
Women and insomnia why prescription sleep medications dont work that well – Women and insomnia: why prescription sleep medications don’t work that well. This deep dive explores the unique challenges women face with sleeplessness and why traditional sleep medications often fall short. We’ll uncover the specific hormonal, psychological, and societal factors that contribute to insomnia in women, and why current sleep aids may not address the root causes. We’ll also examine alternative approaches and strategies for finding effective solutions, moving beyond the limitations of prescription drugs.
From hormonal fluctuations during menstruation, pregnancy, and menopause to the unique stress levels and societal pressures women face, this article explores the complexities behind women’s sleep patterns. We’ll delve into how these factors influence the effectiveness of prescription sleep medications and why a one-size-fits-all approach often doesn’t work. This discussion will equip women with the knowledge and tools to navigate insomnia effectively and find lasting relief.
Understanding Women’s Insomnia
Insomnia, the persistent difficulty falling asleep, staying asleep, or experiencing restful sleep, is a prevalent issue impacting many individuals. However, the experience and contributing factors can vary significantly between genders. This exploration delves into the unique challenges women face with insomnia, examining the interplay of biological, psychological, and societal influences.Women experience insomnia at a higher rate than men, highlighting the need for tailored understanding and treatment approaches.
Women often struggle with insomnia, and sometimes prescription sleep medications just don’t cut it. This is often due to a complex interplay of factors, but a growing concern among medical professionals is the influence of patient influencers online. This phenomenon can lead to misdiagnosis and the inappropriate use of these medications, potentially causing more harm than good, especially for women with underlying health conditions.
Ultimately, the lack of effective sleep solutions for women is a critical issue that needs a multifaceted approach, moving beyond the simple prescription route.
This disparity isn’t simply about quantity; it’s also about the types of insomnia women encounter and the factors that contribute to it.
Prevalence and Gender Differences
Insomnia affects a substantial portion of the population, but studies indicate that women are disproportionately affected. This disparity is not fully understood, but may be linked to hormonal fluctuations, stress levels, and societal expectations. For example, research suggests that women report higher levels of sleep disturbances compared to men across various age groups.
Hormonal Influences
Hormonal fluctuations play a significant role in women’s sleep patterns. These fluctuations, linked to the menstrual cycle, pregnancy, and menopause, can disrupt the natural sleep-wake cycle. During menstruation, fluctuations in estrogen and progesterone can lead to difficulties falling asleep or staying asleep. Pregnancy brings about significant physiological changes that can affect sleep, including hormonal shifts, physical discomfort, and anxieties about the upcoming birth.
Menopause, marked by declining estrogen levels, often results in hot flashes, night sweats, and difficulty regulating body temperature, all of which can significantly impact sleep quality.
Stress and Societal Pressures
The societal pressures and expectations placed on women can contribute to heightened stress levels, which in turn can negatively affect sleep. Women often bear the responsibility for managing multiple roles—career, family, and household—leading to increased stress and anxiety, which can manifest as sleep disturbances. This multitasking can lead to chronic stress and subsequently affect sleep quality. Cultural expectations, such as the perceived need to appear constantly “together,” can contribute to the feeling of stress and pressure that interferes with sleep.
Impact of Pregnancy and Menopause
Pregnancy, a period of significant physiological changes, often results in sleep disturbances due to physical discomfort, hormonal shifts, and anxieties about the upcoming birth. For example, frequent urination, back pain, and discomfort in the abdomen can lead to frequent awakenings. Menopause, characterized by declining estrogen levels, frequently brings about hot flashes, night sweats, and difficulty regulating body temperature, all of which disrupt sleep.
Psychological Factors
Psychological factors like anxiety, depression, and post-traumatic stress disorder (PTSD) are significant contributors to insomnia in women, as they can disrupt the natural sleep-wake cycle. Women may experience these conditions at higher rates than men due to various factors, including societal pressures and unique life experiences. For example, studies suggest that women are more likely to report anxiety and depression, and these conditions can significantly affect sleep quality.
Sleep Needs and Architecture
Sleep needs and sleep architecture, the different stages of sleep, can vary between women and men. For instance, women might have a greater need for sleep than men, but this is not always consistent across all women. The differences in sleep patterns may not always be consistent and can vary greatly among individuals.
Sleep Disorders Specific to Women
Certain sleep disorders may be more prevalent in women than in men. For example, restless legs syndrome (RLS) is often more common in women, although this isn’t always a direct gender-specific issue. Understanding the factors that may contribute to these differences can help develop targeted strategies for diagnosis and treatment.
Prescription sleep meds often fall short for women battling insomnia, a complex issue that goes beyond simple chemical fixes. Recent research into gene therapy for cancer, like that discussed in gene therapy for cancer welcomed with reservations , highlights the nuanced nature of biological responses, which could offer valuable insights into the diverse physiological factors affecting women and their sleep struggles.
Ultimately, a deeper understanding of the individual experiences and unique needs of women is crucial for effective insomnia treatment.
Prescription Sleep Medications for Women: Women And Insomnia Why Prescription Sleep Medications Dont Work That Well
Prescription sleep medications, while sometimes necessary, can have significantly different effects on women compared to men. Understanding these differences is crucial for safe and effective use. This often stems from the complex interplay of hormonal fluctuations throughout a woman’s life, which impacts how her body metabolizes and responds to these medications.Many factors influence a woman’s response to sleep medications, including her age, overall health, and the specific medication prescribed.
The following sections delve into the details of these factors and their implications.
Types of Prescription Sleep Medications
Prescription sleep medications are often categorized based on their mechanism of action. Common types include benzodiazepines, non-benzodiazepines, and orexin receptor antagonists. Benzodiazepines, like temazepam and flurazepam, work by enhancing the effects of GABA, a neurotransmitter that promotes relaxation and sleep. Non-benzodiazepines, such as zolpidem and zaleplon, have similar effects but with a potentially different profile of side effects.
Orexin receptor antagonists, like suvorexant, work by targeting specific brain pathways involved in wakefulness.
Hormonal Fluctuations and Medication Response
Hormonal fluctuations throughout a woman’s life, including menstruation, pregnancy, and menopause, can significantly impact how her body processes sleep medications. These fluctuations can alter the metabolism of certain medications, leading to variations in their effectiveness and potential side effects. For example, during pregnancy, a woman’s liver function and kidney function may change, potentially affecting how quickly the medication is cleared from her system.
Medication Effects Across Different Age Groups
The effects of sleep medications can differ based on a woman’s age. Younger women may experience a different set of side effects than older women due to varying metabolic rates and overall health. For example, older women may be more susceptible to confusion, dizziness, and falls due to reduced liver and kidney function. The effectiveness of sleep medications may also vary depending on the stage of life a woman is in.
Potential Side Effects Specific to Women
Women may experience specific side effects from sleep medications not typically seen in men. These can include, but are not limited to, increased risk of daytime drowsiness, difficulty concentrating, and mood changes. Some women may also experience changes in their menstrual cycles, although this is less common. Furthermore, the risk of dependency and withdrawal symptoms may differ depending on a woman’s individual characteristics and how her body processes the medication.
Limitations of Current Prescription Sleep Medications
Current prescription sleep medications often have limitations, especially for women. These include the potential for side effects, such as rebound insomnia, and the lack of a truly long-term solution for chronic insomnia. Moreover, some medications may not be suitable for women with certain medical conditions. The effectiveness of these medications also varies significantly from person to person, meaning what works for one woman may not work for another.
Effectiveness Across Different Medications
Different sleep medications have varying degrees of effectiveness across different age groups and conditions. For example, some medications might be more effective in treating insomnia associated with anxiety in younger women, while others might be more suitable for older women with underlying health conditions. It is crucial to carefully consider the specific needs of each woman when selecting a sleep medication.
Why Prescription Sleep Medications Often Fail Women
Prescription sleep medications, while sometimes helpful, often fall short for women. This isn’t due to a lack of efficacy in the drugs themselves, but rather a complex interplay of factors unique to women’s physiology, lifestyle, and overall health. Understanding these factors is crucial for developing more effective and personalized treatment strategies.The effectiveness of prescription sleep medications can vary significantly from person to person.
Women often experience different responses to the same medication compared to men, and this variability isn’t always well understood or accounted for in clinical trials. This leads to a mismatch between the drug’s intended effect and the actual experience of the user, often resulting in disappointing outcomes.
Complex Interplay of Factors
Women’s bodies and health experiences differ greatly from those of men, and this translates into differing responses to medications. Hormonal fluctuations throughout the menstrual cycle, pregnancy, and menopause significantly impact neurotransmitter levels and sleep regulation. These changes, often unpredictable, can interfere with the effectiveness of sleep medications designed for a more consistent physiological profile.
Individual Differences in Medication Response
Individual responses to medications are highly variable. Factors like genetics, body weight, and existing health conditions influence how the body processes and metabolizes medications. Women, due to diverse genetic makeup, can process certain drugs at different rates than men. For example, women may metabolize certain sleep medications more slowly, leading to potentially higher and longer-lasting concentrations in the bloodstream, which can cause unwanted side effects or diminish the effectiveness of the medication.
Interactions with Other Conditions
Women are more prone to certain health conditions that can interact with sleep medications. Conditions like anxiety, depression, and chronic pain are more prevalent in women, and these conditions can affect how the body responds to sleep medications. Moreover, women are often taking multiple medications for various conditions, creating the potential for drug interactions that can impact sleep quality or even cause adverse health effects.
For instance, combining certain sleep medications with antidepressants can alter the efficacy of both drugs and potentially increase the risk of side effects.
Impact of Medication’s Chemical Composition
The chemical composition of a sleep medication can impact women differently. Certain molecules might interact differently with the unique hormonal profiles of women at various stages of their lives, potentially altering their effectiveness or side effects. For instance, the impact of a particular sleep medication on the neurotransmitters involved in sleep regulation might be influenced by hormonal changes.
This is a complex area requiring further investigation.
Comparison with Other Sleep Aids
While prescription sleep medications can be effective for some, other options may be more suitable for women. Natural remedies, relaxation techniques, and lifestyle changes can also play a significant role in improving sleep quality. For instance, consistent sleep hygiene practices, such as a regular sleep schedule and a relaxing bedtime routine, often have a positive impact on sleep quality for women.
Furthermore, cognitive behavioral therapy for insomnia (CBT-I) is a non-pharmacological approach that has shown promising results for addressing the underlying causes of insomnia, which may prove more sustainable and less reliant on medication.
Alternative Approaches to Insomnia for Women
Navigating insomnia can be challenging, especially for women. While prescription medications offer a temporary solution for some, they often come with side effects and don’t address the underlying causes. Fortunately, numerous non-pharmacological approaches can effectively manage insomnia and improve sleep quality without the risks associated with medication. This section explores various strategies to help women achieve restful sleep naturally.
Non-Pharmacological Approaches for Insomnia
Effective insomnia management often involves a multifaceted approach, incorporating lifestyle modifications, relaxation techniques, and potentially therapeutic interventions. A comprehensive strategy addresses both the immediate symptoms and the root causes of insomnia.
| Approach | Description | Effectiveness | Potential Side Effects |
|---|---|---|---|
| Relaxation Techniques (e.g., deep breathing, progressive muscle relaxation) | These techniques help reduce stress and anxiety, promoting a sense of calm before sleep. | Generally effective for reducing anxiety and promoting relaxation. | Minimal, if any. Potential for mild discomfort during some techniques. |
| Lifestyle Changes (e.g., regular sleep schedule, dietary adjustments, regular exercise) | Consistent sleep patterns, a balanced diet, and regular physical activity are crucial for optimal sleep. | Highly effective when implemented consistently. Improves overall health and well-being. | Potential for initial discomfort with dietary changes or increased activity, but benefits often outweigh the initial challenges. |
| Cognitive Behavioral Therapy for Insomnia (CBT-I) | CBT-I is a structured therapy that helps identify and modify negative thoughts and behaviors that contribute to insomnia. | Highly effective for addressing underlying psychological factors and creating healthier sleep habits. | Potential for initial emotional discomfort as negative thought patterns are challenged and restructured. Requires commitment to therapy sessions. |
| Alternative Therapies (e.g., acupuncture, herbal remedies) | These therapies aim to restore balance in the body and mind, potentially promoting relaxation and sleep. | Evidence for effectiveness is mixed and often varies based on the specific therapy. More research is needed. | Potential for allergic reactions to herbal remedies, discomfort during acupuncture sessions. Should be approached with caution and under the guidance of a qualified practitioner. |
Importance of Lifestyle Modifications
Lifestyle modifications are fundamental to effective insomnia management. Consistent sleep schedules, regular exercise, and a balanced diet can significantly impact sleep quality. For example, a woman who consistently goes to bed and wakes up around the same time, even on weekends, will often experience better sleep than someone with a fluctuating sleep schedule. This consistency helps regulate the body’s natural sleep-wake cycle, crucial for restful sleep.
Sleep Hygiene Practices
Prioritizing sleep hygiene is essential for improving sleep quality. Creating a conducive sleep environment, limiting caffeine and alcohol intake before bed, and avoiding screen time before sleep are vital components of sleep hygiene. A dark, quiet, and cool bedroom, free from distractions, can significantly improve sleep. Avoiding large meals or strenuous exercise close to bedtime is also important.
Cognitive Behavioral Therapy for Insomnia (CBT-I)
CBT-I is a highly effective, evidence-based treatment for chronic insomnia. It helps identify and modify negative thought patterns and behaviors that interfere with sleep. CBT-I often involves techniques like sleep restriction therapy, stimulus control therapy, and cognitive restructuring. This therapy can help women understand the factors contributing to their insomnia and develop strategies to improve their sleep.
For instance, if a woman consistently stays in bed when she can’t sleep, CBT-I can help her establish a more effective sleep-wake cycle.
Women often struggle with insomnia, and sometimes prescription sleep meds just don’t cut it. It’s frustrating, right? Sometimes, underlying issues like bladder problems can contribute to sleep disruption. For example, if you’re experiencing a leaky bladder, it could make it hard to get a good night’s rest. Check out girlfriends guide to a leaky bladder for helpful tips and solutions.
Ultimately, addressing the root causes, not just the symptom, is key to finding effective sleep solutions for women. Finding the right combination of strategies, including lifestyle changes and perhaps even exploring underlying health issues, is often necessary.
Alternative Therapies
Alternative therapies like acupuncture and herbal remedies are sometimes used to manage insomnia. However, the scientific evidence supporting their effectiveness is often limited. While some individuals may find these therapies helpful, it’s crucial to consult with a qualified healthcare professional before incorporating them into a treatment plan. For example, while some herbal remedies may promote relaxation, others might have adverse interactions with medications.
Strategies for Choosing Effective Sleep Aids
Finding the right sleep aid can feel like navigating a maze, especially when insomnia persists. Choosing a sleep aid is a deeply personal journey, requiring careful consideration of individual needs and potential risks. It’s not a one-size-fits-all solution, and understanding the nuances of various options is crucial for success.Effective sleep aid selection goes beyond simply reaching for a pill.
A multifaceted approach, incorporating lifestyle changes, stress management, and perhaps a carefully chosen sleep aid, often yields the best results. This involves a thorough understanding of the pros and cons of each option, potential side effects, and the importance of consulting a healthcare professional.
Comparison of Sleep Aids
Choosing a sleep aid requires careful consideration of potential benefits and drawbacks. A balanced approach involves evaluating both the effectiveness and potential side effects of various options. This comparison table provides a structured overview to aid in informed decision-making.
| Sleep Aid Type | Effectiveness | Potential Side Effects | Pros | Cons |
|---|---|---|---|---|
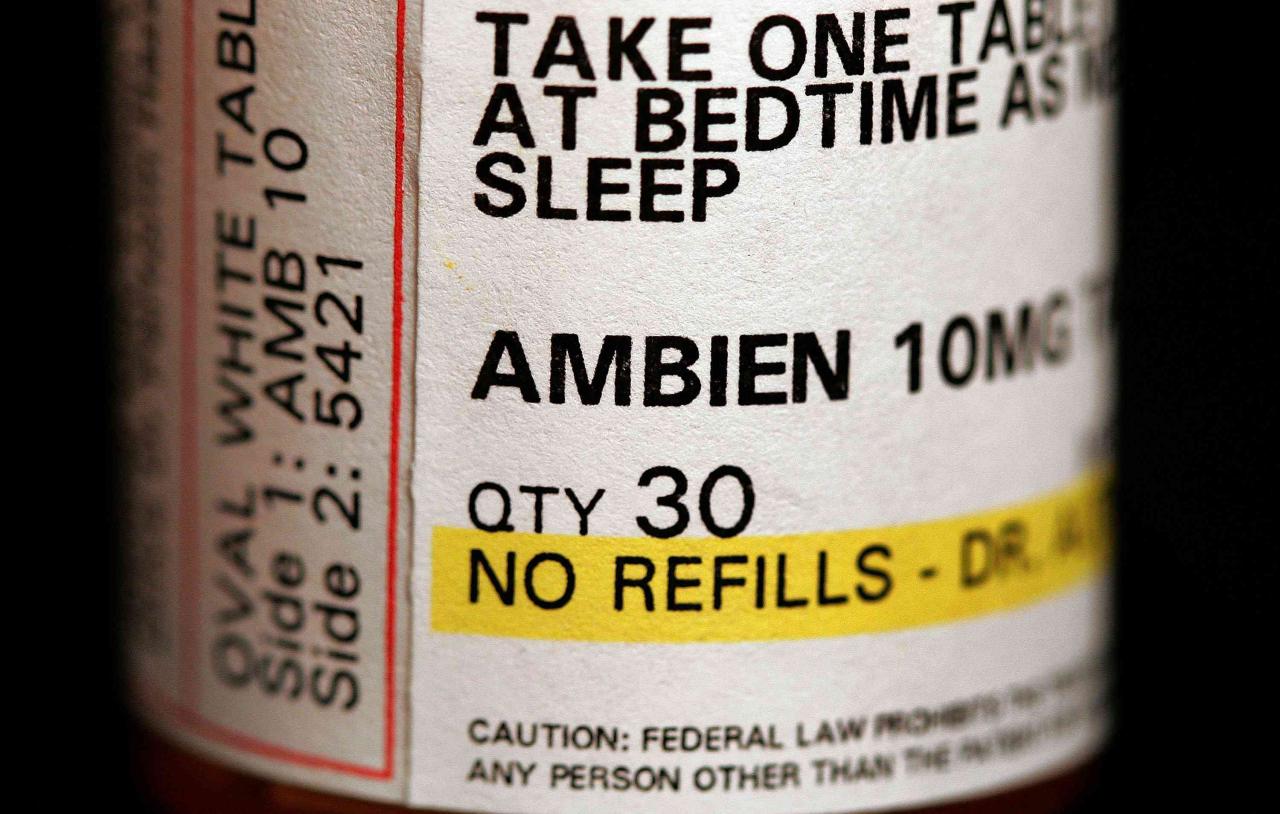
| Prescription Sleep Medications (e.g., Ambien, Lunesta) | Can be effective for short-term use in some cases. | Drowsiness, dizziness, headache, nausea, and potential for dependence and rebound insomnia. May interact with other medications. | May be helpful for acute insomnia. | Requires a prescription, carries potential risks, and may not be suitable for long-term use. |
| Over-the-Counter Sleep Aids (e.g., melatonin, diphenhydramine) | May provide some relief for mild insomnia. Melatonin may be particularly helpful for regulating circadian rhythms. | Drowsiness, dizziness, dry mouth, and potential for interactions with other medications. Diphenhydramine can cause significant daytime drowsiness. | Readily available and generally less expensive than prescription medications. | Limited effectiveness for severe insomnia; diphenhydramine can be less effective in women due to differences in metabolism. |
| Natural Remedies (e.g., chamomile tea, valerian root) | May promote relaxation and improve sleep quality for some individuals. | Generally mild, but potential for interactions with medications. Individual responses vary widely. | Generally considered safe and natural. | May not be as effective as other options for severe insomnia; results can be unpredictable. |
Factors to Consider When Choosing a Sleep Aid
Several factors influence the choice of a sleep aid. Understanding these factors allows for a more informed and tailored approach to improving sleep.
- Severity of Insomnia: Mild cases may respond well to natural remedies or lifestyle changes, while severe cases might require a prescription sleep aid.
- Underlying Medical Conditions: Certain medical conditions can affect sleep, and a sleep aid may not be the appropriate solution. A doctor can assess the impact of underlying conditions on sleep and recommend the best course of action.
- Current Medications: Interactions between sleep aids and other medications can occur, leading to undesirable side effects. A healthcare professional can identify potential interactions.
- Personal Preferences: Different sleep aids have varying effects on individuals. Experimentation with different options may be necessary to determine the most suitable choice.
- Lifestyle: Consider factors like work schedule, stress levels, and daily routine. Adjustments to these factors can also contribute to improved sleep quality.
Evaluating Sleep Aid Effectiveness
Monitoring the effectiveness of a sleep aid is crucial for determining its suitability. Regular assessment helps adjust strategies if needed.
- Tracking Sleep Patterns: Maintaining a sleep diary can track sleep quality and duration. This helps evaluate the aid’s impact on various aspects of sleep.
- Assessing Daytime Function: Notice any improvements or negative impacts on daytime energy levels and cognitive function. A sleep aid that impairs daytime function is less effective, despite providing sleep.
- Monitoring Side Effects: Regularly track any side effects, such as drowsiness or headaches. This helps determine if the benefits outweigh the risks.
- Consulting with a Healthcare Professional: Regular check-ins with a doctor are essential to adjust treatment strategies if needed.
Dangers of Multiple Sleep Aids
Combining multiple sleep aids can lead to dangerous side effects. Understanding the potential risks is essential for responsible sleep aid use.
Combining multiple sleep aids significantly increases the risk of adverse reactions and interactions, potentially leading to severe complications.
- Increased Side Effects: Combining multiple medications can exacerbate side effects, such as drowsiness, dizziness, or confusion. These effects can be compounded and potentially life-threatening.
- Medication Interactions: Multiple sleep aids can interact negatively with each other and other medications, leading to unpredictable outcomes. It’s crucial to disclose all medications to a healthcare professional.
Importance of Professional Consultation
Seeking professional guidance is essential before starting any sleep aid regimen. A healthcare provider can offer personalized advice and monitor progress.
- Individualized Recommendations: Healthcare professionals can assess individual needs and recommend the most appropriate sleep aid based on medical history, current medications, and other factors.
- Risk Assessment: Healthcare professionals can evaluate potential risks and side effects associated with different sleep aids.
- Monitoring Progress: Regular check-ins with a healthcare professional allow for monitoring treatment effectiveness and adjustments to the plan as needed.
Long-Term Impacts and Prevention
Chronic insomnia, when left unaddressed, can have significant and far-reaching consequences for women’s overall well-being. The impact extends beyond just feeling tired; it can affect physical health, mental health, and relationships. Understanding the potential long-term implications and developing preventative strategies are crucial for maintaining a healthy and fulfilling life.The long-term consequences of chronic insomnia in women are multifaceted and can significantly affect various aspects of their lives.
These consequences can include an increased risk of developing certain medical conditions, such as cardiovascular disease, type 2 diabetes, and obesity. Mental health issues, including anxiety and depression, are also more prevalent among women with chronic insomnia. Furthermore, difficulties concentrating, memory problems, and impaired judgment can affect work performance and daily functioning.
Potential Long-Term Health Consequences
Chronic insomnia can contribute to a variety of health problems. Studies have shown a correlation between prolonged sleep deprivation and an increased risk of developing certain medical conditions. For instance, individuals with chronic insomnia may experience elevated blood pressure and cholesterol levels, placing them at a higher risk for cardiovascular disease. Additionally, chronic insomnia can disrupt the body’s metabolic processes, potentially increasing the risk of type 2 diabetes.
Stress Management Techniques for Better Sleep, Women and insomnia why prescription sleep medications dont work that well
Effective stress management is crucial for promoting healthy sleep patterns in women. Techniques such as mindfulness meditation, deep breathing exercises, and progressive muscle relaxation can help reduce anxiety and promote a sense of calm before bedtime. These techniques can help to regulate the body’s stress response, leading to improved sleep quality. For example, incorporating 15 minutes of daily meditation can significantly reduce stress and improve sleep quality.
Importance of Maintaining a Healthy Sleep Schedule
Establishing and maintaining a consistent sleep schedule is vital for regulating the body’s natural sleep-wake cycle, also known as the circadian rhythm. Going to bed and waking up around the same time each day, even on weekends, helps synchronize the body’s internal clock and promotes better sleep quality. Consistency in sleep schedules is essential for ensuring the body’s natural sleep-wake cycle functions optimally.
This ensures a more restful sleep, leading to better overall health.
Role of Diet and Exercise in Sleep Quality
Diet and exercise play a significant role in promoting sleep quality. Avoiding large meals and caffeine or alcohol close to bedtime can help prevent disruptions to sleep. Regular physical activity, especially during the day, is also beneficial for sleep. For example, a balanced diet rich in fruits, vegetables, and whole grains, combined with regular exercise, can contribute to a healthier sleep cycle.
Creating a Supportive Sleep Environment
A conducive sleep environment is essential for promoting healthy sleep. This includes maintaining a cool, dark, and quiet bedroom. Using comfortable bedding and ensuring the room is well-ventilated can also contribute to a more relaxing sleep environment. A comfortable sleep environment, free from distractions, is essential for falling asleep easily and maintaining a restful sleep. For example, using blackout curtains or earplugs can help block out unwanted light and noise.
End of Discussion
In conclusion, women’s experiences with insomnia are multifaceted and often differ from men’s. While prescription sleep medications may offer temporary relief for some, they frequently fail to address the underlying causes of insomnia in women. This article highlights the need for personalized approaches, emphasizing alternative therapies, lifestyle modifications, and a deeper understanding of the intricate interplay of factors influencing women’s sleep.
By exploring non-pharmacological strategies and considering individual needs, women can actively take control of their sleep health and find effective solutions for lasting relief from insomnia.




