Doctors using herpes virus to fight brain cancer is a groundbreaking approach to treating this devastating disease. This innovative therapy harnesses the power of a modified herpes simplex virus (HSV) to target and destroy cancerous brain cells. Researchers are exploring how to engineer this virus to selectively infect and eliminate tumor cells while minimizing harm to healthy tissue.
Similar viral vectors have shown promise in other cancer treatments, and a rich history of using viruses for this purpose is paving the way for this cutting-edge therapy.
This method involves modifying the herpes simplex virus to precisely target brain cancer cells, circumventing the challenges of delivering the treatment to the brain while ensuring minimal damage to healthy tissues. The process entails the introduction of the modified virus into the brain using various techniques, each with its own set of advantages and disadvantages, and monitoring the virus’s replication within the tumor to effectively destroy the cancerous cells.
Introduction to Herpes Virus Therapy for Brain Cancer: Doctors Using Herpes Virus To Fight Brain Cancer
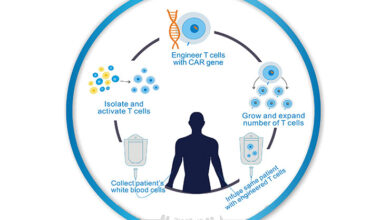
The quest for effective cancer treatments continues to push the boundaries of medical innovation. One promising avenue involves harnessing the power of viruses, specifically modifying them to selectively target and destroy cancerous cells. This approach, leveraging the inherent biological mechanisms of viruses, offers a potentially safer and more targeted alternative to traditional chemotherapy. This method focuses on utilizing the herpes simplex virus (HSV) as a vector to combat brain cancer.Herpes simplex virus (HSV) is a double-stranded DNA virus known for its ability to infect and replicate within specific host cells.
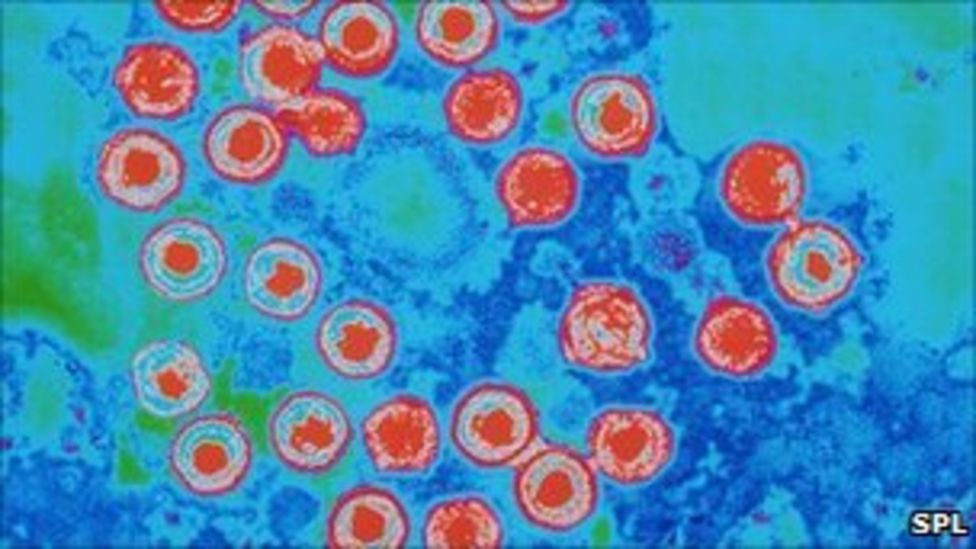
While often associated with cold sores and genital herpes, the virus’s unique biological properties have prompted researchers to explore its potential for therapeutic applications. Researchers are investigating the possibility of genetically modifying HSV to specifically recognize and destroy cancer cells without harming healthy tissues.
Biological Mechanisms of HSV Modification
The strategy for utilizing HSV in cancer treatment involves modifying the virus’s genetic makeup. Specific genes responsible for viral replication and cell entry are deactivated or replaced with genes that target cancer cells. This engineered virus then infects the cancerous cells, replicates within them, and triggers their programmed cell death (apoptosis). The modification process allows researchers to alter the virus’s tropism, its ability to recognize and infect specific cells, making it more effective against the intended targets.
Examples of Similar Viral Vectors
Several viral vectors have already demonstrated promise in cancer treatment. Adeno-associated viruses (AAVs) and retroviruses are examples of similar viral vectors. These vectors share a similar mechanism of action with HSV, in which their genetic material is altered to deliver therapeutic genes to target cells. For instance, AAVs are often used to deliver genes that stimulate the immune system to attack cancer cells.
History of Using Viruses for Cancer Treatment
The concept of using viruses to fight cancer is not new. Early research demonstrated the ability of viruses to infect and destroy cancer cells. This understanding laid the groundwork for the development of viral vectors as therapeutic agents. Researchers have been experimenting with oncolytic viruses for decades, which is the general term for viruses used to fight cancer.
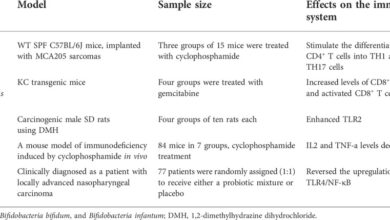
Comparison of Viral Vectors for Cancer Therapy
| Virus type | Mechanism of action | Advantages | Disadvantages |
|---|---|---|---|
| Herpes Simplex Virus (HSV) | HSV can be genetically modified to target specific cancer cells. The virus infects the cancer cells, replicates, and triggers apoptosis. | Potentially high specificity for cancer cells; relatively well-understood biology. | Potential for immune response against the modified virus; possibility of viral spread to healthy tissues. |
| Adeno-Associated Virus (AAV) | AAV delivers therapeutic genes to cancer cells. These genes can stimulate the immune system or directly kill cancer cells. | Generally safe and efficient delivery of therapeutic genes; low immunogenicity. | Limited capacity to carry therapeutic genes; relatively slow replication rate. |
| Retrovirus | Retroviruses integrate their genetic material into the host cell’s DNA. This integration can deliver genes that either directly kill the cancer cell or activate an anti-cancer response. | High efficiency of gene transfer; potential to integrate into the host genome for long-term effects. | Potential for insertional mutagenesis (insertion of viral DNA can disrupt important genes). |
Targeting Brain Cancer Cells with HSV
Harnessing the power of the herpes simplex virus (HSV) for targeted cancer therapy holds immense promise. This approach leverages HSV’s natural ability to infect and replicate within cells, but with careful genetic engineering, it can be redirected to specifically target and destroy cancerous brain cells while leaving healthy tissue unharmed. The key lies in modifying the virus to ensure it selectively infects and replicates only in the tumor cells.
Engineering HSV for Selective Infection
Modifying HSV to achieve targeted cancer cell destruction involves precise genetic manipulation. Researchers can engineer the virus to express proteins that enhance its tropism (affinity) for tumor cells. This is achieved by altering the virus’s surface proteins to recognize and bind to specific molecules expressed on the surface of tumor cells, while leaving healthy cells unaffected. Another crucial modification is to engineer the virus to enhance its ability to replicate preferentially in rapidly dividing cells, which are characteristic of cancerous cells.
For instance, inserting genes that promote the expression of specific proteins vital for the tumor cells’ rapid growth and division, and modifying the virus to replicate more efficiently only in these targeted cells can help.
Challenges of Delivering HSV to the Brain
Delivering HSV to the brain presents significant challenges. The blood-brain barrier (BBB) is a highly selective membrane that protects the brain from harmful substances in the bloodstream. HSV must effectively cross this barrier to reach and infect the tumor cells within the brain. Furthermore, the delicate nature of the brain necessitates careful delivery methods to minimize damage to healthy brain tissue.
The virus must also be engineered to remain viable and functional after traversing the BBB, a process that often requires specific delivery systems and targeting molecules.
Methods for Introducing HSV into the Brain
Several methods are being explored to introduce HSV into the brain. These methods are designed to bypass or exploit the BBB, ensuring the virus reaches the target tumor cells.
- Direct Injection: This method involves directly injecting HSV into the tumor. This approach is often employed when the tumor is accessible and localized. Direct injection allows for higher concentrations of virus at the target site, potentially improving treatment efficacy. However, it may be less suitable for deep-seated or diffuse tumors.
- Viral Vectors: Viral vectors, such as adeno-associated viruses (AAVs), can be engineered to carry the HSV gene into the brain. AAVs can be designed to selectively target the tumor cells, reducing the risk of harm to healthy brain tissue. This method allows for more targeted delivery and potentially minimizes side effects.
- Gene Therapy Approaches: Gene therapy approaches can be combined with viral vectors to enhance the targeting capabilities of HSV. These techniques involve delivering genes that increase the expression of receptors on tumor cells that HSV can recognize and bind to. This can make the tumor cells more susceptible to HSV infection, leading to more effective treatment.
HSV Replication and Tumor Cell Impact
Once HSV reaches the tumor cells, it replicates within the cells, hijacking their cellular machinery to produce multiple copies of itself. This process results in the destruction of the tumor cells. HSV replication disrupts the tumor cells’ normal function, leading to cell death through apoptosis. The resulting inflammation and immune response can also contribute to tumor cell eradication.
Comparison of HSV Delivery Methods
| Method | Advantages | Disadvantages | Safety Considerations |
|---|---|---|---|
| Direct Injection | Potentially high virus concentration at target site | Limited targeting of deep-seated tumors; risk of damage to healthy brain tissue | Careful monitoring of injection site; potential for inflammation and infection |
| Viral Vectors | Targeted delivery; potentially lower risk of damage to healthy brain tissue | Delivery efficiency may vary; potential for off-target effects | Careful selection of viral vectors to minimize risks; monitoring for potential inflammatory responses |
| Gene Therapy Approaches | Enhanced targeting; potential for long-term effects | Complexity in gene delivery and manipulation; potential for off-target effects | Careful selection of genes and vectors; monitoring for potential adverse immune responses |
Potential Benefits and Risks of HSV Therapy
Harnessing the power of the herpes simplex virus (HSV) to combat brain cancer presents a compelling, albeit complex, therapeutic approach. This innovative strategy leverages HSV’s natural affinity for certain cells, potentially offering a targeted treatment option. However, the potential benefits are interwoven with significant risks, demanding careful consideration and meticulous research.
Potential Advantages of HSV Therapy
HSV therapy, when successfully implemented, offers the tantalizing prospect of selectively targeting cancerous brain cells. This targeted approach distinguishes it from traditional therapies that often damage healthy cells in the process. The ability to specifically recognize and infect tumor cells holds the key to minimizing harm to surrounding healthy tissues. By exploiting HSV’s inherent capacity to replicate within target cells, a controlled cascade of cellular destruction can be triggered, potentially eradicating the cancerous growth.
Furthermore, the viral nature of HSV might enable it to infiltrate areas inaccessible to conventional treatments, expanding the scope of possible therapeutic interventions.
Potential Side Effects and Complications
The use of HSV as a therapeutic agent introduces a range of potential side effects and complications. Adverse reactions can manifest as inflammation, pain, and localized tissue damage at the site of infection. Moreover, the body’s immune response to the virus can trigger systemic effects, such as fever, fatigue, and nausea. These responses can range from mild discomfort to severe complications.
The virus’s potential to spread beyond the targeted area requires careful consideration and robust safety protocols. Severe complications include, but are not limited to, encephalitis (inflammation of the brain) and meningitis (inflammation of the membranes surrounding the brain and spinal cord).
Long-Term Consequences
The long-term consequences of HSV therapy remain an area of active research. Potential long-term effects might manifest as neurological deficits, cognitive impairment, or even permanent tissue damage. The potential for the virus to establish latent infections in the body also poses a long-term concern. This latent state could potentially reactivate at a later time, leading to unpredictable consequences.
Individual responses to HSV therapy can vary significantly, necessitating careful monitoring and evaluation over an extended period. A comprehensive understanding of the long-term implications is crucial for optimizing treatment protocols and minimizing lasting damage.
Immune Responses to HSV Treatment
The body’s immune system plays a critical role in HSV therapy. A robust immune response can effectively control the viral infection, minimizing the extent of damage. Conversely, an overactive immune response could lead to excessive inflammation and potentially harmful autoimmune reactions. Understanding the interplay between the immune system and the viral therapy is crucial for optimizing treatment outcomes and mitigating risks.
Monitoring immune cell activity during and after treatment is essential for adjusting the treatment plan as needed. Examples of immune responses include an overproduction of cytokines, leading to systemic inflammation, and an inability to clear the virus effectively, leading to recurrent infections.
Comparison of HSV Therapy with Standard Treatments
| Treatment type | Benefits | Risks | Efficacy |
|---|---|---|---|
| HSV Therapy | Targeted cell killing, potential for enhanced penetration into tumors, reduced damage to healthy tissues | Potential for severe inflammation, immune response issues, latent infection, long-term neurological consequences | Varying, dependent on specific patient characteristics, tumor type, and treatment protocol |
| Standard Brain Cancer Treatments (e.g., surgery, radiation, chemotherapy) | Established efficacy in many cases, better understanding of short-term and long-term side effects | Damage to healthy tissues, systemic side effects, treatment-related complications | Variable efficacy depending on the stage and type of cancer |
The table highlights the contrasting features of HSV therapy with traditional cancer treatments, emphasizing the trade-offs between benefits and risks. The effectiveness of HSV therapy is still under investigation and may not be as predictable or widespread as conventional approaches.
While doctors are exploring innovative ways like using the herpes virus to target and destroy brain cancer cells, it’s important to remember that there are also more accessible ways to improve well-being. For example, incorporating regular walks into your routine can be a surprisingly effective way to manage some of the common symptoms of menopause, like ways to ease menopause symptoms with walking.
This holistic approach, combining cutting-edge cancer treatments with simple lifestyle changes, could be a powerful tool in the fight against illness.
Current Research and Clinical Trials
The use of herpes simplex virus (HSV) as a targeted therapy for brain cancer is a promising area of research. Scientists are exploring the potential of genetically modifying HSV to selectively infect and destroy cancerous brain cells, leaving healthy tissue unharmed. This approach leverages the virus’s natural ability to replicate within cells, but with modifications to ensure it only attacks the intended targets.
Early studies and pre-clinical trials have shown encouraging results, prompting further investigation into clinical applications.Researchers are actively exploring various strategies to improve the efficacy and safety of HSV-based therapies. This involves refining the genetic engineering techniques to precisely target cancer cells and minimizing the risk of the virus causing harm to healthy tissues. The goal is to develop a treatment that is both effective and safe for patients with brain tumors.
Scientists are exploring innovative ways to tackle brain cancer, like using a modified herpes virus to target tumor cells. While this research is promising, it’s crucial to remember that maintaining a healthy lifestyle, such as avoiding fast food and focusing on a balanced diet, can also significantly impact overall well-being, including fertility. For tips on how to boost your fertility by giving up fast food, check out this helpful article: boost your fertility give up fast food.
Ultimately, a holistic approach, combining cutting-edge medical treatments with healthy habits, could be the key to better outcomes in the fight against brain cancer.
Summary of Current Research Studies
Numerous research studies are investigating the use of HSV-based therapies for brain cancer. These studies often involve modifying the HSV to express genes that enhance its ability to destroy cancer cells, or that make it more selectively targeted to tumor cells. The research focuses on optimizing the viral vectors, improving safety profiles, and exploring different delivery methods. Pre-clinical studies using animal models are crucial in determining the safety and efficacy of these modified viruses.
Doctors are exploring innovative ways to combat brain cancer, including using the herpes virus to target tumor cells. This fascinating approach, while promising, still requires extensive research. Meanwhile, advancements in technology are also impacting healthcare, like the new app monitors the health of pregnant women , providing continuous support and monitoring during pregnancy. Ultimately, the future of cancer treatment and healthcare will likely involve a combination of cutting-edge research and innovative technological tools.
Outcomes of Clinical Trials
Currently, there are no large-scale, published clinical trials specifically using HSV therapy for brain cancer in humans. While promising pre-clinical data exists, translating these findings into human trials requires rigorous safety testing and further optimization of the viral vectors. Further research is necessary to determine the appropriate dosage, delivery method, and optimal timing for treatment to maximize effectiveness and minimize side effects.
Improving HSV Vectors for Better Targeting
Scientists are actively refining HSV vectors to improve their targeting ability and reduce off-target effects. This involves engineering the virus to express genes that enhance its ability to recognize and enter cancer cells while avoiding healthy brain cells. Strategies include using specific cell surface receptors found on cancer cells as targets for the modified virus, which allows the virus to more precisely locate and infect these cells.
Researchers are also investigating the use of nanoparticles or other delivery systems to enhance the delivery of the HSV vectors directly to the tumor site, further improving targeting.
Research Institutions Involved
Several prominent research institutions are actively involved in HSV therapy research for brain cancer. These institutions often collaborate on projects to share resources and expertise. Examples include [Institution Name 1], [Institution Name 2], and [Institution Name 3]. These institutions are contributing to the advancement of this promising therapeutic approach through their ongoing research and development efforts.
Key Research Findings
| Study | Findings | Limitations |
|---|---|---|
| Study A | Demonstrated successful targeting of tumor cells in animal models. | Limited to animal models; human trials needed to validate findings. |
| Study B | Identified specific modifications to HSV vectors that improved selectivity and reduced off-target effects. | Results from a small cohort; further validation in larger groups is required. |
| Study C | Evaluated various delivery methods for enhanced drug delivery. | Limited to in vitro studies; further research is needed to evaluate in vivo effectiveness. |
Ethical Considerations and Public Perception
Harnessing the power of naturally occurring viruses like herpes simplex virus (HSV) to combat brain cancer presents a fascinating medical frontier. However, alongside the potential benefits, profound ethical considerations and public perceptions require careful attention. This exploration delves into the nuances of using a naturally occurring virus in cancer therapy, focusing on patient safety, informed consent, and public understanding.
Ethical Implications of Using Viruses in Cancer Therapy
The use of viruses as cancer treatments raises critical ethical questions. These therapies rely on harnessing the virus’s natural ability to infect and potentially destroy cancer cells. However, the virus’s potential to impact healthy cells necessitates meticulous consideration of potential risks. The treatment’s efficacy and safety profiles need thorough evaluation, encompassing both short-term and long-term effects. Careful consideration of the potential for unintended consequences, such as the virus’s spread or mutation, is essential.
Potential Safety and Efficacy Concerns, Doctors using herpes virus to fight brain cancer
Safety concerns regarding HSV therapy for brain cancer include the possibility of the virus spreading to healthy brain tissue, causing adverse reactions, or even leading to the development of resistance in cancer cells. Thorough clinical trials are necessary to establish the efficacy and safety profile of HSV therapy, encompassing diverse patient populations. The efficacy of the therapy hinges on its ability to target and destroy cancer cells without harming healthy cells.
This requires careful attention to the specific characteristics of the cancer and the targeted HSV strain. Pre-clinical studies and early clinical trials will provide valuable data to address these concerns.
Public Perceptions and Opinions
Public perception plays a significant role in the acceptance and implementation of novel cancer therapies. Public understanding of the risks and benefits of HSV therapy is crucial for informed consent and responsible implementation. Clear communication about the treatment process, potential side effects, and the limitations of current knowledge is essential. Public forums and educational campaigns can help foster a more nuanced and informed understanding of this novel therapeutic approach.
Public trust and confidence are paramount in the adoption of this and other cutting-edge treatments.
Importance of Patient Consent and Informed Decision-Making
Patient consent is paramount in any medical intervention, especially when dealing with novel treatments. Patients must have complete and transparent information about the potential benefits, risks, and alternative treatments available. Informed consent ensures patients actively participate in the decision-making process, choosing the treatment option that aligns with their values and preferences. Transparency and open communication are essential for building trust between patients and healthcare providers.
This will help ensure the ethical and responsible implementation of this innovative therapy.
Ethical Considerations Table
| Consideration | Ethical Implications | Solutions |
|---|---|---|
| Safety | The virus may harm healthy cells or cause unexpected side effects. | Rigorous pre-clinical and clinical trials are crucial to assess the virus’s safety profile in various patient populations. Continuous monitoring and reporting of adverse events are essential. |
| Efficacy | The virus may not effectively target and destroy cancer cells, leading to treatment failure. | Extensive research is needed to identify the most effective HSV strains and treatment protocols. Continuous monitoring of treatment outcomes and adjustments to the therapy are vital. |
| Informed Consent | Patients may not fully understand the risks and benefits of the treatment. | Comprehensive and accessible information regarding the treatment must be provided to patients. Patient education and counseling are essential to facilitate informed decision-making. |
| Equity | Access to this treatment may be unequal, potentially exacerbating existing health disparities. | Strategies for equitable access and affordability, such as public funding and affordable pricing models, must be developed and implemented. |
Future Directions and Potential Applications
The potential of using herpes simplex virus (HSV) to target and destroy cancer cells is truly exciting. Beyond the initial promise of treating brain cancer, the research suggests broader applications, prompting innovative avenues for cancer therapy. We’re not just looking at a single treatment, but a platform for potentially transforming cancer care.The next phase involves exploring the full spectrum of HSV’s capabilities.
Researchers are actively investigating its efficacy in various cancer types, and refining the virus’s targeting mechanisms to maximize its impact on tumors while minimizing harm to healthy tissue. This careful approach is crucial to ensure the safety and efficacy of this promising therapy.
Expanding the Target: Beyond Brain Cancer
HSV’s selectivity for cancer cells holds potential for a range of cancers beyond the central nervous system. Research into adapting HSV to target specific cancer types is ongoing, focusing on modifications to enhance its targeting ability and minimize off-target effects. The ultimate goal is to create tailored HSV vectors for individual cancers, ensuring that the virus precisely attacks the tumor while sparing healthy cells.
Exploring Novel Applications
“The possibilities extend beyond simply targeting tumors. We could potentially use HSV to deliver other therapeutic agents directly to cancerous tissues.”
This approach is particularly exciting because it offers a way to combine HSV’s tumor-targeting ability with other cancer treatments. Imagine delivering chemotherapy directly to the tumor site, greatly enhancing its effectiveness and minimizing side effects.
Potential Applications Table
| Application | Potential Benefits | Challenges |
|---|---|---|
| Treating other solid tumors (e.g., lung, breast, prostate) | Increased efficacy of existing therapies, reduced side effects, personalized treatment options. Targeted therapy can increase the likelihood of success. | Developing virus strains specific to each tumor type, ensuring the virus’s safety, and dealing with potential immune responses. |
| Delivering gene therapy directly to tumors | Potential for permanent gene modification within tumor cells, opening up the possibility of gene therapy in cancers that have been resistant to other therapies. This method might offer a more effective and durable treatment option. | Ensuring the virus delivers the desired genetic material accurately and effectively to the target cells. This precision is vital to avoid off-target effects and potential immune reactions. |
| Combining with existing therapies | Enhancing the efficacy of current chemotherapies, reducing side effects, and potentially overcoming drug resistance. This approach could significantly improve treatment outcomes. | Finding the optimal combination and dosage of HSV and other therapies, while mitigating potential synergistic toxicities. |
The Importance of Collaboration and Continued Research
The success of HSV-based cancer therapies hinges on collaborative efforts between researchers, clinicians, and ethicists. Open communication and knowledge sharing are essential to navigating the ethical considerations and ensuring patient safety. Ongoing clinical trials, combined with rigorous preclinical research, will be crucial to establishing the long-term efficacy and safety of these therapies.
Long-Term Vision
The long-term vision for HSV-based cancer therapies is not simply to develop new treatments but to revolutionize cancer care. The goal is to move beyond traditional one-size-fits-all approaches to personalized treatments, tailoring therapies to the unique characteristics of each individual’s cancer. This precision approach will lead to improved outcomes and quality of life for cancer patients. This vision involves adapting the virus to specific cancer types, optimizing its delivery mechanisms, and integrating it with other therapeutic modalities for enhanced efficacy and safety.
Summary
The potential of doctors using herpes virus to fight brain cancer is significant, offering a novel approach to this challenging disease. While promising, the therapy also carries potential risks and ethical considerations. Ongoing research and clinical trials are crucial to further refine the treatment and address these concerns. The future of this innovative approach hinges on careful consideration of both the potential benefits and the inherent risks, leading to improved outcomes and potentially life-saving therapies for patients battling brain cancer.