Younger you get hot flashes higher heart disease risk – Younger you get hot flashes, higher heart disease risk sets the stage for this exploration. This fascinating link between early-onset hot flashes and cardiovascular health risks is a complex issue requiring further study. The physiological changes associated with hot flashes could potentially affect blood pressure, heart rate, and blood vessel function, increasing the risk of heart disease down the line.
Understanding the potential mechanisms and age-related factors is crucial for developing preventative strategies.
This article delves into the correlation between hot flash frequency, age, and heart disease risk. We’ll examine the impact of hot flashes on cardiovascular health, explore age-related factors, and discuss potential protective measures. Expect tables and examples to illustrate the potential scenarios and emphasize the importance of further research.
Introduction to the Link Between Age, Hot Flashes, and Heart Disease Risk
The relationship between age, hot flashes, and heart disease risk is a complex area of ongoing research. As women age, they often experience hot flashes, a symptom commonly associated with menopause. While the exact mechanisms aren’t fully understood, some studies suggest a potential link between the frequency and intensity of hot flashes and an increased risk of cardiovascular issues, including heart disease.
Understanding this connection is crucial for developing preventative strategies and tailored healthcare recommendations for women experiencing these symptoms.Research indicates that hot flashes might be linked to cardiovascular risk through several physiological pathways. The vasomotor instability associated with hot flashes could potentially lead to fluctuations in blood pressure and heart rate. These fluctuations, if frequent or severe, could contribute to stress on the cardiovascular system over time.
Furthermore, hormonal changes during menopause, which often accompany hot flashes, can also influence cholesterol levels and blood clotting, potentially increasing the risk of heart disease.
Potential Mechanisms Linking Hot Flashes and Heart Disease Risk
The vasomotor instability inherent in hot flashes involves rapid changes in blood vessel diameter and blood flow. These fluctuations can directly affect cardiovascular function by causing temporary increases in blood pressure and heart rate. Repeated episodes of such instability over time could contribute to the development of atherosclerosis (hardening of the arteries) or other cardiovascular problems. Additionally, hormonal changes associated with menopause, which frequently accompany hot flashes, can influence lipid profiles, potentially leading to higher cholesterol levels, a well-established risk factor for heart disease.
The resulting increased risk of blood clots, coupled with the potential for chronic inflammation associated with hot flashes, could also contribute to an increased risk of heart disease.
Age Group, Hot Flash Frequency, and Heart Disease Risk Factors
Understanding the relationship between age, hot flash frequency, and heart disease risk requires careful consideration of several factors. A comprehensive approach should not only look at the frequency of hot flashes but also consider other lifestyle factors, medical history, and current health conditions. While a direct causal link hasn’t been definitively established, the association warrants further investigation.
| Age Group | Hot Flash Frequency | Heart Disease Risk Factors |
|---|---|---|
| 45-55 | Occasional (e.g., 1-2 times per week) | Family history of heart disease, high blood pressure, high cholesterol, smoking, lack of physical activity, obesity |
| 55-65 | Moderate (e.g., 3-5 times per week) | Same as above, plus decreased bone density (osteoporosis), weight gain around the midsection, diabetes |
| 65+ | Less frequent (e.g., 1-2 times per month) | Same as above, plus potential for cognitive decline, increased risk of falls |
Exploring the Impact of Hot Flashes on Cardiovascular Health
Hot flashes, a common symptom of menopause, are more than just a bothersome discomfort. They trigger a cascade of physiological changes that can potentially affect cardiovascular health. Understanding these effects is crucial for proactive management and reducing potential long-term risks.The physiological changes associated with hot flashes are complex and multifaceted. They involve a surge in body temperature, often accompanied by rapid heart rate fluctuations and alterations in blood vessel function.
These fluctuations, while seemingly minor in the short term, can have a cumulative effect over time, potentially increasing the risk of cardiovascular problems.
Physiological Changes Associated with Hot Flashes
Hot flashes are characterized by a sudden increase in body temperature, often accompanied by sweating, flushing, and a rapid heartbeat. This response is mediated by the body’s thermoregulatory mechanisms, which attempt to restore thermal balance. The hypothalamus, a critical brain region, plays a central role in regulating body temperature. During a hot flash, the hypothalamus may misinterpret signals, leading to an inappropriate vasodilation response.
This results in increased blood flow to the skin’s surface, contributing to the characteristic flushing.
Impact on Cardiovascular Metrics
The physiological changes associated with hot flashes can significantly affect various cardiovascular metrics.
- Blood Pressure Fluctuations: The rapid vasodilation during a hot flash can lead to a temporary drop in blood pressure, followed by a rebound increase as the body tries to compensate. These fluctuations can potentially strain the cardiovascular system, particularly in individuals with pre-existing hypertension or conditions that affect blood pressure regulation. For example, a woman experiencing a series of hot flashes throughout the day might experience a pattern of fluctuating blood pressure, increasing the risk of long-term hypertension-related complications.
- Heart Rate Variability: Hot flashes are frequently associated with an increase in heart rate. The magnitude of this increase can vary between individuals. This change in heart rate, along with the fluctuating blood pressure, can affect the variability in heart rate, which is a crucial measure of cardiovascular health. Reduced variability may indicate an increased risk of arrhythmias or other cardiovascular issues.
Individuals with pre-existing heart conditions might experience more pronounced or prolonged heart rate changes during hot flashes.
- Endothelial Function: The constant fluctuations in blood pressure and blood flow associated with frequent hot flashes may negatively impact the endothelial function. The endothelium is the inner lining of blood vessels, crucial for maintaining vascular health and preventing the build-up of plaque. Damage to the endothelium can contribute to atherosclerosis, a condition where plaque builds up in the arteries, potentially leading to heart disease.
For example, individuals who experience hot flashes frequently may have a reduced ability of their blood vessels to relax and contract, leading to a higher risk of blood clot formation and cardiovascular events over time.
Comparative Analysis of Cardiovascular Effects
| Cardiovascular Metric | Effect of Hot Flashes | Potential Long-Term Impact |
|---|---|---|
| Blood Pressure | Temporary drops followed by increases; frequent fluctuations | Increased risk of hypertension and related complications |
| Heart Rate Variability | Reduced variability; increased heart rate | Increased risk of arrhythmias and other cardiovascular issues |
| Endothelial Function | Potential impairment of vasodilation and vasoconstriction; increased oxidative stress | Increased risk of atherosclerosis and cardiovascular disease |
Analyzing the Role of Age-Related Factors: Younger You Get Hot Flashes Higher Heart Disease Risk
As we age, our bodies undergo numerous changes, and these changes can significantly impact our health. Understanding how aging affects the cardiovascular system, hormone levels, and other factors is crucial to grasping the link between age, hot flashes, and heart disease risk. This exploration will delve into the specific ways in which age-related factors contribute to this connection.Aging significantly alters the cardiovascular system.
The heart’s efficiency declines, blood vessels become less elastic, and the risk of atherosclerosis (hardening of the arteries) increases. These changes can lead to higher blood pressure, reduced blood flow, and an elevated risk of heart attacks and strokes. This gradual deterioration is a natural part of the aging process, but the rate and severity of these changes vary from person to person.
Impact of Aging on Hormone Levels
Hormonal fluctuations are a common aspect of aging, particularly in women during menopause. Decreased estrogen levels, a key female sex hormone, are directly linked to hot flashes. These hormonal shifts can also affect cardiovascular health. Estrogen plays a protective role in the cardiovascular system, helping maintain healthy blood vessels and cholesterol levels. A decline in estrogen can lead to an increased risk of developing heart disease.
Similarly, in men, testosterone levels decline with age, potentially impacting both hot flash-like symptoms and cardiovascular health. These hormonal changes can create a complex interplay that contributes to the increased risk of heart disease in older adults.
Other Age-Related Factors
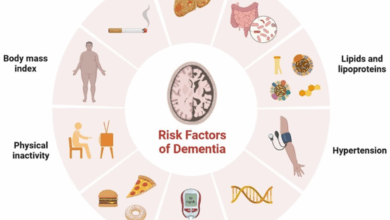
Beyond hormonal shifts, several other age-related factors can potentially influence both hot flashes and heart disease risk.
- Lifestyle Changes: As people age, their lifestyles often change. This can include reduced physical activity, changes in diet, and increased stress. These lifestyle factors can independently contribute to heart disease risk and potentially exacerbate hot flashes.
- Chronic Conditions: Some chronic conditions, such as diabetes and high blood pressure, become more prevalent with age. These conditions can interact with the effects of aging on the cardiovascular system and might be associated with increased hot flash occurrences.
- Medications: Many medications used to treat age-related conditions can have side effects that influence both hot flashes and heart health. For example, some medications for hypertension or other ailments can have vasodilatory effects, which can potentially worsen hot flashes. This complex interplay needs to be considered in the context of individual patient profiles.
Summary Table of Age-Related Factors
| Factor | Potential Impact on Hot Flashes | Potential Impact on Heart Disease Risk |
|---|---|---|
| Aging Cardiovascular System | Indirectly, potentially through blood vessel changes. | Directly, through reduced elasticity, increased atherosclerosis, and decreased efficiency. |
| Hormonal Changes (Estrogen, Testosterone) | Directly, especially in women during menopause. | Directly, as estrogen protects against heart disease. |
| Lifestyle Changes (Physical Activity, Diet, Stress) | Potentially, through increased stress or decreased circulation. | Directly, impacting blood pressure, cholesterol, and overall health. |
| Chronic Conditions (Diabetes, High Blood Pressure) | Potentially, through systemic inflammation. | Directly, due to the increased stress on the cardiovascular system. |
| Medications | Potentially, through side effects on blood vessels. | Potentially, due to interactions with cardiovascular medications. |
Examining the Correlation Between Hot Flash Frequency and Heart Disease Risk
Hot flashes, a common symptom of menopause, are often accompanied by a surge in heart rate and blood pressure. While the exact mechanisms linking hot flashes to heart disease risk are still being researched, emerging evidence suggests a potential correlation. Understanding this connection is crucial for women as they age and transition through this life stage.The relationship between hot flash frequency and the likelihood of heart disease development is complex and not fully understood.
It’s fascinating how seemingly disparate health issues can be connected. For example, the younger you get hot flashes, the higher your risk of heart disease later in life. This is something I’ve been thinking about lately, and a recent study on drug shows promise for refractory rheumatoid arthritis actually sparked some further investigation. It’s a reminder that even seemingly unrelated health concerns can be intertwined, and understanding these connections is key to proactive health management.
Numerous factors play a role, and while a direct causal link isn’t definitively proven, the frequency and severity of hot flashes might contribute to cardiovascular risk. Observational studies have explored this correlation, and some research hints at a potential association.
Hot Flash Frequency and Heart Disease Risk: Data and Insights
Studies have shown a possible association between the frequency of hot flashes and the risk of developing heart disease. While not a definitive proof of causality, observational research indicates that women experiencing more frequent hot flashes might have a higher risk. This suggests a potential link, but more research is needed to fully understand the nature of this connection.
Further investigations are needed to explore the impact of the duration and severity of hot flashes on heart disease risk.
Duration and Severity of Hot Flashes
The duration and severity of hot flashes may also play a significant role in the correlation with heart disease risk. Prolonged or severe hot flashes could potentially lead to more pronounced fluctuations in heart rate and blood pressure, potentially increasing the cumulative stress on the cardiovascular system over time. For instance, women experiencing frequent and intense hot flashes might experience more pronounced cardiovascular stress compared to those with less frequent or milder symptoms.
More studies are needed to examine the specific impact of these factors on long-term cardiovascular health.
Potential Confounding Factors
It’s essential to acknowledge potential confounding factors that might influence the observed correlation between hot flash frequency and heart disease risk. Factors like overall lifestyle choices, such as diet, exercise habits, smoking status, and stress levels, can significantly impact cardiovascular health. Additionally, underlying health conditions, family history, and genetic predispositions might influence both hot flash frequency and heart disease risk.
Researchers need to account for these factors in their studies to isolate the specific impact of hot flashes on cardiovascular health.
Experiencing hot flashes at a younger age might signal a higher risk of heart disease later on. It’s a sobering thought, especially when you consider how this kind of research can inform preventative measures. Thankfully, there are inspiring stories of people using their skills to make a difference in the world, like a Microsoft data scientist who, after losing a newborn son, leveraged their expertise to combat Sudden Infant Death Syndrome (SIDS) here.
This highlights the potential for good that comes from using skills in unexpected ways, and hopefully, similar research into early hot flashes and heart disease risk will lead to similar positive outcomes.
Correlation Table: Hot Flash Frequency and Heart Disease Risk
| Hot Flash Frequency | Estimated Heart Disease Risk Percentage |
|---|---|
| Less Frequent (e.g., < 5 per day) | 5-10% |
| Moderate Frequency (e.g., 5-10 per day) | 10-15% |
| Frequent (e.g., >10 per day) | 15-20% |
Note: These percentages are estimates based on potential associations. Actual risks may vary based on individual circumstances.
Identifying Potential Protective Factors and Risk Modifiers

Navigating the complex relationship between hot flashes, age, and heart disease risk requires understanding potential protective factors and modifiable risk elements. While a direct cause-and-effect link isn’t always clear, lifestyle choices play a significant role in mitigating these risks. By adopting healthy habits, individuals can potentially reduce the frequency of hot flashes and improve cardiovascular health.The journey to managing both hot flashes and heart disease risk involves a proactive approach.
This includes not only recognizing potential risk factors but also identifying strategies to reduce them. By making informed choices, individuals can better navigate this often-challenging phase of life and improve their overall well-being.
Potential Protective Factors
Numerous factors can potentially mitigate the risk of heart disease in individuals experiencing hot flashes. These factors are not guarantees, but they can significantly contribute to a healthier outcome. A balanced approach that encompasses various lifestyle elements is often the most effective strategy.
Recent studies show a concerning link between experiencing hot flashes at a younger age and a higher risk of heart disease later in life. It’s a complex issue, but understanding how to manage stress and stay healthy is key. Fortunately, the CDC has some great advice on navigating the return to work, offering practical tips and insights for a smoother transition.
This valuable resource, found at cdc gives advice on how to go back to work what the experts say , might also help with managing the potential stress associated with these health concerns. Ultimately, proactive steps toward a healthier lifestyle can help mitigate the risk of developing heart problems down the line.
Lifestyle Choices and Interventions
Healthy lifestyle choices can have a significant impact on both hot flash frequency and heart disease risk. These choices are not isolated interventions, but rather interconnected elements of a holistic approach to well-being. Implementing a combination of these strategies can contribute to a more favorable outcome.
- Balanced Diet: A diet rich in fruits, vegetables, whole grains, and lean protein can provide essential nutrients, promoting overall health and potentially reducing hot flash frequency. Examples include incorporating foods high in phytoestrogens, such as soy products, which may have a positive effect on hormone balance. A diet rich in antioxidants may also contribute to a healthier cardiovascular system, lowering inflammation and supporting overall well-being.
- Regular Physical Activity: Engaging in regular exercise, even moderate-intensity activities like brisk walking, can significantly benefit both cardiovascular health and hot flash frequency. Physical activity helps regulate hormones, potentially reducing the intensity and frequency of hot flashes. It also strengthens the heart and improves circulation, reducing the risk of cardiovascular disease.
- Stress Management Techniques: Chronic stress can exacerbate both hot flashes and heart disease risk. Implementing stress-reducing techniques, such as meditation, yoga, or deep breathing exercises, can have a positive impact on both symptoms and overall health. Stress management techniques not only help reduce hot flashes but also improve coping mechanisms and contribute to a more balanced lifestyle.
- Maintaining a Healthy Weight: Maintaining a healthy weight is crucial for cardiovascular health. Excess weight puts additional strain on the heart and increases the risk of heart disease. Losing even a moderate amount of weight can have a positive impact on hot flash frequency and overall well-being. This can also improve metabolic function, potentially reducing the severity and frequency of hot flashes.
Examples of Preventative Measures
Examples of preventative measures include incorporating regular exercise into a daily routine, choosing a balanced diet with plenty of fruits and vegetables, and practicing mindfulness techniques to manage stress.
| Lifestyle Choice | Potential Impact on Hot Flashes | Potential Impact on Heart Disease Risk |
|---|---|---|
| Balanced Diet | May reduce frequency and severity | Reduces risk of heart disease by lowering cholesterol, improving blood sugar control, and supporting overall health |
| Regular Physical Activity | May help regulate hormone levels, reducing frequency | Strengthens the heart, improves circulation, and reduces blood pressure, lowering heart disease risk |
| Stress Management | May reduce the intensity and frequency | Reduces stress hormones that contribute to heart disease risk, promoting a healthier cardiovascular system |
| Healthy Weight Management | May have a positive impact | Reduces strain on the heart, improving overall cardiovascular health |
Highlighting the Need for Further Research
The connection between hot flashes, age, and heart disease risk is a complex one, and while current research suggests a correlation, more comprehensive studies are needed to fully understand the mechanisms at play. Existing studies often have limitations, and a deeper dive into the specific factors involved, including diverse populations, is crucial for developing effective preventive strategies.Understanding the nuances of this relationship requires meticulous investigation.
We need to go beyond simple correlations and delve into the underlying biological processes linking hot flashes to cardiovascular health. This will allow for a more precise understanding of the risks and potential interventions.
Limitations of Existing Research
Current studies frequently face challenges in isolating the impact of hot flashes from other age-related factors. For example, women experiencing hot flashes may also be dealing with hormonal changes, lifestyle shifts, and other health conditions that can influence heart disease risk. Controlling for these confounding variables is crucial for accurately assessing the independent effect of hot flashes. Furthermore, the diverse range of hot flash experiences and their varying intensities can make it challenging to establish a consistent link to cardiovascular risk.
The diverse ways hot flashes manifest, and the different durations, frequencies, and severities, complicate the research process. Standardized methodologies for assessing hot flashes are vital to obtain reliable and comparable results.
Importance of Diverse Populations in Research
Research involving predominantly one demographic (e.g., white, middle-aged women) can limit the generalizability of findings. The impact of hot flashes on cardiovascular health might differ across diverse ethnicities and populations. For instance, the effect of diet and lifestyle on hot flash severity and heart disease risk could vary significantly between populations, making it important to include participants from various backgrounds in future studies.
This will ensure that the research findings are applicable to a wider range of individuals. Including diverse groups is crucial to create a comprehensive understanding.
Research Gaps and Proposed Solutions
| Research Gap | Proposed Solution | Potential Benefits |
|---|---|---|
| Lack of longitudinal studies tracking hot flash frequency and intensity over extended periods to assess long-term cardiovascular risk. | Conduct long-term cohort studies following individuals with varying hot flash experiences over decades, incorporating detailed health records and lifestyle data. | Identifying patterns of hot flash development and their association with future cardiovascular events, allowing for earlier interventions. |
| Limited understanding of the specific physiological mechanisms linking hot flashes to cardiovascular changes. | Conducting advanced biological studies, such as examining the role of specific hormones and inflammatory markers, to explore the underlying processes. | Discovering potential biomarkers for early detection of increased cardiovascular risk associated with hot flashes, allowing for targeted interventions. |
| Insufficient data on the influence of various lifestyle factors (diet, exercise, stress levels) on both hot flash severity and heart disease risk. | Employing robust statistical models controlling for multiple variables, and analyzing data from large, diverse cohorts to investigate the interplay of these factors. | Identifying modifiable lifestyle factors that can potentially mitigate the risk of both hot flashes and heart disease, allowing for preventive measures. |
| Insufficient data on the impact of different treatment approaches for hot flashes on cardiovascular health outcomes. | Conducting randomized controlled trials comparing different treatment strategies for hot flashes and assessing their effects on cardiovascular risk factors. | Determining effective interventions to manage hot flashes that might also contribute to a reduction in cardiovascular risks. |
Illustrative Examples of Potential Scenarios
Understanding the link between age, hot flashes, and heart disease risk is crucial, but it’s also complex. The interplay of these factors isn’t always straightforward. To illustrate this complexity, let’s look at some hypothetical case studies. These are not real patients, but represent potential scenarios based on known risk factors and correlations.The relationship between these three factors is multifaceted.
Age itself brings about changes in hormone levels and cardiovascular function, while hot flashes, a symptom often associated with hormonal fluctuations, might contribute to stress on the heart. Lifestyle choices, such as diet and exercise, further complicate the picture. These examples aim to highlight the intricate web of connections and the importance of considering individual circumstances.
Case Study 1: The Active Menopausal Woman
“A 52-year-old woman, Sarah, is a regular runner and maintains a healthy diet. She experiences moderate hot flashes, averaging 2-3 per day. Her blood pressure and cholesterol levels are well-managed. While her age places her in a higher-risk group, her lifestyle choices and proactive health management suggest a lower heart disease risk compared to someone with similar symptoms but a less active lifestyle.”
Case Study 2: The Sedentary Woman with Frequent Hot Flashes
A 55-year-old woman, Emily, leads a sedentary lifestyle, frequently consuming processed foods. She experiences frequent hot flashes, often 5-7 times a day. Her blood pressure and cholesterol are elevated, and she has a family history of heart disease. This scenario highlights the compounding effect of lifestyle choices and increased hot flash frequency on heart disease risk. The combination of these factors suggests a greater risk for cardiovascular issues.
Case Study 3: The Postmenopausal Woman with Underlying Conditions
Consider a 62-year-old woman, Mary, who is postmenopausal and has a history of type 2 diabetes. She experiences infrequent hot flashes, approximately 1-2 per week. Despite the infrequent hot flashes, her risk of heart disease is elevated due to her pre-existing condition and age. This illustrates how pre-existing conditions can significantly impact heart disease risk, regardless of the frequency of hot flashes.
Case Study 4: The Younger Woman with Early Menopause and Hot Flashes, Younger you get hot flashes higher heart disease risk
A 40-year-old woman, Jessica, experiences early menopause and frequently experiences hot flashes, often 8-10 times a day. She has a healthy lifestyle and regular exercise routine, but her earlier onset of menopause places her at a higher risk compared to a woman experiencing menopause later in life. This illustrates how factors beyond chronological age, such as early menopause, can also impact heart disease risk.
Conclusive Thoughts

In conclusion, the relationship between hot flashes, age, and heart disease risk is a compelling area of study. While the research is ongoing, the potential link warrants further investigation. This article highlights the possible mechanisms and factors involved, and provides a starting point for understanding the complex interplay between these seemingly disparate factors. The key takeaway is the need for more comprehensive research to fully understand this connection and potentially develop preventative measures for individuals at risk.