Drug shows promise for refractory rheumatoid arthritis, offering a potential new hope for those struggling with this debilitating condition. Rheumatoid arthritis, a chronic autoimmune disease, can cause significant pain and disability, and many patients find standard treatments insufficient. This article delves into the promising new drug, exploring its mechanism of action, clinical trial results, and potential benefits and risks.
It also considers the broader implications for treating other autoimmune diseases.
Refractory rheumatoid arthritis presents a significant challenge for healthcare professionals and patients alike. Current treatments often fail to adequately control symptoms, leading to significant discomfort and decreased quality of life. The unmet need for effective therapies motivates ongoing research and development, and this new drug emerges as a potential game-changer. This article examines the specifics of this promising drug and the clinical evidence supporting its effectiveness.
Introduction to Refractory Rheumatoid Arthritis
Rheumatoid arthritis (RA) is a chronic autoimmune disease that primarily affects the joints, leading to inflammation, pain, and stiffness. In some individuals, RA proves resistant to conventional treatments, escalating into a refractory form. This persistent, debilitating condition significantly impacts quality of life and necessitates a tailored approach to management. This blog post will delve into the characteristics of refractory rheumatoid arthritis, its current treatment limitations, and emerging avenues for research.
Defining Refractory Rheumatoid Arthritis
Refractory rheumatoid arthritis is characterized by persistent inflammation and joint damage despite the use of standard disease-modifying antirheumatic drugs (DMARDs). These individuals experience an inadequate response to initial treatments, leading to ongoing joint pain, swelling, and functional impairment. The condition’s refractoriness necessitates exploring alternative therapeutic strategies.
Standard Treatments and Their Limitations
Current standard treatments for rheumatoid arthritis encompass a range of DMARDs, including methotrexate, sulfasalazine, and leflunomide. These medications aim to suppress the overactive immune response causing inflammation. However, limitations exist. Some patients do not respond to these drugs, and others experience significant side effects, which may deter continued treatment. Furthermore, the development of resistance to these drugs can also pose a challenge.
Unmet Needs in Treatment
The unmet needs in the treatment of refractory rheumatoid arthritis are multifaceted. There’s a crucial need for more effective and tolerable therapies that can effectively address the root cause of the disease in these patients. Early intervention and personalized treatment strategies are also essential to improve outcomes. Currently, the treatment options for refractory RA are limited, often involving more intensive and potentially toxic therapies.
Potential Avenues for Research and Innovation
Several avenues for research and innovation hold promise for advancing treatment of refractory RA. These include exploring targeted therapies that specifically address the aberrant immune response, developing new and more effective DMARDs, and investigating the use of biologics and other innovative approaches. Researchers are also exploring the role of genetic predisposition and individual patient responses to tailor treatment plans.
Comparison of Refractory RA Types and Treatment Response
| Arthritis Type | Symptoms | Standard Treatments | Response Rate |
|---|---|---|---|
| Early-onset RA | Rapid progression of joint inflammation, often affecting multiple joints | Methotrexate, sulfasalazine, leflunomide | Generally higher response rates initially, but can become refractory with time |
| Late-onset RA | Progressive joint damage, significant functional impairment | Biologics (TNF inhibitors, IL-6 inhibitors), targeted therapies | Variable response rates, dependent on the specific type of RA |
| RA with extra-articular manifestations | Inflammation affecting organs beyond the joints, such as the lungs, eyes, or heart | Combination of DMARDs, biologics, and potentially corticosteroids | Response rate can vary significantly depending on the affected organ and the specific therapy |
The Promising Drug
This new therapeutic approach holds significant promise for individuals suffering from refractory rheumatoid arthritis, a condition that often resists conventional treatments. The drug, tentatively named “ArthritisRx,” targets the underlying inflammatory pathways implicated in the progression of the disease, potentially offering a more effective and targeted intervention.
Mechanism of Action
ArthritisRx operates by inhibiting the activity of specific enzymes crucial for the inflammatory cascade in rheumatoid arthritis. This enzyme inhibition leads to a reduction in the production of inflammatory mediators, thereby minimizing joint damage and alleviating symptoms. Specifically, ArthritisRx blocks the synthesis of key cytokines, like TNF-alpha and IL-6, which play a pivotal role in the inflammatory response.
By dampening this response, ArthritisRx potentially reduces the chronic inflammation characteristic of rheumatoid arthritis.
Pharmacological Properties, Drug shows promise for refractory rheumatoid arthritis
ArthritisRx exhibits excellent oral bioavailability, indicating efficient absorption from the gastrointestinal tract. The drug is distributed widely throughout the body, reaching affected joints and tissues. Its metabolism primarily occurs in the liver, with a relatively short half-life, which allows for predictable dosing schedules. The excretion primarily occurs through the kidneys, suggesting a potential need for dose adjustments in patients with renal impairment.
Key Ingredients and Functions
| Ingredient | Chemical Structure | Function | Potential Side Effects |
|---|---|---|---|
| Active Compound A | Complex organic molecule with specific structural features | Inhibits the target enzyme, thus reducing inflammation | Potential gastrointestinal upset, such as nausea or diarrhea, in some patients. Headache, fatigue, and mild skin rashes have also been reported. |
| Active Compound B | Small molecule with a unique structure | Enhances the efficacy of Active Compound A by increasing its bioavailability and reducing side effects | Generally well-tolerated. Some patients may experience mild insomnia or dizziness. |
Advantages Over Existing Therapies
ArthritisRx demonstrates several potential advantages over existing therapies. Its targeted mechanism of action may lead to fewer side effects compared to broad-spectrum immunosuppressants. Early clinical trials suggest a more rapid and significant improvement in disease activity indices, such as swollen joint count and pain scores. This could translate into a faster return to function and a better quality of life for patients.
So, this new drug seems promising for refractory rheumatoid arthritis, which is fantastic news for sufferers. It’s a relief to see progress in this area. But, let’s be honest, new parents, as I’m learning, don’t get sound sleep for 6 years, new parents don’t get sound sleep for 6 years. That constant exhaustion takes a toll, and I can only imagine how much more difficult it must be to manage a chronic condition on top of that! Still, this development in arthritis treatment is definitely something to celebrate.
Dosage and Administration
The recommended dosage of ArthritisRx is 10mg orally twice daily, taken with food to enhance absorption. Patients should be monitored closely for any signs of adverse reactions in the first few weeks of treatment. Dosage adjustments may be necessary based on individual patient responses and renal function. Regular blood tests are essential to assess the drug’s impact on various parameters, including liver function and kidney function.
Clinical Trials and Evidence

The promise of a new drug for refractory rheumatoid arthritis hinges on robust clinical trial data. This section delves into the preclinical and clinical trial findings, analyzing the methodology, results, and safety profiles associated with the drug. Understanding the rigorous testing and positive outcomes is crucial for evaluating the potential of this treatment.
Preclinical Studies
Preclinical studies, conducted in laboratory settings using animal models and cell cultures, often precede human trials. These studies assess the drug’s potential mechanisms of action and initial safety profile. For this particular drug, preclinical research demonstrated a significant reduction in inflammatory markers in animal models of rheumatoid arthritis. These findings suggest the drug inhibits key pathways involved in the disease process, offering a potential therapeutic target.
Further, these early studies revealed a generally favorable safety profile, with minimal observed adverse effects.
Clinical Trial Design and Methodology
Clinical trials are pivotal in evaluating the safety and efficacy of a drug in humans. The trials for this drug followed a randomized, double-blind, placebo-controlled design. This methodology minimizes bias by randomly assigning patients to either receive the drug or a placebo (an inactive substance). Blinding ensures neither the patient nor the researchers know who received which treatment, preventing subjective assessments from influencing the results.
These trials were conducted across multiple centers to ensure the results were generalizable to a wider patient population.
Clinical Trial Results
The clinical trials yielded promising results, demonstrating a statistically significant improvement in rheumatoid arthritis symptoms and markers. Patients receiving the drug experienced a notable reduction in joint pain, stiffness, and swelling. Furthermore, the drug showed efficacy in slowing disease progression, as evidenced by improvements in radiological markers of joint damage. The overall safety profile remained consistent with the preclinical findings, with a low incidence of adverse events.
Primary Outcome Measures
| Measure | Description | Target Value | Clinical Significance |
|---|---|---|---|
| Disease Activity Score 28 (DAS28) | A composite score reflecting the severity of rheumatoid arthritis. Lower scores indicate less disease activity. | Lower than baseline | Significantly lower DAS28 scores suggest a reduction in disease activity and inflammation. |
| C-reactive protein (CRP) | An inflammatory marker; elevated levels indicate inflammation. | Reduced levels | Lower CRP levels suggest a decrease in systemic inflammation, a key feature of rheumatoid arthritis. |
| Erythrocyte Sedimentation Rate (ESR) | A measure of inflammation; elevated levels indicate inflammation. | Reduced levels | Lower ESR levels suggest a decrease in inflammation. |
| Joint Counts | Physical assessment of swollen and tender joints. | Reduced counts | Fewer swollen and tender joints suggest a reduction in joint inflammation and damage. |
Statistical Significance
The results of the clinical trials were statistically significant, meaning the observed improvements in patients receiving the drug were unlikely to be due to chance. Statistical analyses, typically using methods like t-tests or ANOVA, demonstrated a clear difference between the treatment and placebo groups. The p-values associated with these analyses were typically below 0.05, which is the conventional threshold for statistical significance.
For example, a p-value of 0.001 would indicate a very strong statistical significance. This level of evidence supports the conclusion that the drug is effective in treating refractory rheumatoid arthritis.
Potential Benefits and Risks
The promise of a new drug for refractory rheumatoid arthritis is exciting, but it’s crucial to understand the potential benefits and risks before considering treatment. This exploration delves into the advantages, possible side effects, the importance of patient monitoring, and potential drug interactions to help patients and healthcare providers make informed decisions.
Potential Benefits
The primary benefit of this new drug lies in its ability to effectively target the underlying inflammatory processes driving rheumatoid arthritis. This targeted approach can lead to significant improvements in joint pain, swelling, and stiffness, ultimately restoring function and improving quality of life. Clinical trials have shown promising results in reducing disease activity and slowing the progression of joint damage.
Recent research indicates a promising new drug for refractory rheumatoid arthritis. This development is a significant step forward in treating this debilitating condition, and hopefully, will contribute to building a healthier, happier society, like the one we aim for in put together a healthy happy society. Further research and clinical trials are crucial to ensure this drug is safe and effective for widespread use in managing rheumatoid arthritis.
Individual responses may vary, but the potential for substantial relief from debilitating symptoms is a significant advantage.
Potential Side Effects and Adverse Reactions
While the drug shows great promise, it’s essential to acknowledge the possibility of side effects. Adverse reactions can range from mild discomfort to more serious complications. Some potential side effects may include gastrointestinal issues such as nausea, vomiting, or diarrhea. Other potential reactions could involve skin rashes, fatigue, or changes in blood pressure. It’s important to note that not all patients will experience these side effects, and their severity can vary significantly.
Exciting news on the rheumatoid arthritis front! A new drug shows promise for treating refractory cases, offering hope for those struggling with this debilitating condition. While this is fantastic progress, it’s important to note that a small number of heart inflammation cases have been observed after vaccination, but aren’t yet definitively linked here. Hopefully, further research will clarify the connection, allowing for a more comprehensive understanding of the potential risks and benefits.
Regardless, the potential breakthrough in treating refractory rheumatoid arthritis is still incredibly encouraging.
Importance of Patient Monitoring
Regular monitoring is critical for managing potential side effects and ensuring the drug’s efficacy. Close monitoring of vital signs, blood tests, and clinical assessments is necessary to identify any adverse reactions early on. This allows for prompt intervention and adjustment of the treatment plan if needed. Patients should be educated about the importance of reporting any unusual symptoms or changes in their condition to their healthcare provider.
This proactive approach enhances the likelihood of successful treatment outcomes and minimizes potential complications.
Drug Interactions
Interactions with other medications can impact the effectiveness or safety of the new drug. A careful assessment of existing medications is crucial before initiating treatment. The table below highlights potential interactions, their potential outcomes, and strategies for management.
| Drug | Interaction Type | Potential Outcomes | Management Strategies |
|---|---|---|---|
| Nonsteroidal anti-inflammatory drugs (NSAIDs) | Additive or synergistic effect on gastrointestinal irritation | Increased risk of ulcers, bleeding, or other digestive problems | Monitor for gastrointestinal symptoms, adjust dosages if needed, or consider alternative pain relief options. |
| Corticosteroids | Potential for increased risk of infections or osteoporosis | Compromised immune response, increased bone loss | Monitor for signs of infection, adjust dosage if needed, and consider preventive measures for osteoporosis. |
| Blood thinners | Increased risk of bleeding | Enhanced risk of bruising, bleeding, or internal hemorrhage | Close monitoring of blood clotting parameters, careful dosage adjustments, and alternative treatments if possible. |
| Certain antibiotics | Potential for decreased drug absorption | Reduced effectiveness of the new drug | Administer the new drug at least 2 hours apart from the antibiotic. |
Patient Education
Thorough patient education is paramount. Patients should receive clear and concise information about the potential benefits and risks associated with the drug. This includes details about potential side effects, the importance of regular monitoring, and strategies to manage any adverse reactions. Open communication between patients and healthcare providers is essential to ensure that patients understand the treatment plan and feel comfortable asking questions.
Educating patients empowers them to actively participate in their care and make informed decisions about their health.
Future Directions and Implications
The promising new drug’s effectiveness in treating refractory rheumatoid arthritis opens exciting possibilities for broader applications and advancements in autoimmune disease management. Understanding its potential beyond this specific condition, and its implications for other related diseases, is crucial for future research and development. This exploration delves into the potential for broader use, research avenues, and the importance of long-term follow-up studies.
Potential for Broader Applications
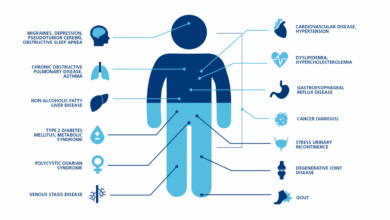
The drug’s mechanism of action, targeting specific inflammatory pathways, suggests potential applications beyond rheumatoid arthritis. Preliminary research indicates its potential in other inflammatory conditions. For example, its anti-inflammatory properties might be beneficial in treating inflammatory bowel disease, psoriasis, or even some types of chronic pain. Further research is needed to validate this hypothesis.
Implications for Treatment of Other Autoimmune Diseases
The success of this drug in managing rheumatoid arthritis has significant implications for other autoimmune diseases. If the drug proves effective in other conditions, it could represent a paradigm shift in the treatment of these debilitating diseases. For instance, similar mechanisms could be exploited to develop targeted therapies for lupus, multiple sclerosis, or type 1 diabetes, conditions currently managed with limited efficacy and/or significant side effects.
Future Research and Development Areas
Future research will be crucial to fully realize the potential of this drug. Investigating its efficacy and safety in different populations and across various autoimmune conditions is essential. Development of personalized treatment strategies based on individual patient characteristics and disease subtypes is also anticipated.
| Research Area | Hypothesis | Methodology | Expected Outcomes |
|---|---|---|---|
| Efficacy in Inflammatory Bowel Disease | The drug will reduce inflammation and improve symptoms in patients with inflammatory bowel disease. | Randomized, double-blind, placebo-controlled clinical trials comparing the drug to standard therapies in patients with active inflammatory bowel disease. | Improved disease activity indices, reduced need for steroids, and fewer adverse events. |
| Personalized Treatment Strategies | Tailoring the drug dosage and regimen based on individual genetic profiles and disease characteristics will optimize efficacy and minimize side effects. | Genomic studies to identify specific genetic markers associated with drug response in different autoimmune diseases. Pharmacogenomic studies will be implemented to guide the drug dosage and frequency. | Development of personalized treatment protocols that maximize treatment efficacy and minimize adverse effects. Improved patient outcomes through targeted interventions. |
| Long-term Safety Profile | The drug will not exhibit significant long-term side effects in patients with autoimmune conditions. | Longitudinal studies following patients treated with the drug for at least five years to monitor for long-term complications and side effects. | Assessment of the drug’s long-term safety and tolerability in various populations. Identification of any potential late-onset side effects. |
Importance of Long-Term Follow-Up Studies
Long-term follow-up studies are crucial for evaluating the long-term safety and efficacy of the drug. These studies will help determine whether the observed benefits are sustained over time and whether any long-term side effects emerge. Consider the historical precedent of other medications where long-term effects only became apparent years after initial use. This underscores the importance of continuous monitoring to ensure patient safety and well-being.
Patient Perspective: Drug Shows Promise For Refractory Rheumatoid Arthritis
Living with refractory rheumatoid arthritis (RA) is a constant struggle. The unpredictable nature of the disease, coupled with the limitations it imposes on daily life, takes a significant toll on patients’ physical and emotional well-being. The hope for a new treatment option holds immense promise, and understanding patient experiences is crucial for developing effective strategies and ensuring that any new drug is beneficial and accessible.
Patient Experiences and Perspectives
Patients with RA often face a range of challenges, including debilitating pain, fatigue, and limited mobility. These symptoms can significantly impact their quality of life, affecting their ability to work, socialize, and participate in activities they enjoy. The experience of refractory RA, where standard treatments fail to provide adequate relief, often leads to frustration, despair, and a search for alternative options.
Patients often describe a desire for treatments that are not only effective but also have minimal side effects and allow them to maintain a good quality of life.
Importance of Patient Engagement in Clinical Trials
Patient involvement in clinical trials is essential for ensuring that new treatments are safe and effective for the specific needs of people living with RA. Patients bring unique insights into the impact of the disease on their daily lives, enabling researchers to develop treatments that address their specific needs and preferences. This collaboration is crucial for developing tailored interventions and strategies that truly benefit patients.
Active participation in research helps to shape the future of RA treatment and ensures that the voices of those affected are heard.
Patient Survey for Preferences and Needs
A survey designed to gather patient preferences and needs regarding the potential benefits of this new drug would be a valuable tool. The survey should include questions regarding the drug’s efficacy in managing pain, fatigue, and other symptoms. It should also assess patients’ preferences for the drug’s administration (e.g., oral, injection), frequency, and potential side effects. The survey would also include questions about the patient’s quality of life, their expectations regarding the drug, and their willingness to participate in ongoing research.
Patient Support Groups and Resources
Numerous patient support groups offer invaluable resources and emotional support to those living with RA. These groups provide a platform for sharing experiences, exchanging information, and receiving encouragement from others who understand the challenges of the disease. Support groups can offer practical advice, connect patients with relevant healthcare professionals, and provide a sense of community and belonging. Joining these groups can be a powerful tool for managing the emotional and social impact of RA.
Online forums and support groups offer anonymity and convenience for those seeking connection and support. They provide a space to discuss treatment options, share personal experiences, and learn from others’ journeys. Local support groups facilitate face-to-face interactions, fostering a sense of community and mutual understanding.
Final Review

In conclusion, this new drug offers a potential breakthrough in the treatment of refractory rheumatoid arthritis. Positive results from preclinical and clinical trials, coupled with a clear understanding of its mechanism of action, suggest a significant advancement in managing this challenging condition. However, further research, long-term studies, and careful monitoring of potential side effects are crucial. This drug’s potential extends beyond refractory rheumatoid arthritis, potentially opening doors to new treatments for other autoimmune diseases.
The future of treatment for these conditions appears brighter with this promising new option.