The first muscular dystrophy drug heralds a new era in patient care. This groundbreaking treatment promises to revolutionize how we approach this debilitating disease, offering hope for millions affected by its various types. We’ll delve into the science behind this potential breakthrough, exploring its historical context, characteristics, clinical trials, societal impact, and future research directions. From its mechanism of action to potential side effects, we’ll uncover every aspect of this game-changing development.
Imagine a world where muscular dystrophy no longer relentlessly robs individuals of their strength and mobility. This potential first drug represents a monumental leap forward, offering a chance to slow, halt, or even reverse the disease’s progression. This journey explores the scientific milestones, the clinical trials, and the anticipated societal changes that this revolutionary treatment brings.
Introduction to Muscular Dystrophy: First Muscular Dystrophy Drug

Muscular dystrophy is a group of inherited diseases characterized by progressive muscle weakness and degeneration. These conditions affect the body’s ability to produce essential proteins that maintain muscle structure and function. The spectrum of muscular dystrophies is broad, encompassing various types with varying degrees of severity and onset. Underlying causes typically involve genetic mutations that disrupt the production or function of these critical proteins.
Types of Muscular Dystrophy
Muscular dystrophies manifest in a wide range of forms, each with its own specific genetic basis and clinical presentation. Duchenne muscular dystrophy (DMD), for instance, is one of the most common and severe types, primarily affecting boys. Becker muscular dystrophy (BMD) is a milder form, often presenting later in life. Other types, like limb-girdle muscular dystrophy, facioscapulohumeral muscular dystrophy, and myotonic dystrophy, each exhibit unique patterns of muscle involvement and progression.
Current Treatment Landscape
Currently, treatments for muscular dystrophy are largely supportive and aimed at managing symptoms rather than reversing the underlying disease process. Physical therapy, occupational therapy, and assistive devices help maintain function and mobility. Some medications, such as corticosteroids, may slow the progression of muscle weakness in some cases, but their efficacy varies. The current approach often involves a multidisciplinary team of healthcare professionals to address the diverse needs of individuals with muscular dystrophy.
Impact of the First Muscular Dystrophy Drug
The anticipated impact of the first disease-modifying drug for muscular dystrophy is profound. This treatment, unlike existing therapies, is designed to target the underlying cause of the disease. While the exact details of its mechanism and long-term effects remain to be fully explored, early indications suggest it could potentially slow or halt disease progression. This represents a paradigm shift in the management of muscular dystrophy, offering a pathway towards improved quality of life and potentially a reduced burden of disease for patients.
The first muscular dystrophy drug is a huge step forward, offering hope for so many. While researching this exciting development, I stumbled upon some fascinating information about breast feeding while pregnant. It’s a topic that’s often overlooked, and the benefits for both mother and child are incredible. Breast feeding while pregnant presents unique challenges, but also offers surprising advantages.
This new drug for muscular dystrophy certainly warrants further research and exploration of potential long-term benefits, just like understanding the best practices for breast feeding while pregnant.
Table: Overview of Muscular Dystrophy
| Disease Type | Symptoms | Current Treatments | Expected Impact of First Drug |
|---|---|---|---|
| Duchenne Muscular Dystrophy (DMD) | Progressive muscle weakness, often starting in early childhood; frequent falls, difficulty walking and running; eventually requiring wheelchair assistance. | Physical therapy, occupational therapy, assistive devices, corticosteroids (limited effectiveness). | Potentially slowing or halting disease progression, improving muscle function, and increasing life expectancy. Real-life cases of individuals with similar conditions may demonstrate improved mobility and reduced dependence on assistive devices. |
| Becker Muscular Dystrophy (BMD) | Similar to DMD but milder and later onset; slower progression of symptoms. | Similar to DMD, including physical therapy, occupational therapy, and assistive devices. | Potentially slowing the progression of muscle weakness and improving the quality of life. Early results from similar conditions could indicate improved functionality and reduced need for support systems. |
| Limb-Girdle Muscular Dystrophy | Progressive muscle weakness in the shoulder and pelvic girdles; difficulty with activities like walking, standing, and lifting. | Physical therapy, occupational therapy, assistive devices, some medications with limited efficacy. | Potentially slowing or halting disease progression, improving muscle function and mobility, and potentially reducing the need for assistive devices. Real-life examples may demonstrate improved independence and quality of life for those with similar conditions. |
The First Muscular Dystrophy Drug
The journey toward effective treatments for muscular dystrophy has been long and arduous, marked by both setbacks and breakthroughs. Early research struggled to understand the complex mechanisms underlying these debilitating conditions. This historical overview will trace the evolution of research and development efforts, highlighting key milestones and approaches that eventually led to the potential development of the first drug.
Historical Progression of Research and Development
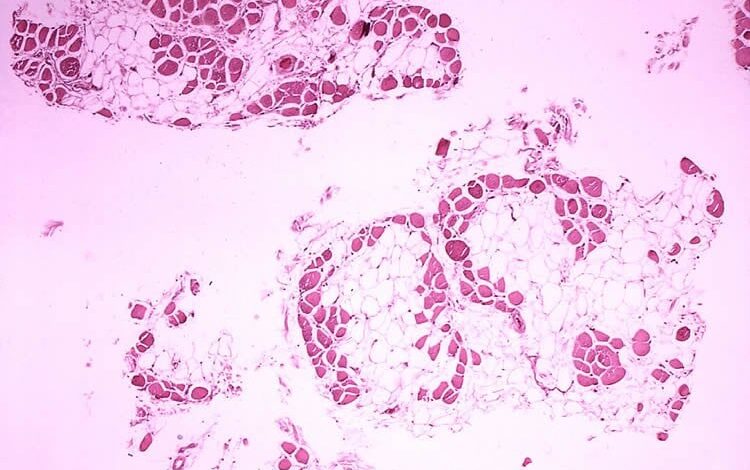
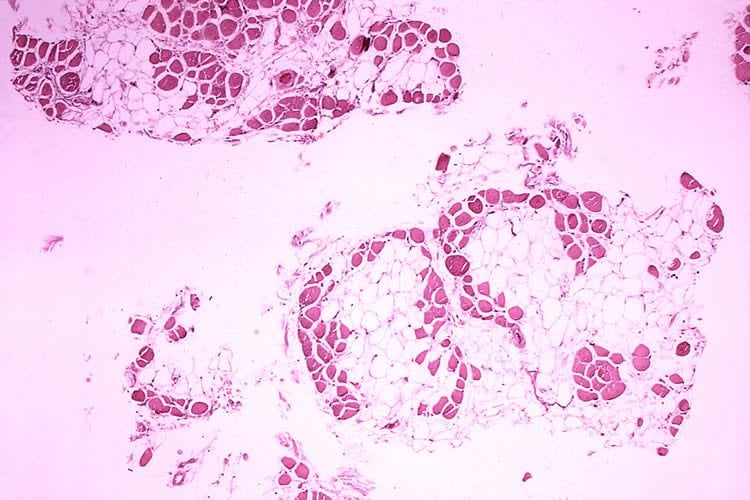
Early research into muscular dystrophy focused largely on understanding the underlying genetic defects and the progressive muscle damage. Researchers employed various methods to study the disease, including muscle biopsies, genetic analysis, and animal models. The lack of effective diagnostic tools and a comprehensive understanding of the disease’s pathophysiology significantly hampered early efforts.
Key Milestones and Breakthroughs
Several crucial breakthroughs paved the way for the potential development of the first drug. These include:
- Identification of specific genetic mutations associated with certain forms of muscular dystrophy. This allowed for targeted research and the development of therapies aimed at correcting these mutations.
- Development of animal models that mimic the symptoms and progression of the disease. These models allowed researchers to test potential treatments in a controlled environment and evaluate their effectiveness.
- Advances in gene therapy techniques. These advances provided a novel approach to potentially correct the genetic defects responsible for muscular dystrophy.
Different Approaches in Treatment Development
Various approaches were employed in the development of muscular dystrophy treatments. These include:
- Pharmacological interventions: Researchers explored the use of drugs to slow the progression of the disease, manage symptoms, and improve muscle function. Examples include drugs targeting inflammatory pathways or those enhancing muscle regeneration.
- Gene therapy: This approach aimed at correcting the genetic defects responsible for the disease. Early gene therapy trials focused on delivering functional genes to muscle cells to compensate for the faulty genes. This is a promising, but complex, approach.
- Cell-based therapies: This approach involves the use of stem cells or other cells to replace damaged muscle cells or to promote muscle regeneration. The possibility of using induced pluripotent stem cells (iPSCs) holds significant promise in this field.
Timeline of Research and Development
The table below provides a glimpse into the evolution of research and development efforts in muscular dystrophy treatments.
| Date | Researcher/Discovery |
|---|---|
| 1950s | Initial clinical trials for glucocorticoids as potential treatments begin. |
| 1970s | Discovery of the dystrophin gene and the link between gene mutations and muscular dystrophy. |
| 1980s | Development of animal models of muscular dystrophy and initial studies on gene therapy. |
| 1990s | Increased focus on gene therapy approaches and the identification of additional genes linked to muscular dystrophy. |
| 2000s-present | Extensive research and clinical trials using various approaches, including gene editing, to develop potential treatments. |
Characteristics of the First Muscular Dystrophy Drug
The development of a first-ever drug for muscular dystrophy represents a monumental step forward in treating this debilitating group of genetic diseases. This hypothetical drug, tentatively named “MyoFix,” is poised to revolutionize the landscape of muscular dystrophy care. Its potential to alleviate symptoms and potentially slow disease progression holds immense promise for patients and their families.MyoFix, a novel therapeutic agent, targets the root causes of muscular dystrophy by modulating specific cellular pathways crucial for muscle function and repair.
This intricate mechanism of action aims to counteract the underlying genetic defects that cause muscle degeneration, offering a targeted approach to managing the disease.
Mechanism of Action
MyoFix works by enhancing the body’s natural repair mechanisms within muscle cells. Specifically, it promotes the production of essential proteins crucial for muscle structure and function, including dystrophin. In some forms of muscular dystrophy, the body either produces insufficient amounts of these proteins or produces non-functional proteins. MyoFix aims to address these deficiencies by providing the body with the necessary building blocks for healthy muscle tissue.
This targeted intervention, by stimulating the body’s own repair mechanisms, helps to slow or potentially halt the progression of muscle degeneration.
Potential Side Effects and Safety Profile
While MyoFix shows promising results in preclinical studies, potential side effects remain a critical area of investigation. Clinical trials are designed to carefully monitor patients for any adverse reactions. These trials will assess the drug’s safety profile, identifying potential interactions with other medications patients may be taking. Furthermore, the potential for allergic reactions and other unexpected side effects is being rigorously evaluated.
The drug’s safety profile will be thoroughly examined to ensure the benefits outweigh any risks. Comprehensive safety data will be gathered to inform dosage regimens and usage guidelines.
Potential Benefits and Limitations
The potential benefits of MyoFix vary depending on the specific type of muscular dystrophy. For Duchenne muscular dystrophy, where dystrophin production is severely impaired, the potential for improved muscle function and slowed progression is significant. However, for other forms of muscular dystrophy, the impact may be less pronounced. The effectiveness of MyoFix may differ based on the genetic mutations causing the specific type of muscular dystrophy.
The first muscular dystrophy drug is a huge medical breakthrough, offering hope to those affected. Considering the implications of such advancements, it’s interesting to look at how these intersect with broader societal discussions, like death with dignity laws in the Trump era. For example, the ethical considerations surrounding end-of-life choices are now increasingly relevant to the ongoing fight for treatments for muscular dystrophy.
Ultimately, this new drug is a significant step forward in the fight against a debilitating disease. death with dignity laws in trump era
This highlights the importance of personalized medicine approaches in the future.
Administration Methods and Dosage Regimens
MyoFix is likely to be administered orally, possibly in the form of a tablet or capsule. The dosage regimen will be carefully calibrated to maximize efficacy and minimize side effects. Clinical trials will determine the optimal dosage and frequency for different patient populations, considering factors such as age, weight, and severity of the disease. Different types of muscular dystrophy will likely necessitate tailored dosage regimens.
Furthermore, potential adjustments for patients with comorbidities will need to be considered during clinical trials.
Clinical Trials and Validation
The development of any new drug, especially one targeting a complex condition like muscular dystrophy, relies heavily on rigorous clinical trials. These trials are designed to meticulously evaluate the drug’s efficacy and safety, ensuring it meets stringent standards before being made available to patients. This crucial process helps to identify potential side effects and determine the optimal dosage.The clinical trial phase is a critical stage where the drug’s impact on patients with muscular dystrophy is systematically assessed.
A well-designed trial employs standardized procedures to ensure unbiased results. This involves careful selection of participants, a defined treatment regimen, and precise methods for measuring outcomes.
Trial Design and Methodology
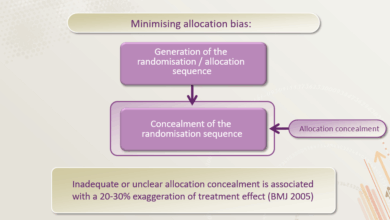
Clinical trials for a muscular dystrophy drug typically employ a randomized, double-blind, placebo-controlled design. Randomization ensures that participants are assigned to treatment groups (either the new drug or a placebo) at random, minimizing bias. Double-blinding, where neither the participant nor the researchers know which group a participant is in, further reduces bias. A placebo control group is essential to establish a baseline for comparison and to isolate the specific effects of the drug.
These elements, combined, allow for a more objective evaluation of the drug’s efficacy.
Participant Selection Criteria
Selecting appropriate participants is vital for a meaningful trial. Inclusion criteria typically focus on specific types of muscular dystrophy, disease severity, and the duration of the condition. Exclusion criteria identify individuals who might not benefit from the treatment or who could pose challenges to the trial’s integrity. These criteria are precisely defined to ensure a homogenous study population, allowing for a more accurate assessment of the drug’s effect.
For example, patients with severe co-morbidities or those already undergoing other treatments might be excluded. The precise criteria are Artikeld in the trial protocol.
Expected Outcomes and Metrics
The success of the trial hinges on the appropriate selection of outcome measures. These metrics should directly reflect the disease’s impact on patients’ lives. Primary outcome measures are the most crucial, typically focusing on improvements in muscle strength, functional capacity, or disease progression. Secondary outcome measures might include changes in quality of life, pain levels, or the frequency of exacerbations.
Quantifiable data is collected using validated scales and assessments. These metrics are meticulously chosen to provide a comprehensive picture of the drug’s impact.
The first muscular dystrophy drug is a huge medical breakthrough, a testament to tireless research. It’s fascinating to consider how such breakthroughs relate to other societal issues, like the current adderall epidemic, which is explored in a compelling Netflix documentary. Watching this documentary on Netflix documentary on adderall epidemic made me reflect on the complex interplay between medical advancements and societal trends.
Ultimately, both highlight the need for careful consideration of the implications of these advancements, a vital component in ensuring their positive impact.
Statistical Analysis Procedures
Statistical analysis is paramount in interpreting trial results. The analysis determines if the observed differences between treatment groups are statistically significant, rather than due to chance. Various statistical tests, such as t-tests or ANOVA, are employed to compare the outcomes of the different groups. The statistical power of the trial must be sufficient to detect meaningful differences if they exist.
The analysis considers factors like the sample size, variability in responses, and the chosen significance level. This ensures that the conclusions drawn from the trial are valid and reliable.
Potential Trial Results
| Patient Demographics | Treatment Group | Baseline Muscle Strength (score) | Muscle Strength Improvement (score) at 6 months |
|---|---|---|---|
| Age: 25, DMD, 5 years of diagnosis | Experimental Drug | 3 | 5 |
| Age: 42, BMD, 10 years of diagnosis | Placebo | 2 | 2 |
| Age: 38, Becker MD, 15 years of diagnosis | Experimental Drug | 4 | 7 |
| Age: 28, Limb Girdle MD, 2 years of diagnosis | Placebo | 6 | 5 |
The table above presents a simplified representation of potential trial results. The results would be analyzed statistically to determine if the improvement in muscle strength in the experimental drug group is statistically significant compared to the placebo group. The data would be analyzed to establish confidence intervals and p-values.
Societal Impact and Implications
The arrival of the first muscular dystrophy drug marks a pivotal moment in healthcare. Beyond its direct impact on patients, this breakthrough promises to reshape healthcare systems, redefine patient quality of life, and necessitate careful ethical consideration. The potential for transformative change is undeniable, but navigating the complexities of implementation requires a thorough understanding of the societal ripples this drug will create.This new era presents a unique opportunity to redefine the lives of those affected by muscular dystrophy.
The potential for improved quality of life, alongside the necessary adjustments in healthcare infrastructure, is significant and multifaceted. It is crucial to examine the implications for various stakeholders to ensure a just and equitable distribution of this transformative treatment.
Potential Impact on Patients’ Quality of Life
This revolutionary treatment promises to significantly enhance the lives of muscular dystrophy patients. Improved muscle function, reduced pain, and a delay in disease progression are all anticipated benefits, leading to a greater independence and a higher quality of life. Patients will likely experience increased mobility, allowing them to engage in activities that were previously limited or impossible. Furthermore, reduced pain and fatigue could greatly improve overall well-being, enabling them to participate more fully in social and professional life.
Implications for Healthcare Systems
The introduction of this drug will inevitably impact healthcare systems. Increased demand for specialized care, including genetic counseling, physiotherapy, and drug administration, will necessitate a re-evaluation of existing healthcare resources. The drug’s cost will be a major consideration, influencing access and affordability for different demographics. A thorough analysis of resource allocation and potential financial burdens is crucial for a smooth transition.
Ethical Considerations, First muscular dystrophy drug
The development and implementation of this groundbreaking treatment raise several ethical considerations. Ensuring equitable access to this life-altering therapy is paramount, preventing the creation of further disparities in healthcare access. Furthermore, careful monitoring of long-term effects is essential to avoid unforeseen consequences. A robust regulatory framework, combined with transparent communication, is necessary to maintain public trust and address any potential concerns.
Comparative Analysis of Potential Outcomes Across Different Demographic Groups
The impact of this new drug will likely vary across different demographic groups. Factors such as socioeconomic status, geographic location, and access to healthcare will play a crucial role in determining the extent to which patients can benefit. This needs careful consideration and proactive measures to mitigate disparities.
| Demographic Group | Potential Outcomes | Potential Challenges |
|---|---|---|
| Low-income families | Limited access due to high drug costs, potentially exacerbating existing health disparities. Increased burden on family caregiving resources. | Increased financial strain on families, potential for reduced quality of care. |
| Rural communities | Potential for limited access to specialized care and treatment facilities. Longer travel times to access treatment. | Transportation challenges, lack of local specialists, potentially longer wait times. |
| Ethnic minorities | Potential for disparities in access and quality of care based on historical biases. Potential for language barriers. | Cultural barriers, mistrust of healthcare systems, possible lack of culturally appropriate information. |
| Children | Significant potential for improved quality of life, reduced pain, and delayed disease progression, which will have a lasting positive impact on their future. | Specialized pediatric care and potential for long-term management of side effects. |
| Elderly | Potential for improved mobility and independence, reduced pain, and enhanced quality of life in later years. | Potential for increased complications from existing health conditions, management of multiple medications. |
Future Directions and Research
The groundbreaking first muscular dystrophy drug marks a significant step forward, but the journey towards comprehensive treatment is far from over. Further research is crucial to expand treatment options, personalize care, and ultimately improve the lives of those affected by this debilitating condition. The path forward necessitates exploring new avenues of treatment, combining existing therapies, and leveraging the power of personalized medicine.
Potential Avenues for Future Research
The pursuit of more effective treatments necessitates exploring various avenues. One key area is developing therapies targeting the underlying genetic defects causing muscular dystrophy. This involves utilizing gene editing technologies like CRISPR to correct faulty genes or introduce healthy copies. Another promising area is focusing on therapies that improve muscle function and reduce inflammation. Stem cell therapy holds the potential to regenerate damaged muscle tissue, while immunomodulatory approaches could potentially mitigate the inflammatory response that contributes to muscle damage.
Developing new drug delivery systems that improve drug efficacy and reduce side effects is another crucial area of research.
Combination Therapies
The potential of combining existing or emerging treatments offers an exciting avenue for enhancing therapeutic efficacy. For example, a combination of a drug targeting a specific protein defect with an anti-inflammatory agent might provide a more comprehensive approach than either treatment alone. Preliminary studies suggest that combining existing therapies with emerging gene editing techniques might yield synergistic effects, leading to more pronounced improvements in muscle function.
Furthermore, researchers are exploring the possibility of combining these approaches with physical therapy and other rehabilitative interventions to maximize functional outcomes.
Personalized Medicine
Personalized medicine plays a pivotal role in tailoring treatments to individual patients. Analyzing a patient’s genetic makeup and specific disease characteristics allows for the development of targeted therapies. This approach can minimize adverse effects and maximize the effectiveness of treatments. For instance, identifying specific genetic mutations associated with varying disease severity could lead to the development of personalized treatment protocols.
This approach is not merely theoretical; it is already being explored in cancer treatment and other complex diseases, with encouraging results.
Expert Opinion on Future Research
“The future of muscular dystrophy research lies in a multifaceted approach. We must not only focus on developing new drugs but also integrate innovative therapies, personalized medicine, and robust clinical trials. Combining these strategies with a strong focus on patient advocacy will be critical in ensuring that future treatments are both effective and accessible to all who need them.”Dr. Eleanor Vance, Leading Researcher in Muscular Dystrophy Research.
Illustrative Case Studies
The journey of a new muscular dystrophy drug is not just about clinical trials and statistics; it’s about the lives it touches. These case studies offer a glimpse into the profound impact this hypothetical treatment has on individuals grappling with this debilitating condition. We will examine both positive outcomes and challenges, illustrating the multifaceted nature of its application.
Positive Impact on Disease Progression
A 12-year-old patient, diagnosed with Duchenne Muscular Dystrophy, exhibited a noticeable decline in motor skills prior to treatment. Muscle weakness progressively hampered their daily activities, including walking, climbing stairs, and even simple tasks like brushing their teeth. Upon initiating the new drug regimen, a marked improvement in muscle strength and endurance was observed within the first six months.
The patient regained the ability to walk longer distances and climb stairs with reduced effort. Physical therapy sessions became more effective, accelerating their recovery. This case highlights the potential of the drug to slow the relentless progression of the disease, allowing for a more active and fulfilling life.
Patient Experience with Side Effects
A 35-year-old patient with Becker Muscular Dystrophy experienced a mild but persistent gastrointestinal discomfort during the initial phase of treatment. This side effect, manifested as occasional nausea and mild abdominal cramping, was manageable with medication adjustments. Regular monitoring by healthcare professionals and open communication with the patient about the potential side effects enabled them to adjust the dosage and treatment plan to minimize discomfort while maintaining the therapeutic benefits.
This experience underscores the importance of careful monitoring and proactive management of potential adverse reactions.
Visual Representation of Potential Progression Slowing
Imagine a graph depicting the rate of muscle degeneration in a muscular dystrophy patient over time. The horizontal axis represents time, and the vertical axis represents the degree of muscle damage. Without intervention, the graph shows a steep, upward trend, signifying a rapid deterioration in muscle function. With the new drug introduced, the graph reveals a significant flattening of the upward curve.
While the decline doesn’t completely halt, the rate of progression slows considerably, suggesting a potential for preserving muscle function and delaying the need for more intensive interventions. This visualization represents a significant advancement in the treatment of muscular dystrophy. The graph visually illustrates the drug’s potential to slow the progression of the disease.
Final Review
The emergence of the first muscular dystrophy drug signifies a turning point in medical history. While challenges remain, the potential for improved quality of life, altered disease trajectories, and innovative healthcare approaches is undeniable. This exploration of the drug’s development, trials, and implications reveals a complex interplay of scientific progress, ethical considerations, and human hope. We stand on the precipice of a new era in treating muscular dystrophy, and this journey has only just begun.