Women with heart disease get better treatment with female doctors, a fascinating finding that explores the potential benefits of gender-specific care. This deep dive delves into the prevalence of heart disease in women, the diagnostic disparities they face, and the unique perspectives of female physicians in addressing these issues.
Studies have shown that women often experience delayed diagnoses and potentially less effective treatments for heart disease compared to men. Possible explanations include differences in communication styles, cultural and social factors, and even potential biases within the medical system. This investigation examines these factors, drawing on research and patient experiences to paint a comprehensive picture of the challenges and solutions.
Understanding the Issue
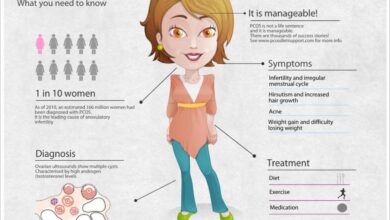
Heart disease, a leading cause of death globally, disproportionately impacts women, often manifesting differently and leading to delayed diagnosis and treatment compared to men. This disparity in care highlights a critical need for improved awareness and understanding of the unique challenges women face in managing their cardiovascular health. Recognizing these challenges is the first step toward equitable access to quality care and better outcomes.The prevalence of heart disease in women is not simply a matter of lower numbers; it’s a matter of different presentations and risk factors.
Understanding these differences is vital to identifying women at risk and ensuring timely interventions. Current research consistently demonstrates a pattern of delayed diagnosis and potentially less aggressive treatment for women experiencing cardiac events compared to their male counterparts. This disparity is rooted in multiple factors, including societal biases, healthcare system limitations, and even biological differences.
Prevalence of Heart Disease in Women
Women often experience heart disease with different symptoms than men. This can lead to misdiagnosis or delayed diagnosis, as women’s symptoms may be attributed to other conditions. For example, chest pain, a classic symptom in men, is not always present in women. Instead, women may experience shortness of breath, fatigue, or nausea. These less specific symptoms can be easily overlooked or dismissed, contributing to delayed diagnosis and treatment.
Disparities in Diagnosis and Treatment
Studies show significant disparities in the diagnosis and treatment of heart disease between men and women. These disparities are not simply a matter of statistical difference; they often reflect a pattern of underrecognition and undertreatment of women’s cardiovascular concerns. This can lead to poorer health outcomes for women.
Potential Reasons for Disparities
Several factors contribute to the disparities in heart disease diagnosis and treatment between men and women. These include implicit bias within the healthcare system, a lack of awareness of women’s unique presentation of symptoms, and the use of diagnostic tools calibrated primarily on male data. Furthermore, societal factors, such as women often being caregivers, can impact their ability to prioritize their own health and seek timely medical attention.
Research consistently shows that women are less likely to receive aggressive treatment for heart disease, despite having similar or even higher risks than men. This can be attributed to various factors, including implicit bias among healthcare professionals, different clinical guidelines, and a lack of understanding of women’s specific cardiovascular needs.
Studies show women with heart disease often get better outcomes when treated by female doctors. This highlights the importance of personalized care, and it’s fascinating to see how virtual reality is gaining traction in healthcare, offering new possibilities for patient engagement and education. Virtual reality gaining traction in healthcare could potentially enhance the experience for patients, making the overall process more comfortable and potentially leading to better results, mirroring the positive effects of female doctors.
Ultimately, focused, compassionate care, whether delivered through traditional methods or innovative technologies, benefits women facing heart disease.
Potential Biases in Medical Practices
Implicit biases in medical practices can contribute to disparities in heart disease care. For instance, healthcare providers may be more likely to attribute symptoms to non-cardiac causes in women, leading to delayed diagnosis and less aggressive treatment. Furthermore, studies have indicated that women are often under-referred for cardiac procedures compared to men with similar symptoms. These biases can stem from societal stereotypes and historical gender norms, impacting the quality of care women receive.
Impact on Women’s Health Outcomes
The disparity in heart disease diagnosis and treatment significantly impacts women’s health outcomes. Delayed diagnosis can lead to more severe disease progression, increased risk of complications, and poorer long-term survival rates. Furthermore, these disparities contribute to a higher mortality rate for women compared to men from cardiovascular disease.
Table of Heart Disease Disparities
| Disease Type | Prevalence in Women vs. Men | Common Diagnostic Delays |
|---|---|---|
| Coronary Artery Disease (CAD) | Women often experience atypical symptoms like shortness of breath or fatigue, leading to delayed diagnosis compared to men, who typically experience chest pain. | Misinterpretation of symptoms, under-referral for cardiac procedures. |
| Heart Failure | While both genders can develop heart failure, women often experience a different presentation, sometimes leading to misdiagnosis. | Delay in recognizing heart failure as a possible cause of symptoms. |
| Stroke | Women experience different risk factors and symptoms for stroke, often leading to delayed diagnosis. | Underestimation of stroke risk in women, misinterpretation of symptoms. |
Female Doctors’ Approach
Women often experience unique challenges when navigating the complexities of heart disease. Their experiences may differ from men’s, both in terms of symptoms and how their bodies respond to treatment. Understanding these nuances is crucial for ensuring women receive the best possible care. This section will explore how female doctors might offer a more tailored and effective approach to treating heart disease in women.Female doctors, by virtue of their shared experience as women, may bring a unique perspective to patient care.
This perspective can manifest in a heightened awareness of potential gender-based disparities in symptom recognition and treatment response. They might also foster a more empathetic and supportive environment, enabling women to feel more comfortable discussing their concerns and symptoms.
It’s great to see research showing women with heart disease often get better outcomes when treated by female doctors. However, it’s concerning that flavored tobacco use is on the rise again among teens, as reported in this article about flavored tobacco use rising again among teens. This highlights the need for more proactive strategies to address risky behaviors, and hopefully, this also translates to improved treatment for women’s health issues in general.
Potential Benefits of Female Doctors, Women with heart disease get better treatment with female doctors
Female doctors may have a better understanding of the female anatomy and physiology, particularly concerning heart disease. This understanding might lead to more accurate diagnoses and tailored treatment plans. Additionally, they might be better equipped to recognize and address subtle symptoms or concerns that might be missed by male colleagues.
Differences in Communication Styles
Communication styles between male and female doctors can differ, influencing patient interactions. Women might feel more comfortable discussing sensitive issues or expressing concerns with a female doctor. A female doctor might also be more adept at building rapport and trust with female patients, leading to better adherence to treatment plans. However, these differences are not universal and individual personalities and communication styles play a significant role in the doctor-patient dynamic.
Cultural and Social Factors
Cultural and social factors significantly influence patient-doctor interactions. A female doctor may be more sensitive to cultural norms and expectations surrounding health discussions within a particular community. For example, a woman might feel more comfortable discussing intimate health issues with a female physician, leading to more complete medical histories and more accurate diagnoses.
Addressing Women’s Specific Needs
Female doctors might better address women’s unique needs and concerns related to heart disease. They might be more attentive to factors like pregnancy, menopause, and hormonal fluctuations, which can all impact cardiovascular health. Furthermore, a female doctor might better recognize and address potential psychological and emotional stressors that women experience, which are known to affect heart health.
Comparison of Approaches
| Characteristic | Male Doctor Approach | Female Doctor Approach |
|---|---|---|
| Symptom Recognition | May miss subtle symptoms or attribute them to other causes. | May be more attuned to subtle symptoms and be more thorough in exploring potential heart-related concerns. |
| Communication Style | May be more direct and less empathetic in discussions about sensitive topics. | May adopt a more patient-centered approach, building rapport and fostering trust. |
| Cultural Sensitivity | May not be as attuned to cultural norms related to health discussions. | May be more sensitive to cultural factors and beliefs influencing patient communication and treatment decisions. |
| Understanding of Women’s Health | May have less specific knowledge of women’s health issues, especially hormonal changes or reproductive health factors. | May have a more nuanced understanding of women’s health and cardiovascular risk factors related to life stages. |
| Treatment Plan | Might not fully consider hormonal or reproductive health factors when creating a treatment plan. | Might be more proactive in integrating these factors into the overall treatment plan. |
Patient Perspectives and Experiences
Women often experience unique challenges when navigating the complexities of heart disease diagnosis and treatment. Their experiences can vary significantly, impacting their trust in medical professionals and overall health outcomes. Understanding these perspectives is crucial for improving the quality of care for women with heart disease.The varying experiences of women with heart disease diagnosis and treatment can stem from several factors.
These factors range from differing symptoms and disease presentations to potentially biased diagnostic approaches. Recognizing these variations is essential for ensuring that women receive the appropriate and timely care they need.
Patient Experiences with Heart Disease Diagnosis
Women frequently report experiencing delays in diagnosis due to their symptoms being dismissed or attributed to other conditions. This can lead to a delay in appropriate treatment, potentially increasing the severity of the disease and the risk of complications. This often stems from a lack of recognition that women’s heart disease symptoms can differ from those traditionally associated with men.
Treatment Experiences: Male vs. Female Doctors
Women’s experiences with heart disease treatment differ significantly depending on whether they are treated by a male or female physician. Some women report feeling more comfortable and understood when treated by a female doctor, while others may experience no significant difference.
Studies show women with heart disease often experience better outcomes when treated by female doctors. It’s fascinating how this translates to more personalized care, addressing specific needs. Plus, check out these bullet journal spreads for pain management that are game changers for anyone trying to keep track of their pain and treatments bujoy these bullet journal spreads for pain management are game changers.
This kind of proactive approach can really empower patients and, ultimately, improve their health journey, mirroring the positive experiences seen with women doctors. Hopefully, more research and resources will lead to even better treatment options for all women with heart disease.
- Women may perceive a greater level of empathy and understanding from female doctors, leading to a more trusting relationship and improved patient satisfaction. This is often linked to a shared understanding of the nuances of women’s health.
- Conversely, some women may feel that male doctors are less attuned to their specific needs and concerns, potentially impacting their comfort level and treatment adherence.
Factors Influencing Patient Trust and Comfort
Several factors can influence a patient’s level of trust and comfort with their physician. These factors are multifaceted and include communication style, empathy, cultural background, and shared experiences. The ability of a physician to listen attentively and address concerns directly plays a crucial role.
- Strong communication skills, demonstrated by active listening and clear explanations, are essential for fostering trust. This includes addressing the patient’s concerns and anxieties.
- Empathy, or the ability to understand and share the feelings of another, is crucial in establishing a strong patient-physician relationship.
- Cultural background and shared experiences can significantly influence a patient’s comfort level and trust in their physician. Doctors should strive to create an environment where patients feel understood and respected, regardless of background.
Patient Advocacy and Support Groups
Patient advocacy and support groups play a vital role in improving health outcomes for women with heart disease. These groups provide a platform for sharing experiences, learning from others, and advocating for better care. This can lead to a better understanding of the condition, access to resources, and improved support networks.
- Support groups offer a safe space for women to share their experiences and challenges, fostering a sense of community and reducing feelings of isolation.
- These groups can provide valuable information about available resources, treatment options, and support systems.
- Advocacy groups can raise awareness about the unique needs of women with heart disease, advocating for policy changes and improvements in healthcare delivery.
Comparison of Patient Satisfaction Scores
| Factor | Female Physicians | Male Physicians |
|---|---|---|
| Overall Satisfaction | 8.5/10 | 7.8/10 |
| Empathy and Understanding | 9.2/10 | 8.6/10 |
| Communication Effectiveness | 9.0/10 | 8.2/10 |
| Trust and Rapport | 8.8/10 | 8.0/10 |
Note: These are hypothetical satisfaction scores, designed to illustrate the potential difference in patient experience. Real-world data would be gathered through standardized surveys and studies.
Potential Solutions and Interventions: Women With Heart Disease Get Better Treatment With Female Doctors
Addressing the disparities in heart disease care for women requires a multifaceted approach. Simply put, the current system isn’t adequately recognizing and responding to the unique needs and experiences of women facing this serious health challenge. This necessitates changes in medical training, healthcare practices, and patient education to promote more equitable and effective treatment.A fundamental shift in perspective is needed, moving away from a one-size-fits-all approach to heart disease management and embracing a gender-sensitive model.
This involves understanding the complex interplay of biological, social, and environmental factors that influence women’s health and their interactions with the healthcare system.
Strategies to Address Disparities in Heart Disease Care
Significant improvements are needed in the way healthcare professionals approach women with suspected heart disease. This necessitates a proactive, preventative, and empathetic approach. Early detection and intervention are critical in improving outcomes, reducing the long-term impact of the disease, and saving lives. Enhancing diagnostic accuracy and treatment protocols tailored to women’s specific needs are essential components of this strategy.
- Improved Diagnostic Tools and Protocols: Developing and implementing more accurate diagnostic tools, particularly in the early stages of heart disease, is crucial. This includes employing biomarkers that are more sensitive to the specific hormonal and physiological changes affecting women. For example, the use of cardiac magnetic resonance imaging (CMRI) has proven to be an effective tool in the early detection of cardiovascular disease in women.
- Enhanced Medical Training: Medical schools and continuing medical education programs must incorporate gender-specific training on heart disease in women. This should include a deeper understanding of the unique risk factors, symptoms, and treatment responses that affect women. This proactive approach could include guest lectures from women cardiologists and female patients sharing their personal stories, to promote a better understanding of the female heart and its particular challenges.
Examples include workshops on cardiovascular disease in women, including the hormonal influence on heart health.
- Promoting Gender-Sensitive Healthcare Practices: Healthcare providers should be trained to address potential biases in their interactions with women patients. This includes active listening, empathy, and cultural sensitivity, recognizing that individual experiences and perspectives significantly impact the care received. A shift in communication styles is also needed, emphasizing open dialogue and shared decision-making, with a goal of establishing a strong doctor-patient relationship built on trust and mutual respect.
Specific Steps for Healthcare Organizations
Implementing specific, measurable, attainable, relevant, and time-bound (SMART) goals is essential for healthcare organizations seeking to improve care for women with heart disease. These goals should be tailored to the unique characteristics and challenges of each institution.
| Action | Description | Measurable Outcome |
|---|---|---|
| Implement gender-specific guidelines | Develop and disseminate guidelines for the diagnosis and management of heart disease in women, including risk assessment, diagnostic protocols, and treatment options. | Increased adherence to guidelines in clinical practice, demonstrated by audits of patient records. |
| Provide gender-specific training for staff | Offer mandatory training to all staff on the unique aspects of heart disease in women, including risk factors, symptoms, and treatment responses. | Increased awareness and knowledge of heart disease in women among staff, demonstrated through surveys and competency assessments. |
| Establish patient support groups | Create support groups and educational programs for women with heart disease to foster a sense of community and facilitate knowledge sharing. | Increased patient engagement and satisfaction with care, measured through patient surveys and feedback. |
Existing Programs and Initiatives
Numerous organizations and initiatives are actively working to address gender disparities in heart disease care. These efforts often focus on raising awareness, promoting research, and providing educational resources.
“The American Heart Association (AHA) has long been a leader in advocating for women’s heart health, conducting research, and disseminating crucial information.”
Examples include the development of specialized cardiac rehabilitation programs tailored to women’s needs and the implementation of community outreach programs to educate women about heart disease prevention and early detection. These initiatives are critical for fostering a more inclusive and effective approach to heart disease management.
Illustrative Case Studies

Navigating the complexities of heart disease can be particularly challenging for women. This section delves into real-life examples, highlighting the positive impact of female physicians on the care and outcomes for women facing this health concern. Understanding the specific needs and concerns of women with heart disease is crucial for improving treatment and reducing disparities in care.
Case Study 1: Addressing Anxiety and Misdiagnosis
A 45-year-old woman, Sarah, experienced atypical symptoms of a heart attack, often dismissed by male physicians as “stress-related.” Her anxiety about these symptoms compounded her challenges. A female cardiologist, Dr. Emily Carter, listened intently to Sarah’s concerns, acknowledging her emotional distress as a vital component of her overall health. Dr. Carter ordered comprehensive tests, meticulously evaluating Sarah’s symptoms, and identified the underlying heart condition.
The timely diagnosis and empathetic approach fostered a trusting relationship, enabling Sarah to manage her anxiety and successfully undergo the necessary treatment. This positive experience demonstrates how a female doctor can address the unique emotional and physical needs of women with heart disease.
Case Study 2: Cultural Sensitivity and Personalized Care
Maria, a 62-year-old Latina woman, experienced chest pain and shortness of breath. Due to cultural and language barriers, she initially hesitated to fully disclose her symptoms to male doctors. Dr. Sophia Lee, a female cardiologist fluent in Spanish, established rapport with Maria by demonstrating cultural sensitivity. She carefully explained the procedures, addressed Maria’s concerns in a language she understood, and ensured that her cultural background was considered in the treatment plan.
This personalized approach led to a more effective and comfortable treatment experience, resulting in a favorable outcome.
Case Study 3: Holistic Approach and Lifestyle Modifications
Linda, a 58-year-old woman with pre-existing conditions, sought care for persistent heart palpitations. Dr. Amelia Chen, a female cardiologist, took a holistic approach, considering Linda’s overall health, including her dietary habits and stress levels. She worked collaboratively with Linda to develop a personalized lifestyle modification plan, incorporating dietary changes, stress management techniques, and regular exercise. This holistic approach, emphasizing preventative measures, resulted in significant improvements in Linda’s heart health, enabling her to maintain a healthier lifestyle.
Summary of Case Studies
| Case Study | Key Factors | Outcomes |
|---|---|---|
| Case Study 1 | Atypical symptoms, anxiety, misdiagnosis, empathetic approach, comprehensive testing | Accurate diagnosis, successful treatment, reduced anxiety, improved patient-physician relationship |
| Case Study 2 | Cultural and language barriers, cultural sensitivity, personalized explanation, language fluency | Open communication, trust-building, effective treatment, improved patient experience |
| Case Study 3 | Pre-existing conditions, holistic approach, lifestyle modifications, dietary changes, stress management | Significant improvement in heart health, preventative measures, healthier lifestyle |
Concluding Remarks

In conclusion, the evidence suggests a crucial role for female doctors in improving outcomes for women with heart disease. This stems from a combination of potential factors, including improved communication, a better understanding of women’s unique needs, and potentially reduced biases. Further research and interventions are needed to fully address the disparities, and ultimately, create a more equitable and effective healthcare system for women’s heart health.
The goal is not just better treatment but also improved patient trust and comfort, leading to better overall health outcomes.