to pursue elective care, especially if concerns about vaccination status influence treatment protocols.
Societal attitudes towards vaccination could influence the treatment protocols offered by facilities and even lead to the refusal of elective care for individuals with certain vaccination histories.
Potential Barriers Categorized
A detailed examination of potential barriers reveals complexities arising from access, affordability, perceived risk, and societal influence. These factors interact in various ways, creating a nuanced understanding of the challenges faced by unvaccinated individuals seeking medical care.
| Type of Medical Care | Access | Affordability | Perceived Risk | Societal Influence |
|---|---|---|---|---|
| Preventative | Geographical limitations, lack of transportation, limited provider availability | Cost of services, lack of insurance | Misinformation, mistrust of providers | Healthcare facility policies, willingness to accommodate |
| Emergency | Delayed response times, limited access in remote areas | High out-of-pocket expenses, cost of treatment | Amplified risk perception, potential discrimination | Resource allocation, provider judgment |
| Elective | Scheduling delays, limited provider availability, potential discrimination | High cost of procedures, out-of-pocket expenses | Concerns about treatment protocols, vaccination status impact | Facility policies, treatment protocol variations |
Historical Precedents and Analogies: Will Unvaccinated People Face Barriers To Medical Care
The debate surrounding access to medical care based on vaccination status sparks comparisons to past societal divisions. Examining historical precedents can offer valuable insights into the potential ramifications of such distinctions, particularly concerning the legal and ethical implications. These parallels can illuminate how similar policies were implemented in the past, their outcomes, and the potential challenges and controversies they engendered.
Understanding these historical echoes is crucial for navigating the complexities of the current discourse.Historical segregation and discrimination, often rooted in prejudice and fear, offer cautionary tales. Past policies that restricted access to services based on factors like race, religion, or socioeconomic status highlight the potential for similar harm if access to vital healthcare is limited based on vaccination choices.
The potential for creating further societal divides and undermining public health necessitates a careful and nuanced approach to the vaccination debate.
Examples of Historical Distinctions in Access to Services
Historical events reveal instances where access to services was restricted based on various factors. The segregation policies of the Jim Crow South, for example, denied certain groups equal access to education, housing, and healthcare, showcasing the devastating consequences of discriminatory practices. These precedents demonstrate the profound impact of policies that limit access to essential resources based on arbitrary distinctions.
Furthermore, historical cases of quarantine and isolation based on perceived health risks provide a context for understanding the contemporary debate. These past measures, while sometimes motivated by public health concerns, also reveal the potential for misuse and abuse, as well as the critical need for balanced considerations of individual liberty and societal well-being.
Similarities and Differences in the Vaccination Debate
Examining the current vaccination debate through the lens of historical precedents reveals striking similarities and notable differences. Both situations often involve public health concerns, but they also differ significantly in their contexts and potential consequences. While past examples often involved explicit discrimination, the current debate centers on individual choices and public health goals, which is a critical distinction.
However, the potential for misapplication of historical precedent and creating a new form of social division is a crucial concern.
Legal and Ethical Implications of Historical Parallels, Will unvaccinated people face barriers to medical care
The potential legal and ethical implications of restrictions on medical care based on vaccination status are substantial. Historical precedents suggest that such policies can be vulnerable to legal challenges based on equal protection clauses and potentially create an environment ripe for discrimination. The ethical considerations include balancing individual autonomy with public health concerns. The need to uphold individual rights while maintaining public health is paramount.
Historical precedents illustrate the difficulty of this balance.
While the FDA’s recent approval of a new drug for episodic cluster headaches, like this one , is a huge win for sufferers, it raises questions about potential future access disparities. Will unvaccinated people face barriers to medical care, especially when new treatments emerge? It’s a complex issue with lots of different perspectives, and the answers are still developing.
This new medication is a promising step forward, but we need to ensure equitable access to it, and to other medical advancements, for everyone.
Table: Historical Examples and Their Similarities to the Vaccination Debate
| Historical Context | Similarities to Vaccination Debate | Differences from Vaccination Debate | Legal/Ethical Implications |
|---|---|---|---|
| Jim Crow South (1877-1965) | Restricted access to resources based on race. | Focus on vaccination status, not race. | Potential for discrimination lawsuits; violation of equal protection. |
| Quarantine of individuals with contagious diseases (various periods) | Public health concerns about the spread of illness. | Focus on voluntary action versus mandatory measures. | Potential for misuse and overreach; balancing individual rights with public health. |
| Immigration restrictions based on perceived health risks (various periods) | Restriction of access based on perceived health concerns. | Focus on voluntary action to prevent spread of disease. | Potential for discriminatory practices; balancing public health with individual rights. |
Potential Impacts on Public Health
Restricting medical care for unvaccinated individuals raises complex concerns about public health. Such policies, while seemingly targeted at individual choices, can have far-reaching consequences, impacting disease transmission, vaccination rates, and the overall well-being of communities, especially vulnerable populations. This section delves into the potential ramifications of such a strategy.
Impact on Disease Outbreaks
Restricting medical care for unvaccinated individuals could potentially hinder the timely and appropriate treatment of infectious diseases. This could lead to a greater likelihood of disease outbreaks, especially if the unvaccinated population is significant. The resulting surges in cases could overwhelm healthcare systems, leading to longer wait times for all patients and potentially compromising the quality of care.
A significant example is the impact of measles outbreaks in communities with low vaccination rates. Measles can cause severe complications and death, particularly in vulnerable populations, and outbreaks can rapidly spread throughout a region. The increased workload on healthcare resources due to these outbreaks can further strain the system and affect the treatment of other conditions.
Impact on Vaccination Rates and Herd Immunity
Policies that restrict access to medical care for unvaccinated individuals might inadvertently affect vaccination rates. A sense of mistrust in the health system could arise, potentially leading to lower vaccination rates in the general population. This can erode herd immunity, making the entire community more susceptible to outbreaks. A decrease in herd immunity means fewer people are protected from contagious diseases, creating a higher risk for widespread infections and outbreaks.
Herd immunity, a critical component of public health, relies on a significant portion of the population being immunized to protect those who cannot be vaccinated.
Impact on Vulnerable Populations
Restricting access to medical care for unvaccinated individuals can disproportionately affect vulnerable populations. These individuals often have pre-existing conditions or are otherwise more susceptible to serious illness. They might not have access to alternative healthcare options, potentially facing severe consequences if an outbreak occurs. For example, individuals with compromised immune systems or young children might be particularly vulnerable to the negative effects of reduced healthcare access for unvaccinated individuals.
Comparison of Scenarios
| Scenario | Disease Spread | Vaccination Rates | Impact on Vulnerable Populations |
|---|---|---|---|
| No restrictions on medical care for unvaccinated individuals | Potentially slower disease spread due to treatment of all individuals regardless of vaccination status, thus limiting the severity and duration of outbreaks. | Vaccination rates may remain relatively stable or may even increase as people see the value of vaccination. | Vulnerable populations are likely to receive timely and appropriate care, reducing their risk of severe illness or death. |
| Restrictions on medical care for unvaccinated individuals | Potentially faster disease spread and more severe outbreaks due to delayed or withheld treatment for unvaccinated individuals. | Vaccination rates may decrease as a result of perceived discrimination or lack of trust in the healthcare system. | Vulnerable populations may face significant risks due to delayed or denied treatment, increasing the likelihood of severe illness and death. |
International Perspectives and Experiences
Navigating the complexities of vaccination mandates and healthcare access requires a global perspective. Different countries have adopted various strategies for promoting vaccination and ensuring equitable access to medical care, each with unique impacts on public health and societal well-being. Understanding these diverse approaches can illuminate potential paths forward in addressing the current challenges.
Different Approaches to Vaccination
Various nations employ different strategies to encourage vaccination rates and maintain public health. Some countries utilize mandatory vaccination policies, while others rely on public health campaigns and incentivized programs. These diverse strategies reflect differing cultural values, socioeconomic factors, and historical contexts.
- Australia: Australia has a strong history of high vaccination rates, largely attributed to a combination of effective public health campaigns, readily available vaccines, and the integration of vaccination schedules into routine healthcare. The country has successfully mitigated outbreaks of preventable diseases.
- Israel: Israel, due to its high vaccination rates, has successfully managed COVID-19 outbreaks. This has been attributed to the swift rollout of vaccination programs and high public trust in the medical system. The proactive approach allowed for a swift return to normalcy, showcasing the potential of proactive vaccination programs.
- France: France, while generally having high vaccination rates, has faced challenges with hesitancy regarding specific vaccines. The government has implemented public health campaigns and educational initiatives to address concerns and promote vaccination. These efforts reflect the ongoing need to engage with and address public concerns regarding vaccination.
Comparative Analysis of Healthcare Access
Examining the healthcare access policies in different countries offers valuable insights. Different nations have adopted varying approaches to ensuring access to care for all citizens, including those who may have differing vaccination statuses. These differences can be attributed to a variety of factors, including socioeconomic structures and the strength of public health infrastructure.
- Canada: Canada’s universal healthcare system provides access to care for all citizens, regardless of their vaccination status. The system’s emphasis on equity and accessibility is reflected in its provision of care to all.
- United Kingdom: The UK’s National Health Service (NHS) offers comprehensive healthcare coverage. While vaccination status is not a primary factor in healthcare access, public health messaging and campaigns encourage vaccination. This approach demonstrates a focus on promoting public health alongside ensuring equitable access to care.
- United States: The US healthcare system presents a complex scenario, with varying levels of access depending on factors such as insurance coverage and geographic location. The debate around vaccination mandates has significantly influenced access to healthcare in certain sectors, highlighting the need for clear and consistent policies.
International Examples of Vaccination Policies
The table below presents international examples of vaccination policies and their impact.
| Country | Policy | Impact on Public Health | Societal Acceptance |
|---|---|---|---|
| Australia | High vaccination rates, mandatory vaccination for certain populations. | Effective control of preventable diseases. | High societal acceptance of vaccination. |
| Israel | Swift COVID-19 vaccination rollout, high public trust. | Effective management of COVID-19 outbreaks. | High societal acceptance of vaccination. |
| France | Public health campaigns, efforts to address vaccination hesitancy. | High vaccination rates but some challenges with specific vaccines. | Mixed societal acceptance. |
| Canada | Universal healthcare, vaccination not a barrier. | High vaccination rates, consistent with universal healthcare approach. | High societal acceptance. |
Addressing Misinformation and Public Concerns
Navigating the complex landscape of vaccination hesitancy requires understanding the anxieties and misconceptions driving public opposition. Misinformation, often amplified by social media, can significantly impact public perception, making it crucial to address these concerns proactively and with accurate information. This section explores common misconceptions, their potential impact on public perception of restrictions, and strategies to combat them, fostering trust and open communication between healthcare providers and patients.Misconceptions surrounding vaccination often stem from a combination of factors, including a lack of accurate information, fear of unknown side effects, and distrust in authority figures.
These anxieties can influence public opinion regarding restrictions on medical care for unvaccinated individuals, potentially leading to polarization and conflict. Developing strategies to counter misinformation is essential to maintaining public health and trust in the healthcare system.
Common Misconceptions about Vaccination
Addressing the underlying anxieties and concerns is paramount in countering misinformation and fostering open communication. Common misconceptions frequently surface in discussions about vaccination. These misconceptions often lead to misinformed decisions about vaccination status and potentially influence perceptions about restrictions on medical care.
- Safety Concerns: One common misconception is the belief that vaccines contain harmful ingredients, such as mercury or aluminum. Extensive scientific research has repeatedly debunked these claims, demonstrating the safety and efficacy of vaccines. The use of such ingredients is precisely controlled and regulated, ensuring their safety and minimizing potential adverse reactions.
- Effectiveness Concerns: Another prevalent misconception revolves around the perceived ineffectiveness of vaccines in preventing disease. Decades of research and real-world data have shown the remarkable effectiveness of vaccines in reducing the incidence and severity of infectious diseases. The global success in eradicating diseases like smallpox and significantly reducing the prevalence of others like polio and measles stands as a testament to their efficacy.
- Autonomy and Personal Choice: A core concern for many revolves around personal autonomy and the perceived infringement on individual rights by vaccination mandates. This concern often intertwines with fears about potential long-term health effects and the need for informed consent. This concern should be addressed with open dialogue and a clear explanation of the benefits and risks involved in vaccination, in a context of respecting individual choices while highlighting the community’s well-being.
- Government Conspiracy Theories: The proliferation of unfounded conspiracy theories surrounding vaccination is another major obstacle. These theories often allege a sinister agenda by governments or pharmaceutical companies, and they can create significant distrust in official health recommendations. Countering these theories requires a multi-pronged approach involving fact-checking, debunking false claims, and promoting transparent communication from credible sources.
Impact of Misconceptions on Public Perception
The prevalence of these misconceptions directly influences how individuals perceive restrictions on medical care for unvaccinated individuals. Fear and distrust can lead to resistance against such restrictions, fueling public debate and potentially hindering public health initiatives.
Strategies for Countering Misinformation
Combating misinformation requires a multifaceted strategy, focusing on education, transparency, and community engagement.
- Public Health Campaigns: Public health campaigns can effectively disseminate accurate information about vaccination safety and efficacy, addressing concerns directly and using trusted sources. This can include social media outreach, community events, and collaborations with influencers to deliver accurate information in easily accessible formats.
- Engagement with Healthcare Providers: Healthcare providers play a critical role in countering misinformation. Open and honest communication with patients about vaccination benefits and potential risks, as well as actively addressing their concerns, can foster trust and understanding. Healthcare professionals should be equipped with tools and resources to address questions about vaccine safety and effectiveness.
- Fact-Checking and Debunking: Rigorous fact-checking and debunking of false claims about vaccines are essential. Identifying and addressing misinformation on social media platforms is crucial to preventing the spread of inaccurate information. Collaborating with journalists and social media influencers to provide accurate information can help counter false narratives.
Promoting Open Communication and Understanding
Establishing trust and fostering open communication between healthcare providers and patients is crucial for successful vaccination programs. This requires a commitment to empathy, transparency, and responsiveness.
| Common Misconception | Potential Impact on Public Perception of Restrictions | Strategies for Countering Misconceptions |
|---|---|---|
| Vaccines contain harmful ingredients. | Resistance to vaccination mandates and restrictions on medical care. | Highlight extensive scientific research, regulatory oversight, and safety data. |
| Vaccines are ineffective. | Skepticism about the need for restrictions. | Showcase real-world data demonstrating vaccine efficacy and disease prevention. |
| Vaccination infringes on personal autonomy. | Opposition to any restrictions on access to medical care. | Emphasize informed consent, patient rights, and the community benefits of vaccination. |
| Government/Pharmaceutical conspiracy theories. | Deep distrust in official health recommendations. | Engage in transparent communication from trusted sources, debunking false claims. |
Alternative Solutions and Approaches
Navigating the complexities of vaccine hesitancy requires a multifaceted approach that goes beyond simply imposing restrictions. Focusing solely on punitive measures risks alienating segments of the population and potentially hindering broader public health goals. Instead, a comprehensive strategy encompassing education, community engagement, and accessible healthcare options is essential. This approach prioritizes informed decision-making and fosters trust in the medical community.Alternative solutions to addressing public health concerns related to unvaccinated individuals need to consider the reasons behind vaccine hesitancy.
Understanding the anxieties and concerns of individuals who choose not to be vaccinated is crucial to designing effective interventions. A one-size-fits-all approach will likely prove ineffective.
Strategies for Promoting Vaccination Without Imposing Barriers
Promoting vaccination effectively hinges on a multi-pronged strategy that goes beyond simply mandating vaccinations. It necessitates addressing the underlying factors contributing to vaccine hesitancy, such as misinformation and distrust. This approach emphasizes empowering individuals with accurate information and fostering a supportive environment for vaccination.
- Targeted Public Health Campaigns: Effective public health campaigns should focus on the specific concerns and anxieties of different communities. Employing diverse communication channels, including social media, community events, and trusted local leaders, can significantly increase vaccination rates. For example, culturally relevant messaging and community health fairs can improve accessibility and trust.
- Community Engagement and Education Initiatives: Collaborating with community leaders, healthcare providers, and trusted organizations can foster trust and encourage vaccination uptake. Interactive workshops, presentations, and Q&A sessions can address misconceptions and provide accurate information in a welcoming setting. Educational materials tailored to specific populations can further enhance understanding.
- Accessible Healthcare Options and Vaccination Clinics: Simplifying access to vaccination services is vital. Establishing mobile vaccination clinics, weekend clinics, and vaccination sites in diverse locations can improve accessibility for individuals with limited mobility or scheduling constraints. Partnering with employers to offer on-site vaccination programs can further increase convenience.
Potential Benefits and Drawbacks of Alternative Approaches
Alternative approaches to promoting vaccination, focusing on education and accessibility, offer several potential benefits. These approaches can build trust, address misinformation, and encourage informed decisions, potentially leading to higher vaccination rates without the negative repercussions of imposing barriers. However, these strategies require significant investment in resources and sustained effort.
- Benefits: Enhanced community engagement, increased trust in healthcare providers, greater understanding of vaccination benefits, and potential for long-term behavioral change. Addressing misinformation and promoting accurate information can also positively impact future vaccination campaigns.
- Drawbacks: These approaches may require significant time and resources. Success depends on the engagement of diverse stakeholders and community leaders. Effectiveness may vary depending on the specific population and the underlying reasons for vaccine hesitancy.
Comparing Effectiveness with Imposing Barriers
The effectiveness of alternative solutions to imposing barriers should be assessed in the context of both short-term and long-term outcomes. While imposing barriers may demonstrate immediate effects, it can also lead to long-term damage to community trust and hinder future vaccination efforts. Alternative approaches aim for more sustainable solutions that promote trust and understanding.
| Approach | Benefits | Drawbacks | Potential Effectiveness |
|---|---|---|---|
| Targeted Public Health Campaigns | Addresses specific concerns, builds trust | Requires significant resources, may not reach all | Moderate to High, dependent on targeting |
| Community Engagement and Education | Promotes informed decision-making | Requires community buy-in, time-consuming | High, if executed well |
| Accessible Healthcare Options | Increases convenience and accessibility | High initial investment, logistical challenges | Moderate to High, depends on location and population |
| Imposing Barriers | Potential for immediate impact | Erodes community trust, may lead to backlash | Low to Moderate, with potential for long-term damage |
Final Review
Ultimately, the debate surrounding vaccination status and access to medical care is multifaceted. While public health concerns are legitimate, the potential impacts on overall health outcomes and societal well-being must be carefully weighed against alternative approaches to vaccination promotion. This discussion necessitates a nuanced approach that balances the need for public health measures with the principles of equitable access to care.