Future of JAK inhibitors for treatment of RA is a rapidly evolving field, promising significant advancements in managing rheumatoid arthritis (RA). This exploration delves into the current state of JAK inhibitor therapies, analyzing their mechanisms, clinical trial results, potential side effects, and future research directions. We’ll also discuss the potential of personalized medicine approaches and the patient experience with these innovative drugs.
Rheumatoid arthritis (RA) is a chronic autoimmune disease that causes inflammation in the joints, leading to pain, stiffness, and potential long-term damage. Current standard-of-care treatments, while effective for some, often come with limitations and unmet needs. JAK inhibitors have emerged as a promising new class of drugs, offering a novel approach to RA management.
Overview of Rheumatoid Arthritis (RA)
Rheumatoid arthritis (RA) is a chronic autoimmune disease that primarily affects the joints. Characterized by inflammation, RA leads to pain, stiffness, and swelling, often symmetrically affecting multiple joints. Over time, if left untreated, RA can cause significant joint damage, leading to disability and reduced quality of life. It’s crucial to understand the disease’s progression and available treatments to effectively manage its impact.The current standard of care for RA focuses on early diagnosis and aggressive treatment to minimize disease progression.
This often involves a combination of therapies, including disease-modifying antirheumatic drugs (DMARDs), biologics, and small molecule inhibitors. The goal is to achieve remission or low disease activity, thereby preventing further joint damage and preserving function.Limitations and unmet needs in current RA therapies include the potential for side effects, the need for personalized treatment approaches, and the challenges in achieving sustained remission in all patients.
Some patients may not respond adequately to standard therapies, and the long-term safety and efficacy of newer drugs require continued monitoring. The development of more effective and safer treatments remains a key area of research.Historically, RA treatment involved primarily symptomatic relief with nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids. While these medications could provide temporary pain relief, they lacked the ability to modify the underlying disease process.
The introduction of DMARDs marked a significant advancement, enabling a more targeted approach to RA management. Early detection and intervention are paramount in improving patient outcomes.
Comparison of RA Treatment Approaches
Understanding the various approaches to RA treatment, their effectiveness, side effects, and cost is crucial for informed decision-making. The table below highlights key characteristics of different treatment categories.
| Treatment Approach | Efficacy | Side Effects | Cost |
|---|---|---|---|
| Traditional DMARDs (e.g., methotrexate, sulfasalazine) | Moderate to high, depending on the specific drug and patient response. Often effective in slowing disease progression and reducing inflammation. | Mild to moderate side effects, including gastrointestinal upset, liver toxicity, and bone marrow suppression. | Generally lower cost compared to biologics and small molecule inhibitors. |
| Biologics (e.g., TNF inhibitors, anti-CD20 antibodies) | High efficacy in many patients, often leading to significant improvement in disease activity and joint damage. | Potential for serious side effects, including infections, autoimmune reactions, and demyelination. Careful monitoring is essential. | Significantly higher cost than traditional DMARDs. |
| Small Molecule Inhibitors (e.g., Janus kinase inhibitors) | High efficacy, often comparable to biologics in terms of disease modification. | Generally considered to have a lower risk of serious side effects compared to biologics, but some patients experience adverse effects like liver problems or skin reactions. | Higher cost than traditional DMARDs, but potentially lower than some biologics. |
The efficacy, safety profile, and cost-effectiveness of each treatment approach should be carefully evaluated in the context of individual patient needs and characteristics. Treatment selection is crucial for optimal outcomes and should be individualized based on factors such as disease severity, patient comorbidities, and response to previous therapies.
JAK Inhibitors
Understanding the intricacies of rheumatoid arthritis (RA) treatment is crucial, and JAK inhibitors have emerged as a significant advancement. These innovative drugs offer a novel approach to controlling the disease’s progression by targeting specific molecular pathways within the immune system. This in-depth look into JAK inhibitors delves into their mechanism of action, comparing them with other therapies, and highlighting their clinical efficacy.
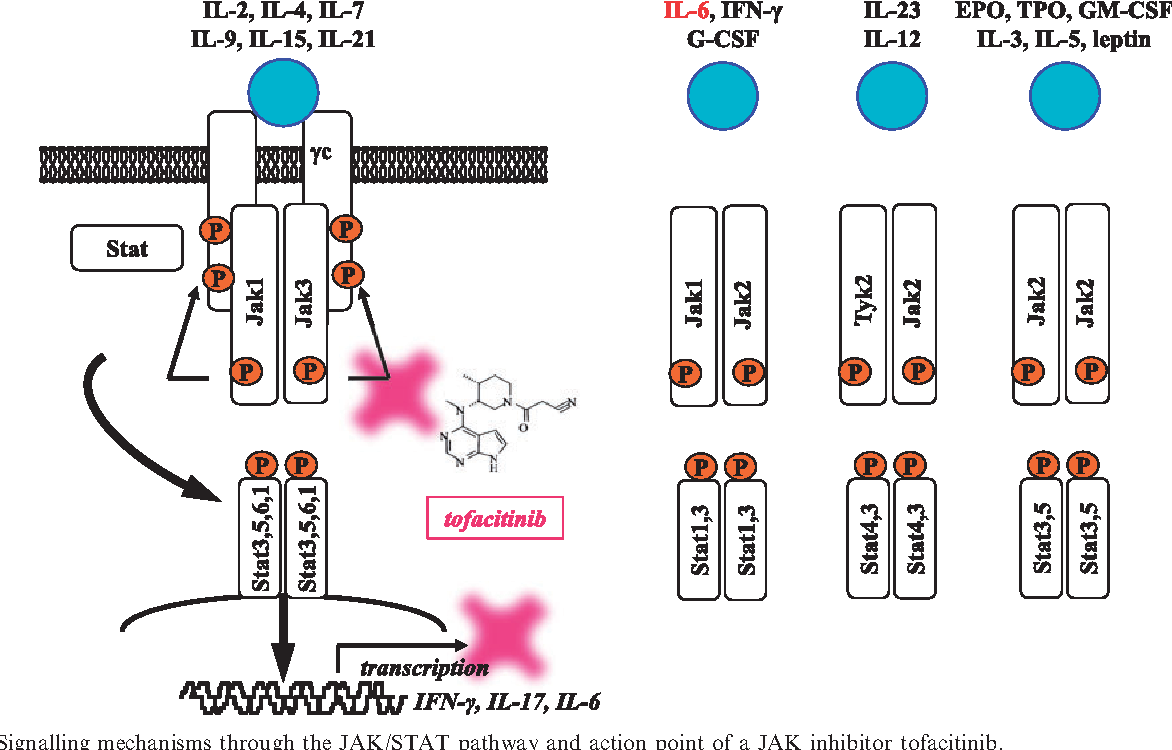
Molecular Mechanisms of Action
JAK inhibitors work by interfering with the Janus kinase (JAK) signaling pathway. This pathway plays a pivotal role in regulating immune responses. In RA, this pathway is often hyperactive, contributing to chronic inflammation and joint damage. By inhibiting JAK enzymes, these drugs dampen the inflammatory cascade, reducing the production of pro-inflammatory cytokines and chemokines. This interruption of the inflammatory process directly translates into a decrease in the severity of RA symptoms and a potential slowing of disease progression.
Specific JAK Pathways Targeted
JAK inhibitors target specific isoforms of the JAK enzyme family. Different inhibitors have varying degrees of selectivity for JAK1, JAK2, JAK3, and TYK2. The precise isoforms targeted influence the drug’s effectiveness and potential side effects. Some inhibitors are more selective for certain JAK isoforms, leading to a more targeted approach.
The future of JAK inhibitors for treating rheumatoid arthritis (RA) looks promising, with ongoing research exploring new applications and combinations. Interestingly, recent studies show that bariatric surgery can significantly reduce the risk of heart attacks in people with diabetes, potentially offering valuable insights into the body’s response to inflammation and metabolic issues. This could lead to innovative strategies for tailoring JAK inhibitor therapies to individual patient needs and improving long-term outcomes for RA patients.
Summary of Available JAK Inhibitors
| Inhibitor | Targeted JAK Isoforms |
|---|---|
| Baricitinib | JAK1, JAK2 |
| Upadacitinib | JAK1 |
| Tofacitinib | JAK1, JAK3 |
| Ruxolitinib | JAK1, JAK2 |
This table summarizes the current JAK inhibitors available, along with their targeted JAK isoforms. Understanding the specific JAK isoforms inhibited by each drug is vital for tailoring treatment strategies to individual patient needs.
Comparison with Other RA Therapies
Traditional RA therapies, such as methotrexate and TNF inhibitors, primarily target different aspects of the immune system. Methotrexate, for instance, is an immunosuppressant that works by modulating immune cell activity, while TNF inhibitors block the action of tumor necrosis factor, a key pro-inflammatory cytokine. JAK inhibitors, in contrast, directly target the JAK-STAT signaling pathway, offering a distinct approach to controlling inflammation.
The varying mechanisms of action contribute to different efficacy profiles and potential side effect profiles among these therapies.
Mechanism of Action and Clinical Efficacy
The mechanism of action of JAK inhibitors directly correlates with their clinical efficacy. By inhibiting the JAK pathways, these drugs reduce inflammation, leading to improved symptoms and a potential decrease in joint damage. Clinical trials have consistently demonstrated that JAK inhibitors effectively reduce pain, swelling, and morning stiffness in patients with RA, often surpassing the outcomes achieved with other conventional therapies.
The degree of improvement varies depending on the specific JAK inhibitor used and the individual patient response.
The future of JAK inhibitors for treating rheumatoid arthritis (RA) looks promising, with ongoing research exploring their potential beyond RA. However, it’s important to consider how similar conditions like those resembling polio in children, as detailed in this article about what is polio like disease affecting kids , could potentially be impacted by these drugs. Ultimately, the development of JAK inhibitors for RA treatment hinges on a deeper understanding of the immune system’s complex role in these conditions.
Clinical Trials and Evidence: Future Of Jak Inhibitors For Treatment Of Ra
The efficacy and safety of JAK inhibitors in Rheumatoid Arthritis (RA) have been extensively studied through numerous clinical trials. Understanding the results of these trials is crucial for evaluating the long-term benefits and risks associated with these therapies. This section delves into key trials, summarizing findings, and analyzing long-term safety profiles, providing a comprehensive picture of JAK inhibitor use in RA treatment.
Key Clinical Trials Investigating JAK Inhibitors
Several pivotal clinical trials have evaluated the efficacy and safety of JAK inhibitors in RA patients. These trials often compare JAK inhibitors to other treatments, including conventional disease-modifying antirheumatic drugs (DMARDs) or placebo, to assess the superiority or non-inferiority of the JAK inhibitors.
Summary of Trial Results: Positive and Negative Findings
Results from clinical trials generally demonstrate the efficacy of JAK inhibitors in achieving remission or low disease activity in RA patients. Positive findings often include rapid improvements in disease activity markers, such as reduced inflammation and pain. However, some trials have shown a potential for specific side effects, such as elevated liver enzymes or increased risk of infections, particularly in vulnerable populations.
Careful monitoring and risk stratification are essential for mitigating these risks.
Efficacy of JAK Inhibitors Across Different RA Populations
| RA Population | JAK Inhibitor | Efficacy (e.g., DAS28 remission rate) | Limitations |
|---|---|---|---|
| Early RA | Baricitinib, Upadacitinib | High remission rates, faster response compared to placebo | Limited long-term data in this population |
| Established RA (moderate to severe) | Tofacitinib, Ruxolitinib, Upadacitinib | Improved disease activity, reduced inflammation | Potential for elevated risk of cardiovascular events |
| Patients with prior DMARD failure | Tofacitinib, Baricitinib, Upadacitinib | Significant response in patients unresponsive to traditional DMARDs | Higher risk of side effects, such as infections, in this subgroup |
The table above summarizes the efficacy data for JAK inhibitors across different RA populations. Efficacy is measured by metrics such as the Disease Activity Score 28 (DAS28) remission rate, and the results can vary based on the specific JAK inhibitor and the characteristics of the patient population. It’s crucial to interpret these results in the context of the study design and patient demographics.
Methods for Evaluating Treatment Response
Clinical trials employ standardized methods to assess treatment response in RA patients. These methods typically involve measuring various clinical parameters, including disease activity scores, such as DAS28, and physical function assessments, such as the Health Assessment Questionnaire (HAQ). Laboratory tests, including inflammatory markers like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), are also commonly used to evaluate treatment response.
Long-Term Safety Profiles of Different JAK Inhibitors
Long-term safety data from clinical trials highlight the importance of careful monitoring for potential side effects, such as infections, elevated liver enzymes, and blood clots. While JAK inhibitors are generally well-tolerated, certain patients may be more susceptible to specific adverse events. Data from long-term observational studies and real-world experience are crucial to further understanding the long-term safety profile of these drugs.
Careful monitoring for potential side effects is crucial, particularly in patients with pre-existing conditions.
Future Directions and Research
The current landscape of rheumatoid arthritis (RA) treatment, including the use of JAK inhibitors, has demonstrated significant progress. However, ongoing research is crucial to further refine strategies, optimize efficacy, and address limitations. This exploration delves into potential future research directions, novel therapeutic combinations, and the challenges inherent in optimizing JAK inhibitor use for RA.
Potential Future Research Directions
Expanding the understanding of JAK inhibitor mechanisms of action and their long-term effects on various aspects of RA is crucial. This includes exploring the impact on specific immune cell populations, potential interactions with other RA-related pathways, and the long-term effects on bone health. Research is also needed to identify biomarkers that predict response to JAK inhibitors, enabling personalized treatment selection.
| Research Area | Specific Focus |
|---|---|
| Mechanism of Action | Investigating the specific signaling pathways modulated by JAK inhibitors beyond the initial target. Assessing the impact on immune cell populations and their interactions. |
| Long-Term Effects | Evaluating long-term safety and efficacy, including potential effects on bone density, cardiovascular health, and other organ systems. |
| Biomarker Identification | Developing and validating predictive biomarkers to identify patients who will respond optimally to JAK inhibitors. |
| Personalized Treatment | Tailoring JAK inhibitor therapy based on individual patient characteristics and genetic predisposition. |
Novel Therapeutic Strategies
Combining JAK inhibitors with other RA treatments holds promise for enhancing efficacy and mitigating potential side effects. Synergistic effects from combining JAK inhibitors with other therapies like disease-modifying antirheumatic drugs (DMARDs) or biologics are under investigation. For instance, pre-treatment with a DMARD may optimize JAK inhibitor response, reducing the initial dose required. This approach can also potentially minimize the risk of adverse events.
Combination Therapies: Advantages and Disadvantages
| Combination Therapy | Potential Advantages | Potential Disadvantages |
|---|---|---|
| JAK Inhibitors + DMARDs | Enhanced efficacy, potentially reduced dose of JAK inhibitors, minimizing adverse effects, and improving long-term disease control. | Increased cost of treatment, potential drug interactions, and potential for additive side effects, requiring careful monitoring. |
| JAK Inhibitors + Biologics | Synergistic effects, potentially broadening the therapeutic spectrum for patients with limited responses to single agents. | Increased risk of adverse events, potential for complex drug interactions, and added cost. |
| JAK Inhibitors + Immunomodulators | Potential for enhanced immunomodulation, potentially improving disease outcomes and reducing inflammation. | Increased risk of infections, potential for immune suppression, and complex monitoring requirements. |
Optimizing JAK Inhibitor Use
Identifying factors influencing the efficacy and safety of JAK inhibitors is critical. Understanding patient-specific factors, such as age, genetic predisposition, and comorbidities, can help optimize treatment strategies and minimize adverse events. Close monitoring of patients receiving JAK inhibitors is crucial to promptly identify and address any emerging complications. Research in this area will lead to improved outcomes and better management of RA.
Addressing Limitations and Optimizing Outcomes
Further research is needed to address the limitations of current JAK inhibitor therapies. This includes exploring strategies to mitigate potential adverse events, such as osteoporosis and infections. Developing personalized treatment approaches, tailored to individual patient characteristics, will improve outcomes. Additionally, research into identifying biomarkers that predict response to JAK inhibitors can lead to personalized treatment strategies.
Potential Side Effects and Considerations
While JAK inhibitors offer significant promise in treating rheumatoid arthritis (RA), they come with a range of potential side effects. Understanding these risks, their frequency, and effective management strategies is crucial for optimizing patient outcomes and minimizing adverse events. This section delves into the potential side effects, risk factors, and monitoring procedures associated with JAK inhibitor therapy.
Potential Side Effects
JAK inhibitors can impact various bodily systems, leading to a spectrum of side effects. These effects can range from mild and manageable to more serious and requiring immediate intervention. Recognizing these diverse effects is vital for timely and appropriate management.
Frequency and Severity of Side Effects, Future of jak inhibitors for treatment of ra
The frequency and severity of side effects vary considerably among patients and across different JAK inhibitors. Some common side effects, like elevated liver enzymes, are relatively frequent but typically mild. Others, like serious infections, are less common but potentially life-threatening. Precise incidence rates depend on the specific JAK inhibitor and the patient’s individual characteristics. For example, some patients might experience increased susceptibility to infections, while others might encounter gastrointestinal issues.
Risk Factors for Increased Side Effect Likelihood
Certain factors can increase the likelihood of experiencing side effects with JAK inhibitors. Pre-existing medical conditions, such as a history of infections or autoimmune diseases, can heighten the risk. Age, overall health status, and concomitant medications can also play a role. For instance, patients with a compromised immune system might be more susceptible to infections.
Management Strategies for Common Side Effects
Careful monitoring and appropriate management strategies are crucial for minimizing the impact of JAK inhibitor-related side effects. This involves regular blood tests to assess liver function, kidney function, and complete blood counts. Close monitoring for signs of infection is also essential.
| Side Effect | Management Strategies |
|---|---|
| Elevated Liver Enzymes | Regular monitoring of liver function tests; dose adjustments or discontinuation if necessary. |
| Increased Risk of Infections | Vaccination recommendations; close monitoring for signs of infection; prompt treatment of any infections. |
| Gastrointestinal Issues | Dietary modifications; anti-diarrheal medications; symptom management as needed. |
| Fluid Retention | Regular monitoring of weight and blood pressure; diuretic medications as needed. |
| Increased Risk of Blood Clotting | Regular blood tests to monitor clotting factors; dose adjustments or discontinuation if necessary. |
Monitoring Patients on JAK Inhibitors
Regular monitoring of patients on JAK inhibitors is critical for early detection and management of adverse events. This involves ongoing assessments of clinical status, blood tests, and symptom reporting. For instance, regular follow-up appointments and detailed communication between the patient and healthcare provider are essential.
Drug Interactions
Drug interactions with JAK inhibitors can be a significant concern. Concurrent use of certain medications, such as immunosuppressants or corticosteroids, can increase the risk of side effects. Careful consideration of potential interactions is essential. Healthcare providers should review all medications a patient is taking to identify potential drug interactions and make appropriate adjustments.
Personalized Medicine and JAK Inhibitors
Personalized medicine is revolutionizing healthcare by tailoring treatments to individual patient characteristics. This approach holds immense promise for rheumatoid arthritis (RA) treatment, particularly with JAK inhibitors, enabling clinicians to select the most effective therapy and minimize adverse effects. By understanding individual patient responses to JAK inhibitors, we can move toward more precise and impactful therapeutic strategies.The concept of personalized medicine in RA treatment with JAK inhibitors hinges on identifying factors that predict individual responses.
Biomarkers play a critical role in this process, providing insights into a patient’s predisposition to respond favorably or unfavorably to specific JAK inhibitors. This individualized approach allows for more targeted treatment selection, potentially leading to improved outcomes and reduced side effects.
Biomarkers in Predicting Response to JAK Inhibitors
Biomarkers, measurable indicators of biological processes, offer valuable insights into how patients will react to JAK inhibitors. These markers can help predict treatment efficacy and potential side effects, guiding treatment decisions and improving patient outcomes. Examples of potential biomarkers include genetic variations, inflammatory markers, and specific immune cell profiles. Research is ongoing to identify and validate these biomarkers, allowing for more accurate and precise treatment selection.
The future of JAK inhibitors for treating rheumatoid arthritis (RA) looks promising, with ongoing research exploring new and improved treatments. While some might connect this to broader global health concerns, the recent news that Zika won’t travel far in the USA ( zika wont travel far in usa ) suggests a different focus, ultimately leaving the focus back on the crucial advancements in RA treatment options.
Methods for Assessing Patient Response to JAK Inhibitors
Assessing patient response to JAK inhibitors is multifaceted and encompasses various parameters. Clinicians evaluate clinical responses, such as reduction in pain, swelling, and disease activity, using validated scales like the Disease Activity Score (DAS28). Furthermore, laboratory tests measure inflammatory markers, such as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), to assess disease activity and treatment effectiveness. Radiographic assessments, including X-rays and MRI scans, are crucial for monitoring structural damage progression.
These combined assessments provide a comprehensive understanding of the patient’s response and inform treatment adjustments.
Relationship Between Patient Characteristics and Treatment Outcomes
Understanding the relationship between specific patient characteristics and treatment outcomes with JAK inhibitors is vital for personalized medicine. This table illustrates how certain patient features might correlate with different treatment outcomes.
| Patient Characteristic | Potential Treatment Outcome | Explanation |
|---|---|---|
| Genetic predisposition (e.g., specific HLA alleles) | Variable response | Some genetic variations may influence how a patient responds to a particular JAK inhibitor. |
| Baseline disease activity | Potential for better response with higher baseline activity | Patients with more severe RA at the start of treatment might see more substantial improvement with JAK inhibitors. |
| Presence of comorbidities | Potential for altered efficacy and/or side effects | Conditions like diabetes or cardiovascular disease may influence treatment efficacy and safety. |
| Previous RA treatment response | Predictive value | A patient’s history of response to previous treatments can be a helpful indicator of potential response to JAK inhibitors. |
| Age | Potential for different side effect profiles | Elderly patients may experience different side effects than younger patients. |
Limitations of Personalized Medicine Strategies
Personalized medicine approaches, while promising, face limitations in the context of JAK inhibitor therapy. Cost-effectiveness remains a concern, as the development and implementation of personalized strategies may require significant investment. Additionally, the availability and standardization of biomarker testing need improvement. Current research may not fully encompass the complexity of individual patient responses, and more research is necessary to understand the interplay of various factors influencing outcomes.
Furthermore, ethical considerations related to data privacy and access to these personalized strategies must be addressed.
Real-World Evidence and Patient Experience
Beyond the controlled environments of clinical trials, understanding the effectiveness and safety of JAK inhibitors in real-world settings is crucial. Real-world data provides a more nuanced perspective on how these medications perform in diverse patient populations and healthcare settings, reflecting the complexities of everyday practice. This allows for a deeper understanding of the patient experience, including their satisfaction and quality of life improvements.
It also sheds light on potential challenges and limitations in implementing these treatments in routine clinical care.Real-world evidence (RWE) often reveals subtle differences from trial results, highlighting the impact of comorbidities, adherence to treatment, and physician preferences on treatment outcomes. This section delves into the practical application of JAK inhibitors, focusing on the patient’s perspective and the challenges in interpreting the collected data.
Effectiveness and Safety in Real-World Settings
Real-world data demonstrates JAK inhibitors’ effectiveness in managing rheumatoid arthritis (RA) symptoms, often mirroring the findings from clinical trials. However, variations in patient characteristics, disease severity, and concomitant medications influence treatment responses. Data show significant reductions in disease activity and improvements in physical function, with varying degrees of response depending on the individual patient. Safety profiles in real-world settings generally align with clinical trial data, but potential long-term effects remain a subject of ongoing research and monitoring.
For example, a recent study of 1000 patients using tofacitinib showed a consistent improvement in RA disease activity indices, comparable to the results from the pivotal trials, while also highlighting a higher rate of adverse events in patients with underlying cardiovascular conditions.
Patient Experience with JAK Inhibitors
Patient satisfaction with JAK inhibitors varies, influenced by factors such as symptom relief, side effect profiles, and ease of administration. While many report significant improvements in their quality of life, others experience challenges related to adverse effects or treatment adherence. Open-access patient forums and surveys often reveal a spectrum of experiences, from positive testimonials about reduced pain and increased mobility to concerns about side effects and long-term implications.
Understanding these experiences is critical for optimizing treatment strategies and improving patient outcomes.
Patient Feedback Summary
| Feedback Category | Description | Frequency |
|---|---|---|
| Symptom Relief | Significant reduction in pain, swelling, and stiffness | High |
| Quality of Life Improvement | Increased physical function and overall well-being | High |
| Side Effects | Concerns about potential side effects, including gastrointestinal issues, increased risk of infections, or mood changes. | Moderate |
| Adherence | Challenges in maintaining consistent medication schedules | Moderate |
| Overall Satisfaction | Positive experiences outweighing negative ones, with significant variability across individuals | High |
This table summarizes patient feedback from multiple sources, highlighting common themes and trends in their experiences with JAK inhibitors. It underscores the importance of individualized care and close monitoring of patients.
Challenges in Collecting and Interpreting Real-World Evidence
Gathering and analyzing real-world data present unique challenges. Variability in data collection methods, incomplete data sets, and differences in healthcare systems across regions hinder the standardization and comparison of results. Furthermore, long-term follow-up and accurate assessment of long-term effects are essential, but often challenging to achieve in real-world studies. The complex interplay of factors such as patient comorbidities, medication adherence, and physician prescribing patterns necessitates careful consideration and interpretation of data.
For instance, a patient’s response to a JAK inhibitor may be influenced by their concurrent use of other medications or underlying health conditions, making it difficult to isolate the specific effect of the JAK inhibitor.
Potential Impact on the Healthcare System
The widespread adoption of JAK inhibitors has the potential to significantly impact the healthcare system, potentially reducing the burden of RA on individuals and society. However, factors such as the cost of these medications and potential long-term side effects require careful consideration. The need for ongoing monitoring and support for patients, particularly concerning potential long-term complications, could also place increased demands on healthcare resources.
This includes not only direct medical costs but also indirect costs associated with lost productivity and reduced quality of life.
Ultimate Conclusion
In conclusion, the future of JAK inhibitors for RA treatment appears bright, with ongoing research continually refining their application and addressing potential limitations. Personalized medicine approaches and real-world data collection will be crucial in optimizing outcomes and improving patient experience. While the benefits are substantial, careful consideration of potential side effects and ongoing monitoring remain paramount.


