New IBS guidelines call for personalized treatments what to know. The shift towards personalized medicine is revolutionizing healthcare, and now, it’s impacting how Irritable Bowel Syndrome (IBS) is diagnosed and treated. This approach moves beyond one-size-fits-all solutions, recognizing the unique factors influencing each individual’s experience with IBS. This means a more tailored and effective treatment plan, potentially leading to better outcomes and improved quality of life for those affected.
The new guidelines represent a significant departure from traditional approaches, incorporating the latest research and a deeper understanding of the complex interplay of factors that contribute to IBS. This personalized approach considers not just the symptoms, but also patient history, lifestyle, and even genetic predispositions. The result is a more proactive and patient-centered strategy that empowers individuals to take control of their health.
Introduction to IBS and Personalized Treatments
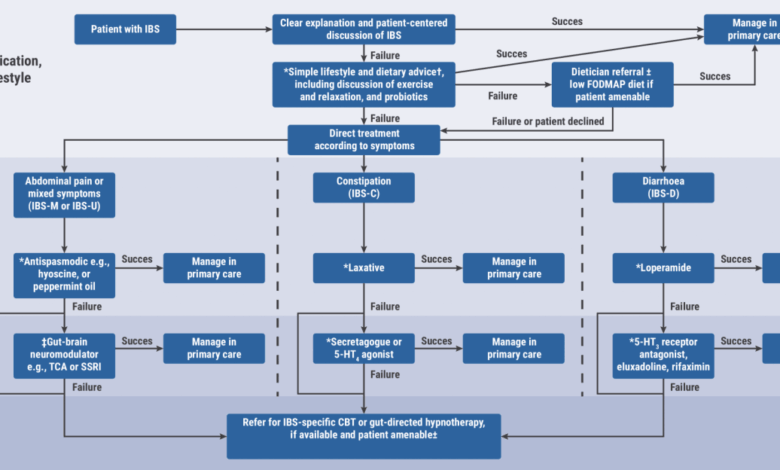
Irritable bowel syndrome (IBS) is a common chronic condition affecting the digestive system. Characterized by abdominal pain, changes in bowel habits (constipation, diarrhea, or both), and often gas and bloating, IBS significantly impacts quality of life for millions worldwide. While the exact cause remains elusive, various factors including diet, stress, and gut microbiota are believed to play a role.Historically, IBS treatments have been largely symptom-based, relying on general dietary recommendations, stress management techniques, and over-the-counter medications like antispasmodics and laxatives.
This approach, while helpful for some, often failed to address the unique needs of individual patients. This approach has proven to be insufficient for many, as the underlying causes and responses vary significantly from person to person.
The Shift Towards Personalized Medicine
The healthcare landscape is undergoing a significant shift towards personalized medicine. This approach recognizes that each individual responds differently to treatments and that tailored strategies can improve outcomes. This concept extends beyond IBS and is revolutionizing many areas of medical care. The shift is driven by advancements in genetics, genomics, and diagnostics.
Historical Approaches to Treating IBS
Early treatments for IBS were often focused on symptom management. Dietary restrictions, stress reduction techniques, and over-the-counter medications like antispasmodics were common approaches. While these methods offered some relief for some individuals, they often lacked the precision necessary to address the specific needs of each patient.
The Evolution of IBS Guidelines
The new IBS guidelines represent a departure from previous approaches. These updated guidelines emphasize a personalized treatment strategy, tailoring recommendations to individual patient needs. This approach acknowledges the variability in IBS presentations and responses to treatments. This difference is crucial, as it recognizes the diverse and complex nature of the condition. The key difference lies in the focus on understanding individual patient factors.
Key Factors Driving the Change
Several factors have driven the shift towards personalized IBS treatment strategies. Advanced diagnostic tools allow for a more thorough understanding of individual gut microbiota profiles, genetic predispositions, and other factors that influence disease progression. Increased awareness of the complex interplay between genetics, diet, and the gut microbiome has also played a significant role. Furthermore, the growing body of research exploring these factors has fueled this shift towards a more targeted approach.
Research has shown that certain genetic markers can indicate an individual’s likelihood of responding to particular treatments, providing crucial insights for personalized treatment plans.
Example of Personalized Approaches
Consider a patient with IBS-D (diarrhea-predominant IBS). Traditional approaches might focus on reducing dietary triggers and increasing fiber intake. However, a personalized approach might involve a comprehensive assessment including stool analysis, genetic testing, and potentially even personalized dietary recommendations based on their gut microbiome. This strategy aims to identify specific triggers and tailor a treatment plan to address those triggers directly, maximizing efficacy and minimizing side effects.
Understanding the New Guidelines
The new IBS guidelines represent a significant shift from previous approaches, emphasizing a more personalized and patient-centered approach to diagnosis and treatment. These updated recommendations move beyond a one-size-fits-all approach, acknowledging the diverse range of symptoms and experiences associated with Irritable Bowel Syndrome. This personalized strategy aims to tailor management plans to the individual needs of each patient, leading to more effective and satisfying outcomes.The core principles of these new guidelines are built upon a foundation of shared decision-making between patients and healthcare providers.
This collaborative approach allows for a more thorough understanding of individual symptoms, lifestyle factors, and personal preferences. It also highlights the importance of addressing the psychological and emotional impact of IBS, recognizing that these factors can significantly influence symptom severity and management.
Diagnostic Criteria in the New Guidelines
The new guidelines have broadened the diagnostic criteria for IBS, moving beyond solely relying on symptom duration and frequency. These updated criteria incorporate a more comprehensive evaluation of patient history, physical examination findings, and potential contributing factors. This holistic approach aims to improve accuracy and reduce misdiagnosis, recognizing that IBS symptoms can overlap with other conditions.
Types of IBS
The new guidelines recognize the diverse presentations of IBS, encompassing various subtypes, each with its own characteristic symptom profile. These include Irritable Bowel Syndrome with Diarrhea (IBS-D), Irritable Bowel Syndrome with Constipation (IBS-C), and Irritable Bowel Syndrome with Mixed Symptoms (IBS-M). Understanding these distinct subtypes is crucial for developing tailored management strategies.
Comparison of Old and New Guidelines for IBS-D
The old guidelines often focused primarily on symptom frequency and duration to diagnose IBS-D. The new guidelines, however, emphasize the need for a more nuanced assessment, considering the patient’s overall health, lifestyle factors, and psychosocial well-being. They also consider the presence of other conditions that may mimic IBS-D. For instance, a patient experiencing frequent diarrhea might also have underlying celiac disease or inflammatory bowel disease.
Comparison of Old and New Guidelines for IBS-C
Historically, IBS-C diagnosis was often reliant on the presence of constipation as the primary symptom. The updated guidelines encourage a more comprehensive evaluation, encompassing a broader range of symptoms beyond just constipation, such as bloating and abdominal pain. They also emphasize the importance of evaluating for potential underlying medical conditions that can contribute to constipation, such as hypothyroidism or medication side effects.
Comparison of Old and New Guidelines for IBS-M
For IBS-M, the old guidelines often lacked specific diagnostic criteria. The new guidelines aim to clarify diagnostic approaches by emphasizing the heterogeneity of IBS-M. They encourage a thorough assessment of both diarrhea and constipation symptoms, along with abdominal pain and bloating. This more detailed evaluation assists in distinguishing IBS-M from other conditions with overlapping symptoms.
New Considerations for Patient Factors in Diagnosis
The new guidelines emphasize the crucial role of patient factors in the diagnostic process. They highlight the need to consider psychological factors, such as stress and anxiety, as potential contributors to IBS symptoms. Furthermore, these guidelines acknowledge the impact of lifestyle choices, including diet and exercise, on symptom management. A patient’s reported stress levels and dietary habits will now be incorporated into the diagnostic process, emphasizing a holistic approach.
Personalized Treatment Strategies
The new IBS guidelines emphasize a personalized approach to treatment, moving away from a one-size-fits-all strategy. This shift recognizes the diverse range of factors influencing IBS symptoms and responses to treatment. Understanding these individual factors allows healthcare professionals to tailor interventions for optimal outcomes. This personalized approach goes beyond simply adjusting medication dosages; it considers the patient’s unique needs and preferences.Personalized treatment plans are designed to address the specific needs of each individual with IBS.
So, the new IBS guidelines are all about personalized treatments, which is super exciting. It’s all about figuring out what works best for each individual. While we’re on the topic of innovative dietary approaches, did you know that edible insects are gaining popularity as a potential superfood? Check out why edible insects are the next superfood trend for a deeper dive.
Ultimately, this personalized approach to health, whether it’s through diet or medicine, is a fantastic step forward in understanding and treating conditions like IBS.
This approach considers a multitude of factors, from dietary sensitivities to psychological stressors, to create a comprehensive and effective treatment plan. By taking these factors into account, healthcare providers can work with patients to achieve better symptom management and improve their overall quality of life.
Patient Characteristics Influencing Treatment Decisions
Various patient characteristics significantly influence treatment decisions for IBS. These include a patient’s medical history, including any pre-existing conditions, allergies, or sensitivities. Also crucial are lifestyle factors such as dietary habits, exercise routines, and stress levels. Furthermore, psychological factors like anxiety and depression can play a substantial role in symptom severity and response to treatment. Understanding these factors is essential for developing a tailored approach that addresses the multifaceted nature of IBS.
Examples of Personalized Treatment Strategies
Personalized treatment strategies for IBS encompass a range of interventions. Dietary modifications, a cornerstone of personalized treatment, might involve identifying specific food triggers through detailed dietary diaries and elimination diets. This process allows for the identification of problematic foods and the development of a personalized dietary plan that minimizes symptom exacerbation. Medication choices also play a critical role.
The new guidelines often recommend targeted medications based on the specific type of IBS and the patient’s response to various medications. For instance, certain medications might be more effective in managing diarrhea-predominant IBS, while others might be better suited for constipation-predominant IBS. Furthermore, the selection of medication can be influenced by a patient’s specific medical history, including allergies or other health conditions.
This meticulous approach ensures that medications are both effective and safe.
Potential Benefits of a Personalized Approach
A personalized approach to IBS treatment offers several significant advantages. Improved symptom management is a primary benefit. By addressing the unique factors contributing to a patient’s IBS, the personalized approach can lead to more effective symptom relief. Increased patient satisfaction is another benefit. When patients feel heard and understood, they are more likely to adhere to their treatment plan and experience a greater sense of control over their condition.
Furthermore, a personalized approach can lead to a reduced risk of adverse events. Tailoring treatment to individual needs minimizes the potential for negative side effects associated with inappropriate medication choices.
Comparison of Old and New Treatment Options
| Old Treatment Option | New Personalized Treatment Option | Rationale for Change | Patient Considerations |
|---|---|---|---|
| Generic medication for IBS | Targeted medication based on IBS subtype (e.g., loperamide for diarrhea-predominant) | Targeted medications are often more effective and safer, minimizing side effects and maximizing efficacy | Patient’s specific medical history (allergies, other conditions), IBS subtype (diarrhea-predominant, constipation-predominant), and response to various medications |
| Generalized dietary advice | Personalized dietary plan based on identified food triggers and intolerances | Identifying specific triggers allows for tailored dietary modifications to minimize symptoms | Patient’s specific dietary preferences, food intolerances, and sensitivities |
| Limited psychological support | Integrated psychological support to address stress, anxiety, and depression | Recognizing the significant role of psychological factors in IBS symptom management | Patient’s mental health status, coping mechanisms, and willingness to engage in psychological support |
Impact on Patient Management
The new IBS guidelines, emphasizing personalized treatments, represent a significant shift in how we approach patient care. This shift requires a fundamental change in how patients are educated and supported, demanding a more active role for patients in their own healthcare journey. This new paradigm acknowledges the diversity of IBS experiences and the need for tailored interventions.The personalized approach necessitates a deeper understanding of the patient’s individual needs, preferences, and lifestyle factors.
This, in turn, demands improved communication channels and a more collaborative relationship between patients and healthcare providers. The guidelines aim to empower patients to take ownership of their health, ultimately leading to better outcomes.
Patient Education and Support
The new guidelines highlight the importance of comprehensive patient education. This goes beyond simply explaining the diagnosis and treatment options. It involves educating patients about the various factors influencing their IBS, such as stress management techniques, dietary considerations, and the role of gut microbiota. This empowers patients to actively participate in their treatment and make informed decisions.
Support groups and online resources can play a crucial role in providing a community for patients to share experiences and gain encouragement.
Role of Patient Communication
Effective communication is paramount in a personalized approach to IBS management. This involves open dialogue between patients and healthcare providers, fostering a trusting relationship where patients feel comfortable discussing their symptoms, preferences, and concerns. Patients need to feel heard and understood, enabling them to actively participate in creating a treatment plan tailored to their unique needs. This involves sharing personal experiences and preferences, while healthcare providers provide evidence-based information and guidance.
Challenges in Implementing the New Guidelines
Implementing these new guidelines presents certain challenges. One key challenge is ensuring that healthcare providers have the necessary training and resources to effectively implement personalized treatments. Another challenge is the potential for increased costs associated with specialized diagnostic tests and treatments. Finally, the complexities of personalizing treatments might require more time for consultations and potentially greater workload for healthcare providers.
So, the new IBS guidelines are all about personalized treatments, which is super exciting. It means figuring out what works best for you individually. While exploring different approaches, it’s important to consider potential connections to other conditions, like how marijuana might impact ulcerative colitis. For a deeper dive into that fascinating link, check out this article on marijuana and ulcerative colitis.
Ultimately, the goal is still to tailor the best treatment plan for your specific IBS needs.
Importance of Patient Involvement in Treatment Decisions
Patient involvement in treatment decisions is crucial. Patients possess unique insights into their symptoms, responses to different interventions, and personal preferences. This collaborative approach ensures that treatment plans are more effective and aligned with the patient’s specific needs. Active participation leads to greater patient satisfaction and adherence to the treatment plan, ultimately improving long-term outcomes.
Potential Patient Questions about Personalized Treatments
- How will my specific IBS subtype affect the treatment plan?
- What are the potential benefits and risks of different personalized treatment options?
- What role will my diet play in my personalized treatment?
- How can I best manage stress and its impact on my IBS symptoms?
- What are the different diagnostic tools used to personalize my treatment?
- What are the different types of medications and therapies that might be considered for my IBS?
- How can I find support groups or resources related to my specific type of IBS?
Dietary Considerations in Personalized Treatment
Dietary choices play a pivotal role in managing irritable bowel syndrome (IBS). The impact of specific foods on symptoms varies significantly between individuals, making a personalized dietary approach crucial for effective symptom control. This individualized strategy considers the specific needs and triggers for each patient.Understanding the complex interplay between diet and IBS symptoms is essential for creating a personalized management plan.
Different dietary patterns can significantly affect bowel function, leading to either symptom relief or exacerbation. Tailoring dietary strategies to individual needs allows patients to regain control over their digestive health and improve their overall well-being.
Importance of Diet in Managing IBS
Diet is a critical component of IBS management. Individual responses to various foods differ greatly, making it essential to identify triggers and personalize dietary approaches. By carefully monitoring food intake, patients can potentially minimize symptoms and enhance their quality of life. This individualized approach allows for a more effective management strategy, tailored to the specific needs of each person.
Different Dietary Approaches Tailored to Individual Needs
A range of dietary approaches can be effective in managing IBS. These include low FODMAP diets, elimination diets, and even incorporating specific prebiotics and probiotics. The effectiveness of each strategy varies based on the individual’s specific IBS subtype and symptom profile. This personalized approach allows for a more tailored and effective management strategy.
Examples of Specific Dietary Modifications for Various IBS Types
Different IBS subtypes respond differently to dietary modifications. For example, individuals with IBS with diarrhea (IBS-D) often find that reducing fermentable carbohydrates, such as those found in beans, onions, and apples, can help alleviate symptoms. Conversely, those with IBS with constipation (IBS-C) may find that increasing fiber intake and incorporating foods like fruits and vegetables can promote regularity.
This tailored approach is crucial for effectively managing IBS symptoms.
Sample Dietary Plans for Different IBS Types
| IBS Type | Dietary Focus | Example Foods to Include | Example Foods to Limit |
|---|---|---|---|
| IBS-D | Low FODMAP | Cooked rice, chicken breast, plain yogurt, lean meats, bananas (in moderation), well-cooked vegetables (e.g., carrots, zucchini) | Beans, onions, apples, garlic, wheat, most dairy products (unless lactose-free), mushrooms, some fruits |
| IBS-C | High Fiber | Fruits (e.g., berries, pears), vegetables (e.g., broccoli, spinach), whole grains (e.g., brown rice, quinoa), legumes (e.g., lentils, chickpeas), chia seeds | Processed foods, refined grains, high-fat foods, excessive dairy products, some fruits (e.g., plums, prunes) |
| IBS-M (Mixed) | Balanced, Low FODMAPs | Lean protein sources, whole grains, vegetables, fruits (in moderation), small portions of certain FODMAPs | High-fat foods, processed foods, highly-processed sugary drinks, foods high in FODMAPs |
This table provides a basic overview. A personalized approach is crucial, and consultation with a registered dietitian or healthcare professional is highly recommended for tailored dietary plans. This individualized approach ensures optimal management of symptoms and overall well-being.
Role of Technology and Data in Personalized Treatment
The new IBS guidelines emphasize personalized treatments, tailoring therapies to individual needs. Technology plays a crucial role in this approach, enabling better symptom monitoring and data analysis to optimize treatment plans. This allows for more effective management and improved patient outcomes.Technology empowers individuals with IBS to actively participate in their care, providing tools for self-management and enhancing communication with healthcare providers.
Data analysis facilitates the development of customized treatment strategies, leading to a more precise and effective approach to managing IBS symptoms.
Tracking and Monitoring IBS Symptoms
Data collection and analysis are essential components of personalized IBS treatment. Accurate symptom tracking allows healthcare professionals to identify patterns and triggers, leading to more effective interventions. Individuals with IBS can use various technologies to meticulously record their symptoms, including pain intensity, frequency of bowel movements, and the presence of any associated discomfort.
Data Analysis for Tailored Treatments
Data analysis helps healthcare providers gain insights into individual patient responses to different treatments. This data-driven approach allows for adjustments to treatment strategies as needed. Sophisticated algorithms can identify correlations between specific dietary factors, lifestyle choices, and symptom severity. This leads to a more individualized and responsive treatment plan. For instance, a patient might discover a correlation between caffeine consumption and increased abdominal pain, prompting a reduction in caffeine intake.
Wearable Devices for Symptom Monitoring
Wearable devices, such as smartwatches and fitness trackers, offer convenient and continuous symptom monitoring. These devices can track activity levels, sleep patterns, and even subtle physiological changes, providing a comprehensive picture of the patient’s overall health. For example, a patient might notice a correlation between increased stress and heightened IBS symptoms, prompting them to incorporate stress-reduction techniques into their daily routine.
So, the new IBS guidelines are all about personalized treatments, which is super exciting. It’s like finally recognizing that everyone’s body is different, and treatments need to be tailored accordingly. This reminds me of how fascinating research into using your body clock to treat cancer is exploring – using your body clock to treat cancer is a whole new frontier.
Ultimately, these personalized approaches, whether for IBS or other conditions, are promising a more effective and comfortable path toward better health.
This data can be shared with healthcare providers to further personalize the treatment plan.
Digital Tools Enhancing Patient Engagement
Digital tools and apps can significantly enhance patient engagement and adherence to treatment plans. Interactive platforms provide educational resources, support communities, and facilitate communication with healthcare professionals. This improved communication allows for a more proactive and collaborative approach to IBS management. For instance, online forums or support groups can connect patients with others experiencing similar symptoms, fostering a sense of community and shared understanding.
Data Collection and Analysis
Data collection for IBS treatment often involves a combination of self-reported information, wearable device data, and medical records. These data points are then analyzed using various methods, including statistical modeling and machine learning algorithms. This process aims to identify patterns and correlations, leading to personalized recommendations. For instance, a patient’s dietary logs, alongside their activity levels tracked by a smartwatch, could be analyzed to reveal patterns linking specific foods to symptom flare-ups.
This comprehensive data allows for a more precise understanding of individual responses to different treatments. The data is collected and analyzed with strict adherence to patient privacy regulations.
Addressing Potential Challenges and Concerns
The exciting prospect of personalized IBS treatments brings with it a set of potential challenges. While these treatments hold the promise of more effective and targeted therapies, careful consideration must be given to practical implementation, cost-effectiveness, and equitable access. Addressing these concerns is crucial to ensuring that this advancement in care benefits all those affected by IBS.Implementing personalized treatments requires a significant shift in the healthcare landscape.
Existing systems may not be fully equipped to handle the complexities of tailoring treatment plans to individual needs. This necessitates investment in infrastructure, training, and potentially, new diagnostic tools.
Potential Challenges in Implementation
The successful implementation of personalized treatments requires a robust healthcare system. Existing infrastructure may struggle to adapt to the individualized approach. This necessitates investments in updated diagnostic tools, training programs for healthcare providers to administer these new treatments, and potentially, new software or platforms for managing patient data. Furthermore, the need for specialized expertise in different areas of treatment (nutrition, behavioral therapy, etc.) might necessitate interdisciplinary collaboration.
Cost Implications of Personalized Treatments
Personalized treatments, while potentially highly effective, often come with a higher price tag compared to standard treatments. The need for specialized diagnostics, tailored medication regimens, and potentially ongoing monitoring can increase the overall cost of care. This raises concerns about affordability and access for patients with limited financial resources. Insurance coverage for these treatments may also pose a challenge, and further investigation into cost-sharing models and subsidies may be needed to make these treatments more accessible.
Potential Disparities in Access to Personalized Care
Access to personalized treatments may not be uniform across different demographics or geographic locations. Factors like socioeconomic status, geographic location, and existing healthcare disparities could exacerbate existing inequalities. This underscores the importance of proactive strategies to ensure equitable access, such as subsidies, community outreach programs, and the development of accessible telehealth platforms. Further research into the potential for personalized treatments to improve health outcomes for underserved populations is essential.
Addressing Data Privacy and Security Concerns
The use of patient data in personalized treatments raises important concerns regarding data privacy and security. Strict adherence to data protection regulations, robust security measures, and transparent communication about data usage are crucial. Patients must be empowered to understand how their data is being used and have control over its access. This includes clear policies regarding data storage, sharing, and potential breaches.
Transparent communication with patients about how their data will be used is critical.
Strategies for Promoting Equitable Access
Promoting equitable access to personalized treatments requires a multi-faceted approach. Developing affordable pricing models, offering financial assistance programs, and ensuring that these treatments are accessible through various healthcare settings, including community health centers and telehealth platforms, are vital. Investment in training healthcare providers and implementing clear guidelines for insurance coverage will also be essential to address potential barriers.
Illustrative Case Studies: New Ibs Guidelines Call For Personalized Treatments What To Know

The new IBS guidelines emphasize personalized treatment plans, moving away from a one-size-fits-all approach. Understanding how these guidelines translate into real-world scenarios is crucial for both patients and healthcare professionals. This section provides hypothetical case studies to illustrate the application of personalized treatment strategies.Personalized medicine in IBS involves tailoring treatment based on individual patient characteristics, symptoms, and responses to various interventions.
This approach promises to improve outcomes by addressing the root causes of IBS rather than just managing symptoms.
Case Study 1: Young Female with IBS-D, New ibs guidelines call for personalized treatments what to know
This case study focuses on a 25-year-old female presenting with frequent, watery bowel movements (IBS-D). Her symptoms were exacerbated by stress and certain foods, particularly dairy products and processed foods. Initial assessments included a detailed symptom diary, a food diary, and blood tests to rule out other potential medical conditions. A dietitian recommended a low-FODMAP diet, eliminating high-fermentable oligosaccharides, disaccharides, monosaccharides, and polyols.
This dietary intervention led to a significant reduction in bowel movements and improved overall quality of life. Further investigation into stress management techniques, such as mindfulness exercises, was also incorporated into her treatment plan.
Case Study 2: Older Male with IBS-C
A 65-year-old male patient presented with chronic constipation (IBS-C). His symptoms were linked to a sedentary lifestyle and a history of medication use. Initial assessments included a review of his medical history, a physical examination, and a stool test. While dietary modifications were explored, the patient’s primary issue was addressed by adding a daily dose of a stimulant laxative.
This was carefully monitored and adjusted based on the patient’s response, ensuring it did not cause any adverse effects. His treatment plan also included increasing physical activity and adjusting his current medication regimen.
Case Study 3: Patient with IBS and Anxiety
A 30-year-old patient presented with IBS symptoms that were significantly worsened by anxiety. This case emphasizes the importance of addressing the psychological factors associated with IBS. The patient was referred to a therapist for cognitive behavioral therapy (CBT) to help manage their anxiety. In conjunction with CBT, the patient was given a personalized dietary plan, focusing on stress-reducing foods and minimizing triggers.
The combination of CBT and dietary adjustments proved highly effective in managing both the anxiety and the IBS symptoms.
Comparison of Case Studies
| Case Study 1 | Case Study 2 | Similarities | Differences |
|---|---|---|---|
| Young female with IBS-D, symptoms exacerbated by food triggers. | Older male with IBS-C, symptoms linked to lifestyle and medication. | Both patients benefited from tailored treatment plans, considering individual factors. | Patient 1 focused on dietary changes (low-FODMAP diet), while Patient 2 used medication (laxatives) and lifestyle adjustments. Patient 3 addressed both physical and psychological factors. |
Final Wrap-Up
In conclusion, the new IBS guidelines represent a crucial advancement in patient care. By embracing personalized treatments, we can move beyond symptom management and toward more effective, sustainable solutions. The integration of technology, data analysis, and patient-centered care promises a brighter future for individuals living with IBS. However, challenges such as cost and equitable access must be addressed to ensure that these benefits are available to everyone who needs them.