Rheumatoid arthritis clinical trials are crucial for advancing treatments and understanding this complex disease. This exploration delves into the intricacies of these trials, from their various phases and methodologies to the ethical considerations and emerging trends. We’ll examine the pivotal role of stakeholders, the importance of rigorous design, and the challenges faced in bringing new therapies to patients.
The different phases of clinical trials, from initial safety assessments to large-scale efficacy studies, each play a critical role in evaluating potential treatments. We’ll also analyze the diverse trial designs employed, including randomized controlled trials, observational studies, and case-control studies, and discuss their strengths and weaknesses. Understanding these methodologies is essential for interpreting the results and making informed decisions.
Overview of Rheumatoid Arthritis Clinical Trials

Rheumatoid arthritis (RA) is a chronic autoimmune disease that causes inflammation of the joints. Effective treatment strategies and disease management are critical to improving patients’ quality of life. Clinical trials play a vital role in advancing our understanding of RA and developing new and improved therapies.The current landscape of RA clinical trials is characterized by ongoing efforts to identify and test novel therapies targeting different inflammatory pathways.
Researchers are exploring biologics, small molecules, and combination therapies, aiming to achieve better disease control and minimize adverse effects. The focus is also on early intervention and prevention of joint damage, recognizing the importance of early diagnosis and treatment in mitigating long-term complications.
Phases of Clinical Trials in Rheumatoid Arthritis
Clinical trials are typically conducted in phases to evaluate the safety and efficacy of new treatments. Understanding these phases is crucial to grasping the progression of research.Phase I trials are primarily focused on assessing the safety of a new drug or treatment in a small group of healthy volunteers or patients with RA. Researchers monitor for side effects and determine the appropriate dosage range.
For example, in RA, Phase I trials might explore the tolerance and maximum tolerated dose of a novel biologic.Phase II trials involve a slightly larger group of patients with RA to further evaluate the drug’s safety and efficacy. Researchers assess the treatment’s effectiveness in reducing disease activity markers and potential side effects in a controlled environment. A Phase II trial for an RA treatment might examine the drug’s impact on inflammation and joint pain compared to a placebo or standard therapy.Phase III trials are large-scale studies that compare the new treatment to existing standard therapies or a placebo.
These trials provide statistically robust data on the treatment’s effectiveness, safety, and optimal use. A Phase III RA trial might involve thousands of patients across multiple centers, comparing the new drug to a current gold-standard treatment.Phase IV trials occur after a drug is approved for use. These studies investigate the long-term effects and potential rare side effects in a larger population.
A Phase IV RA trial might examine the incidence of specific adverse events over several years of treatment.
Common Methodologies in Rheumatoid Arthritis Clinical Trials
Several methodologies are employed in RA clinical trials to ensure the validity and reliability of results. These methods often include careful patient selection, rigorous data collection, and statistical analysis.Randomized controlled trials (RCTs) are a common method. Patients are randomly assigned to either a treatment group or a control group (placebo or standard therapy). This helps minimize bias and allows researchers to compare the treatment’s effectiveness against the control.
Researchers might use RCTs to evaluate the efficacy of a new disease-modifying antirheumatic drug (DMARD) in reducing joint damage.Observational studies, in contrast to RCTs, do not involve random assignment. Researchers observe patients with RA and their responses to various treatments or risk factors without intervention. This type of study can provide valuable insights into real-world treatment patterns and potential risk factors associated with disease progression.
Researchers might use observational studies to understand the relationship between certain lifestyle factors and RA flares.Case-control studies compare patients with a specific condition (e.g., RA) with a control group that does not have the condition. This helps identify potential risk factors or associations with the disease. Researchers might use case-control studies to investigate genetic predispositions to RA or the role of environmental factors.
Role of Stakeholders in Rheumatoid Arthritis Clinical Trials
Several stakeholders play crucial roles in the success of RA clinical trials.Researchers, including physicians, scientists, and statisticians, design, conduct, and analyze the trials. They ensure ethical conduct, data integrity, and adherence to regulatory guidelines.Patients are essential participants in these trials, providing crucial data and feedback about their experiences. Their informed consent and active participation are critical to the process.Regulatory bodies, such as the Food and Drug Administration (FDA) in the US and equivalent organizations globally, oversee the trials to ensure safety and efficacy standards are met.
They review trial protocols, data, and safety reports before approving a new treatment.
Comparison of Trial Designs
| Trial Design | Description | Strengths | Limitations |
|---|---|---|---|
| Randomized Controlled Trials (RCTs) | Patients randomly assigned to treatment or control groups. | High internal validity, minimizes bias. | Can be expensive and time-consuming, may not always reflect real-world practice. |
| Observational Studies | Researchers observe patients without intervention. | Can study real-world treatment patterns, identify risk factors. | Lower internal validity, potential for confounding variables. |
| Case-Control Studies | Compare patients with a condition to controls without the condition. | Efficient for studying rare diseases, exploring risk factors. | Lower internal validity, can be prone to recall bias. |
Trial Design and Methodology: Rheumatoid Arthritis Clinical Trials
Rigorous trial design is paramount in rheumatoid arthritis (RA) research, ensuring the validity and reliability of findings. A well-structured trial not only evaluates treatment efficacy but also minimizes bias, maximizing the chance of drawing meaningful conclusions about the best approaches to managing this chronic condition. Understanding the methodologies employed in these trials is crucial for interpreting the results and applying them effectively in clinical practice.
Blinding in Rheumatoid Arthritis Clinical Trials
Blinding, or masking, is a critical component of RA trials. It prevents researchers and participants from knowing which treatment a participant is receiving, thereby reducing bias in outcome assessment. This crucial element enhances the objectivity of the study. Several types of blinding exist, each with varying degrees of effectiveness:
- Single-blind: Participants are unaware of the treatment assignment.
- Double-blind: Both participants and researchers assessing the outcomes are unaware of the treatment assignments.
- Triple-blind: Participants, researchers assessing outcomes, and data analysts are unaware of the treatment assignments. This is the highest level of blinding.
The choice of blinding level depends on the specific trial and the potential for bias. Double-blinding, for example, is widely considered the gold standard to reduce bias from both subjective and objective assessments.
Sample Size Calculation in Rheumatoid Arthritis Clinical Trials
Accurate sample size calculation is vital to ensure a trial has sufficient power to detect a meaningful difference between treatments. An insufficient sample size can lead to inconclusive results, while an excessively large sample size wastes resources. Statistical power analysis is essential for determining the appropriate number of participants to enroll.
The calculation considers factors such as the anticipated effect size, the variability in the outcome measures, and the desired level of statistical significance. A smaller effect size, for instance, would require a larger sample size to achieve statistical significance.
Outcome Measures in Rheumatoid Arthritis Clinical Trials
Multiple outcome measures are used to assess treatment effectiveness in RA trials. These measures provide a comprehensive evaluation of the impact of a therapy on various aspects of the disease.
- Disease Activity Measures: These measures quantify the level of inflammation and disease activity, such as the Disease Activity Score (DAS28). This is a common composite score reflecting various aspects of disease severity.
- Physical Function: Assessments of physical function, like the Health Assessment Questionnaire (HAQ), evaluate a patient’s ability to perform daily activities. A lower HAQ score indicates improved function.
- Patient Reported Outcomes: These measures gather data directly from patients regarding their experiences with RA, such as pain levels, fatigue, and quality of life. These provide a patient-centric perspective on treatment effectiveness.
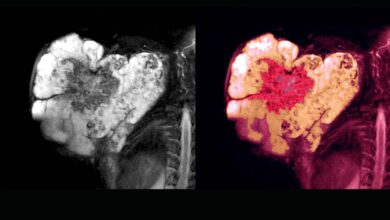
- Radiographic Progression: X-rays or other imaging techniques assess the structural damage caused by the disease. Reduced radiographic progression is a key outcome to consider.
Inclusion and Exclusion Criteria
Clearly defined inclusion and exclusion criteria are necessary for selecting participants who are most likely to benefit from the trial and for ensuring the study’s internal validity.
Rheumatoid arthritis clinical trials are crucial for finding new treatments, but the high cost of healthcare is a major factor to consider. For a deeper dive into why healthcare costs so much, check out this Q&A with a doctor: q a with the doctor who can tell you why healthcare costs an arm and a leg. Understanding these costs helps us better appreciate the challenges faced in developing and accessing effective rheumatoid arthritis treatments.
- Inclusion Criteria: These criteria define the characteristics of participants eligible for the study. Examples might include a specific range of disease activity, duration of RA, and specific demographics. For example, a study targeting a particular drug might include patients who have a specific genetic marker associated with better response.
- Exclusion Criteria: These criteria define the characteristics of participants who are ineligible for the study. This may include pre-existing conditions that could interfere with the results, such as other autoimmune disorders or concomitant medications that could affect the study outcome. An example could be exclusion of patients with active infections or uncontrolled comorbidities.
Data Collection and Management
Rigorous data collection and management procedures are essential for ensuring the accuracy and integrity of trial data. A structured approach, including standardized data forms and electronic data capture systems, minimizes errors.
Recent rheumatoid arthritis clinical trials are exploring various treatment avenues, but maintaining a healthy lifestyle is crucial too. For example, studies show a strong link between diet and overall well-being, and boosting your fertility by giving up fast food could potentially have positive knock-on effects for those managing chronic conditions like rheumatoid arthritis. Ultimately, these trials are vital for finding the best possible solutions for individuals facing this condition.
- Data Management System: A robust electronic data capture system is crucial for managing large volumes of data and ensuring data quality, allowing for rapid and efficient analysis.
- Data Validation: Regular validation procedures, including data cleaning and error correction, ensures the accuracy and completeness of the data collected.
Potential Sources of Bias and Mitigation Strategies
| Potential Source of Bias | Mitigation Strategy |
|---|---|
| Selection Bias (Participants not representative of the population) | Carefully designed inclusion and exclusion criteria, randomisation procedures, and appropriate sample size calculation. |
| Performance Bias (Differences in care between treatment groups) | Standardized care protocols, blinding of healthcare providers, and frequent monitoring. |
| Detection Bias (Differences in outcome assessment) | Blinding of outcome assessors, standardized assessment tools, and multiple assessment points. |
| Attrition Bias (Participants dropping out of the study) | Strategies to maintain participant adherence, including careful patient monitoring, communication, and incentives. |
| Reporting Bias (Selective reporting of results) | Pre-specification of outcome measures, complete reporting of all outcomes, and transparent data sharing. |
Emerging Trends and Future Directions
The landscape of rheumatoid arthritis (RA) clinical trials is constantly evolving, driven by breakthroughs in understanding the disease’s complexities and innovative therapeutic approaches. This dynamic environment presents both exciting opportunities and significant challenges for researchers and patients. Emerging trends are pushing the boundaries of treatment effectiveness and patient experience, promising a brighter future for those living with RA.The future of RA clinical trials hinges on a multifaceted approach, integrating advancements in diagnostics, therapeutics, and trial design.
These changes aim to personalize treatment, improve outcomes, and reduce the time and resources required for successful trials.
Emerging Therapeutic Approaches
Significant advancements in understanding RA pathogenesis have spurred the development of novel therapeutic targets. These include biologics targeting specific inflammatory pathways, and the exploration of immunomodulatory agents that can effectively dampen the overactive immune response characteristic of RA. Researchers are actively investigating targeted therapies that can potentially minimize side effects and maximize efficacy. These innovative approaches are transforming how RA is managed, potentially leading to more personalized and effective treatments.
Promising Areas of Research and Development
Several promising areas of research are shaping the future of RA clinical trials. One key area is the development of disease-modifying antirheumatic drugs (DMARDs) with enhanced efficacy and reduced side effects. Another promising avenue is the exploration of precision medicine strategies tailored to individual patient characteristics, aiming for more targeted and effective treatments. This includes the identification of biomarkers to predict treatment response, enabling earlier intervention and optimization of therapy.
Finally, the investigation of combination therapies is being explored to achieve synergistic effects, potentially offering improved outcomes.
Innovative Trial Designs
Innovative trial designs are being implemented to address challenges in RA clinical trials. Adaptive designs, which allow for adjustments in the trial protocol based on accumulating data, are gaining popularity. This flexibility allows for quicker identification of effective therapies and more efficient use of resources. Another approach involves the use of patient-reported outcomes (PROs) alongside traditional clinical measures.
Rheumatoid arthritis clinical trials are pushing the boundaries of what’s possible, and the potential for breakthroughs is huge. Innovative approaches, like those explored in the field of regenerative medicine, hold incredible promise for future treatments. Regenerative medicine has bright future offers exciting possibilities for repairing damaged tissues and restoring function, which could revolutionize the outcomes for patients in rheumatoid arthritis clinical trials.
Researchers are actively investigating these novel approaches to tackle the disease’s debilitating effects.
PROs provide valuable insights into the patient experience, capturing aspects of quality of life and disease impact that are not always reflected in objective measures.
Role of Technology in Streamlining Trials
Technology is playing an increasingly crucial role in streamlining RA clinical trials. Electronic data capture systems, for example, improve data accuracy and reduce manual errors. Remote monitoring technologies allow for more convenient and efficient collection of patient data, enabling longitudinal observation and potentially leading to quicker recruitment and follow-up. Furthermore, the use of artificial intelligence (AI) is being explored to analyze large datasets and identify patterns that might lead to better treatment strategies.
Potential Challenges Facing Future Trials
Despite the exciting advancements, several challenges could hinder progress in RA clinical trials. One key challenge is the recruitment of diverse patient populations to ensure the generalizability of findings. Another challenge is the need for standardized outcome measures across different trials to facilitate comparison and meta-analysis. Additionally, ensuring patient adherence to treatment protocols and managing potential side effects remain crucial considerations.
Comparison of Traditional and Novel Approaches
| Feature | Traditional Approaches | Novel Approaches |
|---|---|---|
| Mechanism of Action | Generally targeting inflammation with broad-spectrum DMARDs | Targeting specific inflammatory pathways or immune mechanisms |
| Specificity | Less specific; potential for side effects | More targeted; potentially fewer side effects |
| Trial Design | Often fixed designs, less adaptable to emerging data | Adaptive designs, utilizing real-time data analysis |
| Patient Outcomes | Variable, sometimes limited improvements | Potential for more effective and personalized outcomes |
| Examples | Methotrexate, corticosteroids | Biologics (e.g., TNF inhibitors), targeted therapies |
Ethical Considerations in Clinical Trials
Clinical trials for rheumatoid arthritis, like any medical research involving human subjects, demand stringent ethical considerations. These trials aim to improve patient outcomes and advance medical knowledge, but must always prioritize the well-being and rights of participants. Maintaining ethical standards ensures the integrity of the research and public trust in the medical field.Ethical principles are the bedrock upon which trustworthy and responsible clinical trials are built.
They ensure that the rights and welfare of participants are protected, and that research is conducted in a manner that is aligned with societal values and expectations. Ethical oversight is crucial in all phases of a clinical trial, from initial design to data analysis and dissemination of findings.
Informed Consent
Informed consent is paramount in clinical trials. Participants must fully understand the nature of the study, potential risks and benefits, and their rights. This involves providing detailed information about the trial procedures, potential side effects, alternative treatment options, and the right to withdraw at any time without penalty. A clear and understandable explanation of the trial protocol, in a language the participant comprehends, is essential for truly informed consent.
The consent form must be properly documented, signed, and witnessed to ensure the participant’s voluntary agreement.
Ethical Approval Process
Ethical approval for clinical trials is a multi-step process that involves a rigorous review of the trial protocol by an independent Institutional Review Board (IRB) or Ethics Committee. This review ensures that the trial adheres to ethical guidelines and protects the rights and safety of participants. The IRB assesses the study design, data collection methods, risk-benefit assessment, informed consent procedures, and the overall conduct of the trial.
This thorough review process safeguards against potential harm and ensures the trial aligns with established ethical standards.
Ethical Guidelines and Regulations
Numerous ethical guidelines and regulations govern clinical trials, aiming to protect human subjects. These regulations often come from national and international bodies like the World Medical Association and various national regulatory agencies. They Artikel principles like respect for persons, beneficence, and justice. These guidelines ensure the trials are conducted in a manner that prioritizes the well-being and autonomy of participants.
- Respect for Persons: Recognizing the autonomy of individuals and protecting vulnerable populations. This necessitates tailored consent processes for individuals with cognitive impairments or limited capacity to understand the trial.
- Beneficence: Minimizing risks and maximizing potential benefits for participants. The study must demonstrate a reasonable expectation of benefit, outweighing potential harms.
- Non-maleficence: Avoiding or minimizing harm to participants. This requires rigorous assessment of potential risks and the implementation of safety measures.
- Justice: Ensuring equitable selection of participants and fair distribution of benefits and burdens. This principle addresses issues of potential bias in participant recruitment and ensures that the trial is not exploitative.
Patient Safety in Clinical Trials
Patient safety is paramount in rheumatoid arthritis clinical trials. Careful monitoring of participants throughout the trial is essential to identify and address any adverse events promptly. Procedures must be in place for reporting and managing adverse events, and participants should have access to appropriate medical care. This includes close monitoring for side effects of the treatment and careful evaluation of the potential risks associated with the experimental intervention.
Beneficence and Non-maleficence
The principles of beneficence and non-maleficence are central to clinical trials. Beneficence mandates a commitment to maximizing benefits and minimizing risks to participants. Non-maleficence stresses the imperative to avoid causing harm. The trial design and conduct must carefully balance these principles, aiming to produce meaningful improvements in the lives of participants while minimizing potential adverse effects. The IRB plays a critical role in assessing the risk-benefit ratio of the trial to ensure the safety of participants.
Key Ethical Considerations in Different Phases of Clinical Trials
| Trial Phase | Key Ethical Considerations |
|---|---|
| Phase 1 | Focus on safety, dosage optimization, and preliminary efficacy. Rigorous monitoring of side effects is crucial. |
| Phase 2 | Evaluation of efficacy and further assessment of safety. Informed consent must be continuously reviewed and updated as needed. |
| Phase 3 | Large-scale testing of efficacy and safety. Recruitment of diverse populations is essential to ensure generalizability of results. |
| Phase 4 | Post-market surveillance of long-term effects and benefits of the treatment. Monitoring for rare or delayed adverse events is paramount. |
Data Analysis and Interpretation
Unraveling the complexities of rheumatoid arthritis clinical trials requires meticulous data analysis and interpretation. This crucial step transforms raw trial data into actionable insights, helping researchers understand treatment efficacy, safety, and potential long-term effects. Accurate interpretation is vital for informing clinical practice and shaping future research directions.
Common Statistical Methods
Statistical methods are essential tools in analyzing data from rheumatoid arthritis clinical trials. They allow researchers to quantify the impact of interventions and determine if observed differences are likely due to chance or genuine effects. Commonly used methods include:
- Descriptive statistics: These methods summarize and describe the characteristics of the study population, such as age, gender, disease severity, and baseline characteristics. They provide a snapshot of the trial participants and help in understanding the representativeness of the sample. For example, a researcher might calculate the mean age and standard deviation of the participants in the treatment and control groups.
- Inferential statistics: These methods allow researchers to make inferences about a larger population based on the sample data. They help determine if observed differences between treatment groups are statistically significant. Common tests include t-tests, analysis of variance (ANOVA), and regression analysis. For instance, a t-test can compare the mean disease activity scores between the treatment and control groups.
- Survival analysis: This method is particularly useful in assessing the time until a specific event occurs, such as disease remission or the need for joint replacement surgery. It considers factors like the duration of treatment and the risk of events over time. Survival analysis is crucial in evaluating the long-term impact of rheumatoid arthritis treatments.
Interpreting Trial Results
Interpreting results requires careful consideration of both statistical significance and clinical significance. Statistical significance indicates that the observed difference is unlikely to have occurred by chance. Clinical significance, however, assesses whether the difference is meaningful in the context of real-world patient care.
- Statistical Significance vs. Clinical Significance: A statistically significant result might show a small difference in disease activity between treatment groups. However, this difference might not be clinically relevant if the magnitude of the effect is too small to translate into meaningful improvements in patients’ quality of life. A good example is a treatment showing a statistically significant reduction in inflammation, but the reduction is so small it doesn’t result in a noticeable improvement in pain or function.
Communicating Trial Results
Disseminating trial results to the medical community and the public is a critical step in the research process. This often involves publishing findings in peer-reviewed journals and presenting them at medical conferences. Transparent communication ensures that the information is accessible and understood by healthcare professionals and patients.
- Transparency and Dissemination: Researchers should be transparent about all aspects of the trial, including study design, data analysis methods, and potential limitations. This ensures that the results are interpreted accurately and that the conclusions are supported by the data. Trial results are often presented in presentations at medical conferences, enabling discussions and fostering further research.
Example: Statistical vs. Clinical Significance
A rheumatoid arthritis trial might find a statistically significant reduction in disease activity with a new drug compared to a placebo. However, the reduction might be so small that it doesn’t translate into a noticeable improvement in patients’ daily lives. This highlights the importance of considering both statistical and clinical significance when interpreting trial results. For example, a 10% reduction in disease activity might be statistically significant but not clinically meaningful if the baseline disease activity was already very low.
Key Steps in Interpreting Trial Results
| Step | Description |
|---|---|
| 1. Data Cleaning and Preparation | Ensuring data accuracy and consistency |
| 2. Descriptive Statistics | Summarizing and visualizing the data |
| 3. Statistical Analysis | Applying appropriate statistical methods to test hypotheses |
| 4. Interpretation of Results | Considering both statistical and clinical significance |
| 5. Reporting and Dissemination | Communicating findings to the medical community and public |
Case Studies and Examples

Diving into the world of rheumatoid arthritis clinical trials reveals a fascinating interplay of scientific rigor, patient resilience, and ultimately, progress in treatment. These trials aren’t just about numbers and data; they represent the journeys of individuals seeking relief and the collective pursuit of a better future for those affected by this chronic condition. Let’s explore some compelling case studies and examples that showcase the impact of clinical trials on our understanding and management of rheumatoid arthritis.
A Successful Clinical Trial: The Impact of Tofacitinib
The development and approval of tofacitinib, a Janus kinase (JAK) inhibitor, marked a significant advancement in the treatment of rheumatoid arthritis. This oral medication demonstrated impressive efficacy in clinical trials, reducing inflammation and improving patient outcomes compared to traditional disease-modifying antirheumatic drugs (DMARDs). One particular trial, for example, showed a statistically significant reduction in disease activity scores (DAS28) in patients treated with tofacitinib, leading to improved physical function and quality of life.
This success story highlights the potential of targeted therapies in effectively managing rheumatoid arthritis, moving beyond the limitations of older treatments.
Efficacy of Specific Treatments in Clinical Trials
Numerous clinical trials have confirmed the efficacy of various treatments for rheumatoid arthritis. Methotrexate, a cornerstone of DMARD therapy, has consistently demonstrated its ability to slow disease progression and reduce symptoms. Other biological DMARDs, like tumor necrosis factor (TNF) inhibitors, have proven highly effective in suppressing inflammation and preventing joint damage in many clinical trials. These successes underscore the importance of diverse treatment options, catering to the unique needs and responses of individual patients.
Impact of Clinical Trials on Understanding and Treatment
Clinical trials have significantly reshaped our understanding of rheumatoid arthritis and its treatment. Early trials revealed the crucial role of early intervention and aggressive treatment strategies in preventing joint damage. Subsequent studies have further refined our understanding of disease mechanisms and identified specific biomarkers for disease activity. This has led to the development of targeted therapies that precisely address the underlying causes of the disease.
Importantly, clinical trials have emphasized the need for personalized medicine approaches, tailoring treatments to the individual characteristics of each patient.
Challenges and Strategies in Conducting a Clinical Trial
Conducting a rheumatoid arthritis clinical trial presents several challenges. Recruiting a diverse and representative patient population is often difficult, particularly for trials evaluating the efficacy of newer or more specialized treatments. Maintaining the integrity of the study design, controlling for confounding variables, and ensuring compliance with rigorous ethical standards are also critical. Researchers employ various strategies to overcome these hurdles, such as using standardized assessment tools, establishing clear inclusion/exclusion criteria, and actively engaging patient advocacy groups.
A Failed Clinical Trial: The Limitations of a Novel Antibody Therapy
One failed clinical trial focused on a novel antibody therapy, which aimed to neutralize a specific inflammatory cytokine believed to be a key driver of rheumatoid arthritis. The trial failed to demonstrate a statistically significant improvement in disease activity compared to placebo. The reasons for failure could be varied, including a lack of sufficient potency of the antibody, insufficient targeting of the inflammatory cytokine, or an inadequate understanding of the complex interplay of factors involved in rheumatoid arthritis.
This example underscores the importance of rigorous preclinical testing and a thorough understanding of the disease before embarking on a clinical trial.
Illustrative Examples of Progression and Treatment Efficacy
Visual representations, like graphs and charts, can effectively illustrate the progression of rheumatoid arthritis symptoms and the impact of treatment efficacy. For instance, a graph showing the decline in joint pain and swelling over time for patients treated with a specific DMARD could visually demonstrate the positive effects of therapy. Furthermore, longitudinal data from clinical trials, presenting the evolution of disease activity scores (DAS28), can provide concrete evidence of treatment effectiveness.
These illustrations are crucial in communicating complex clinical trial data to both researchers and patients in a clear and accessible manner.
Summary
In conclusion, rheumatoid arthritis clinical trials represent a multifaceted journey from initial research to the potential development of life-altering therapies. From the meticulous design and execution of trials to the ethical considerations and data interpretation, every aspect is vital in ensuring patient safety and advancing medical knowledge. The future of rheumatoid arthritis treatment hinges on continued innovation in clinical trial design, and on the ongoing collaboration between researchers, patients, and regulatory bodies.