How should I prepare for a meeting with the clinical trials research coordinator or doctor? This guide will equip you with the knowledge and tools to navigate these crucial interactions. From understanding the meeting’s purpose to mastering the post-meeting follow-up, we’ll cover everything you need to feel prepared and confident.
Preparing for a clinical trial meeting goes beyond simply gathering information. It’s about actively engaging with the process, understanding your role, and anticipating potential questions. By organizing your thoughts and materials effectively, you can ensure a productive and successful discussion.
Understanding the Meeting’s Purpose
Navigating the world of clinical trials can feel overwhelming. Knowing the purpose of your meeting with a clinical trials research coordinator or doctor beforehand can significantly ease the process and ensure you get the most out of the interaction. This section will Artikel the possible reasons for these meetings, the information you should gather, expected outcomes, and the benefits of preparation.
Getting ready for a meeting with the clinical trials research coordinator or doctor? It’s crucial to have your questions prepared. Think about your medical history, especially considering the rising trend of women in their 30s having babies than in their 20s, as seen in this recent study. Knowing your family history and any relevant details is key to a productive discussion and to understanding your potential participation in the trial.
Having all your paperwork organized beforehand will also help the meeting run smoothly.
Possible Reasons for Meeting
Understanding the reasons for your meeting helps you prepare effectively. These meetings can serve various purposes, including:
- Enrollment in a clinical trial: The coordinator will discuss the trial’s eligibility criteria, procedures, and potential benefits and risks.
- Clarifying trial details: This includes understanding the trial’s specific protocols, schedules, and the doctor’s role in the trial.
- Addressing concerns or questions: You may have questions about the trial’s design, potential side effects, or your role as a participant.
- Obtaining information about ongoing trial status: This is important to track the trial’s progress and understand the impact of your participation.
- Reviewing your medical history and current health status: This ensures that you meet the criteria for the trial and are fit to participate.
Information to Gather
Thorough preparation is key. Before the meeting, gather relevant information about yourself and the trial. This might include:
- Personal medical history: This includes past diagnoses, treatments, and any allergies.
- Current medications: This encompasses prescription and over-the-counter medications, supplements, and herbal remedies.
- Relevant test results: Include any recent lab work, imaging scans, or other diagnostic results.
- Trial-specific details: Review the trial’s protocol, eligibility criteria, and contact information.
- Questions to ask: Write down specific questions about the trial or your participation.
Expected Outcomes of the Meeting
A productive meeting will provide clear answers and expectations. You can anticipate:
- Clarification of trial details: Understanding the trial’s procedures, schedules, and requirements.
- Confirmation of eligibility: Determining if you meet the criteria to participate in the trial.
- Discussion of potential risks and benefits: Gaining a comprehensive understanding of the trial’s impact on your health.
- Answering your questions: Addressing any concerns or uncertainties you have about the trial.
- Agreement on next steps: Defining the actions required to move forward with your participation.
Benefits of Preparation
Preparing for your meeting is invaluable. It allows you to:
- Feel more confident and informed: This can reduce anxiety and increase your comfort level.
- Maximize the meeting’s effectiveness: Ensuring you get the information you need and ask the right questions.
- Reduce the likelihood of misunderstandings: Clear communication fosters a smoother interaction.
- Make informed decisions: Having all the facts will empower you to make the best choice for your health.
- Streamline the process: Well-prepared meetings typically lead to faster progress and enrollment.
Comparing Meetings: Coordinator vs. Doctor, How should i prepare for a meeting with the clinical trials research coordinator or doctor
The following table highlights key differences between meeting with a research coordinator and a doctor.
| Characteristic | Research Coordinator | Doctor |
|---|---|---|
| Primary Focus | Trial logistics, enrollment, and eligibility | Patient care, overall health, and treatment |
| Information Provided | Trial specifics, procedures, and next steps | General medical guidance, patient history, and recommendations |
| Decision-Making | Facilitating participation and ensuring eligibility | Diagnosing, treating, and managing health conditions |
| Frequency of Interaction | More frequent, often throughout the trial | Dependent on the patient’s needs and the trial’s requirements |
Gathering Essential Information: How Should I Prepare For A Meeting With The Clinical Trials Research Coordinator Or Doctor
Before diving into a meeting with a clinical trials research coordinator or doctor, thorough preparation is key. Understanding the meeting’s purpose is just the first step. Next, proactive information gathering ensures a productive discussion and allows you to get the most out of the interaction. This involves reviewing relevant documents, formulating insightful questions, and creating a system to organize the collected information.
Key Documents to Review
To maximize the value of your meeting, meticulously review any materials provided in advance. This might include study protocols, informed consent forms, patient recruitment materials, or data summaries. Understanding these documents beforehand allows you to identify potential areas of interest or concern, and ensures you’re well-informed before engaging in discussion.
Getting ready for a meeting with the clinical trials research coordinator or doctor? First, jot down any questions you have, especially about the specific trial. Understanding the potential risks and benefits is key, and knowing more about the current research on why more young people are getting colorectal cancer, like this article explains why are more young people getting colorectal cancer , will help you feel more prepared and engaged in the discussion.
Bring a list of your current medications and any relevant medical history. This thorough preparation will make the meeting productive and beneficial for you.
- Study protocol: This document Artikels the objectives, methodology, and procedures of the clinical trial. Familiarize yourself with the trial design, inclusion/exclusion criteria, and the overall study goals.
- Informed consent forms: Reviewing these forms provides crucial insight into the patient’s rights and responsibilities. Understanding the procedures and risks involved in the trial is vital.
- Patient recruitment materials: Examining these documents allows you to understand the target population for the clinical trial and the methods used to recruit patients.
- Data summaries: Reviewing any available data summaries provides a preliminary understanding of the trial’s progress and potential outcomes.
Questions to Ask Yourself
Before the meeting, consider a series of self-reflective questions to clarify your needs and goals. This proactive approach helps in focusing the meeting on the most important points and ensures you address the critical aspects you want answered.
- What specific aspects of the clinical trial are most important to me? This might include questions regarding specific treatments, expected outcomes, or the duration of the trial.
- What are my personal goals and expectations for this meeting? Identifying these helps focus the discussion on the most critical points.
- What are my potential concerns regarding the trial? This allows you to identify and address potential problems before the meeting.
- What are my expectations regarding the role of the research coordinator or doctor? Understanding their roles and responsibilities will allow for more effective interaction.
Questions to Ask the Research Coordinator/Doctor
Prepare a list of specific, targeted questions to guide the meeting. These questions should delve into the details of the clinical trial, allowing for a comprehensive understanding of its aspects.
- What are the eligibility criteria for patient inclusion in the trial? Understanding these criteria helps identify potential candidates for the study.
- What are the anticipated timelines for patient recruitment and data collection? Understanding these timelines helps in gauging the trial’s progress and its potential completion.
- What are the potential risks and benefits associated with participating in the trial? Understanding these elements helps patients make informed decisions about their involvement.
- What is the anticipated duration of the trial? This allows you to gauge the trial’s expected duration and potential implications.
Question and Answer Template
Creating a template to organize your questions and answers ensures you can easily reference the information later. This structured approach allows for effective follow-up and ensures you have a record of the critical details discussed.
| Question | Answer |
|---|---|
| What are the eligibility criteria for patient inclusion in the trial? | … |
| What are the anticipated timelines for patient recruitment and data collection? | … |
| What are the potential risks and benefits associated with participating in the trial? | … |
| What is the anticipated duration of the trial? | … |
Organizing Collected Information
Organizing the collected information for easy reference ensures that you can quickly access the key details discussed during the meeting. A well-organized system allows you to review the information later, reinforcing your understanding of the trial and your role in it.
A simple method is to create a document with sections corresponding to the different aspects of the meeting. This might include sections on eligibility criteria, timelines, risks, and benefits. Each section can include the questions, answers, and any relevant supporting documentation.
Preparing Your Presentation
Stepping into a clinical trial meeting can feel daunting, but preparation is key. A well-structured presentation of your medical history, questions, and understanding of the trial can significantly contribute to a productive and positive experience. By meticulously organizing your thoughts and using clear communication, you’ll empower yourself to fully participate and contribute to the process.The meeting is a dialogue, not a monologue.
Coming prepared with a clear and concise presentation of your needs, concerns, and understanding of the trial will allow for a more focused and informative exchange of information. This proactive approach ensures that you get the most out of the meeting and facilitates a smoother understanding between you and the clinical trial team.
Summarizing Your Medical History
A concise and accurate summary of your medical history is crucial for the research team to understand your overall health status in relation to the trial. Avoid lengthy narratives. Instead, focus on pertinent details relevant to the trial’s objectives. This will save time and ensure clarity.
- Highlight key diagnoses, treatments, and procedures, emphasizing any conditions that might affect your eligibility or participation in the trial.
- Include dates and details of past medical events to provide a comprehensive overview of your health history.
- Summarize current medications, including dosage, frequency, and reason for taking each medication. If you have any allergies, be sure to list them, including reactions.
Presenting Your Questions and Concerns
Anticipating questions and concerns beforehand will help you organize your thoughts and present them effectively. Prioritize questions based on their importance to your understanding of the trial.
- Organize your questions into logical categories. For example, you might have questions about the trial’s procedures, potential side effects, or your role in the study.
- Consider writing down your questions and concerns before the meeting, and prioritize them in order of importance.
- Use clear and concise language to frame your questions, ensuring they are easily understood by the research coordinator or doctor.
Presenting Your Current Medications and Allergies
Providing a clear list of your current medications, including dosage, frequency, and reasons for taking them, is vital. Similarly, a precise listing of your allergies is essential.
Getting ready for a meeting with your clinical trials research coordinator or doctor? Knowing your medical history inside and out is key, but also remember that heart disease is the top cause of death in women but few know warning signs. This article highlights the importance of recognizing early symptoms. Prepare by jotting down questions, any concerns, and a list of medications you’re currently taking.
This will ensure a productive and informative discussion.
| Medication | Dosage | Frequency | Reason |
|---|---|---|---|
| Example Medication 1 | 10mg | Twice daily | High blood pressure |
- Be prepared to explain any potential interactions between your medications and the trial treatment.
- Clearly state any known allergies, including the specific allergen and the type of reaction experienced.
Presenting Your Understanding of the Clinical Trial
Demonstrating your comprehension of the trial protocol and your responsibilities will facilitate a productive conversation.
- Summarize the trial’s purpose and goals, showing your grasp of the research objectives.
- Highlight key elements of the trial’s procedures, emphasizing aspects you find particularly important or concerning.
- Express your understanding of your role in the trial. This will help the research team understand your expectations and ensure that you feel comfortable and well-informed.
Using Clear and Concise Language
Using clear and concise language avoids misunderstandings and ensures effective communication.
“Instead of asking ‘How long will the trial last?’, ask ‘What is the estimated duration of the trial?'”
- Employ precise terminology to describe your medical history, medications, and allergies.
- Focus on the specifics of the clinical trial, highlighting key details like the trial’s phases, duration, and procedures.
- Ask clarifying questions if anything is unclear. This is a critical part of the process. Don’t hesitate to ask if you need clarification.
Managing Expectations and Logistics
Navigating clinical trial meetings requires a proactive approach, understanding the common procedures, and anticipating potential challenges. This section provides insights into managing the logistics and expectations to ensure a productive and positive experience. Knowing what to expect can ease anxieties and allow you to focus on the critical aspects of the discussion.
Common Procedures During a Clinical Trial Meeting
Clinical trial meetings often follow a structured format, starting with introductions and an overview of the trial’s objectives. The coordinator or doctor will likely discuss the patient’s current status within the trial, review any recent data, and address any concerns or questions. This is a crucial opportunity to clarify any ambiguities and gain a better understanding of the trial’s progress and potential implications for you.
Expected Length of a Meeting
The duration of a clinical trial meeting can vary depending on the complexity of the discussion and the specific needs of the participant. Typically, these meetings can range from 30 minutes to an hour. However, it’s not uncommon for the meeting to extend beyond the initially estimated time, especially if there are complex issues or follow-up questions. Realistically, be prepared for the meeting to last longer than the estimated time, as important information may need additional time to be fully addressed.
Potential Challenges During a Meeting
Several challenges may arise during a clinical trial meeting. Misunderstandings about trial procedures, concerns regarding the patient’s health status, or unforeseen logistical issues are common. Furthermore, technical difficulties or delays in communication can sometimes impact the flow of the meeting.
Possible Solutions to Overcome Potential Challenges
Addressing potential challenges proactively can make a significant difference in the success of the meeting. Having a list of prepared questions can help manage any uncertainties and ensure you receive clear answers. If technical difficulties arise, having a backup communication method, such as a phone or another device, is crucial. Be prepared to seek clarification if anything is unclear.
For example, if there is a misunderstanding about a procedure, ask clarifying questions to ensure everyone is on the same page.
Scheduling a Follow-up Meeting
If necessary, schedule a follow-up meeting to discuss any outstanding issues or questions. A clear and concise agenda for the follow-up meeting is crucial. For instance, clearly stating the specific issues that need addressing ensures the meeting stays focused and productive. Include a detailed description of the items needing attention in the meeting’s agenda, to ensure efficiency and clarity.
Also, confirm the meeting time and date with the coordinator or doctor beforehand to avoid any scheduling conflicts.
Post-Meeting Actions
Navigating the follow-up phase after a clinical trial meeting with research coordinators or doctors is crucial for success. Effective action after the meeting ensures that agreed-upon steps are implemented correctly and efficiently, leading to a positive outcome. This section details the critical steps for post-meeting action, focusing on documenting the meeting, clarifying any ambiguities, and tracking progress.
Reviewing Meeting Notes and Follow-Up Actions
A well-structured checklist for reviewing meeting notes and subsequent actions is essential for keeping track of commitments. This checklist ensures that all agreed-upon items are addressed, reducing the risk of omissions and misunderstandings.
- Create a dedicated document to record the meeting minutes, including attendees, key discussion points, decisions made, and assigned responsibilities.
- Clearly define the specific actions to be taken and the individuals responsible for each action.
- Establish a timeframe for completing each action. This helps maintain momentum and ensure timely progress.
- Include a column for the status of each action (e.g., completed, in progress, pending). This provides a dynamic view of the project’s progress.
Documenting Meeting Outcomes
Thorough documentation of meeting outcomes serves as a vital record of decisions, agreements, and next steps. It provides a clear reference point for future discussions and ensures consistency in actions.
- Record all key decisions and agreements made during the meeting, including specific details about the agreed-upon actions.
- Note the date and time of the meeting for reference purposes.
- Include the names of all attendees and their roles.
- Clearly document any outstanding questions or issues that require further clarification. This prevents delays or errors in future phases.
Following Up on Discussed Items
Effective follow-up is crucial for maintaining momentum and ensuring that agreed-upon items are addressed timely. It demonstrates respect for the time and effort invested in the meeting.
- Example 1: If a doctor suggests a specific data analysis approach, send a follow-up email outlining the proposed steps, confirming understanding, and asking if any clarifications are needed.
- Example 2: If the research coordinator assigned a task to a specific team member, send a confirmation email with a clear timeline for completion and potential roadblocks.
- Example 3: Schedule a brief follow-up meeting to discuss any issues that arise or to provide updates on the progress of assigned tasks.
Seeking Clarification on Unclear Points
Addressing unclear points promptly prevents misinterpretations and ensures that everyone is on the same page. This minimizes potential errors and delays.
- If a point is unclear, write it down and ask for clarification promptly. This shows engagement and respect for the meeting’s purpose.
- Reiterate the unclear point to ensure understanding. This can help the coordinator or doctor clarify the intent.
- If a point is still unclear, schedule a brief follow-up call or email to clarify the confusion. Avoid prolonged delays in resolving ambiguity.
Ensuring Accurate Record-Keeping
Accurate record-keeping is critical for maintaining a clear audit trail and ensuring accountability. A well-maintained record ensures traceability and efficiency in the clinical trial process.
- Use a shared online document platform for all meeting notes, action items, and follow-up communication.
- Employ a standardized format for recording meeting minutes and action items. This improves readability and consistency.
- Ensure all participants have access to the shared records and can update them as needed. This promotes transparency and collaborative work.
Visual Aids and Examples
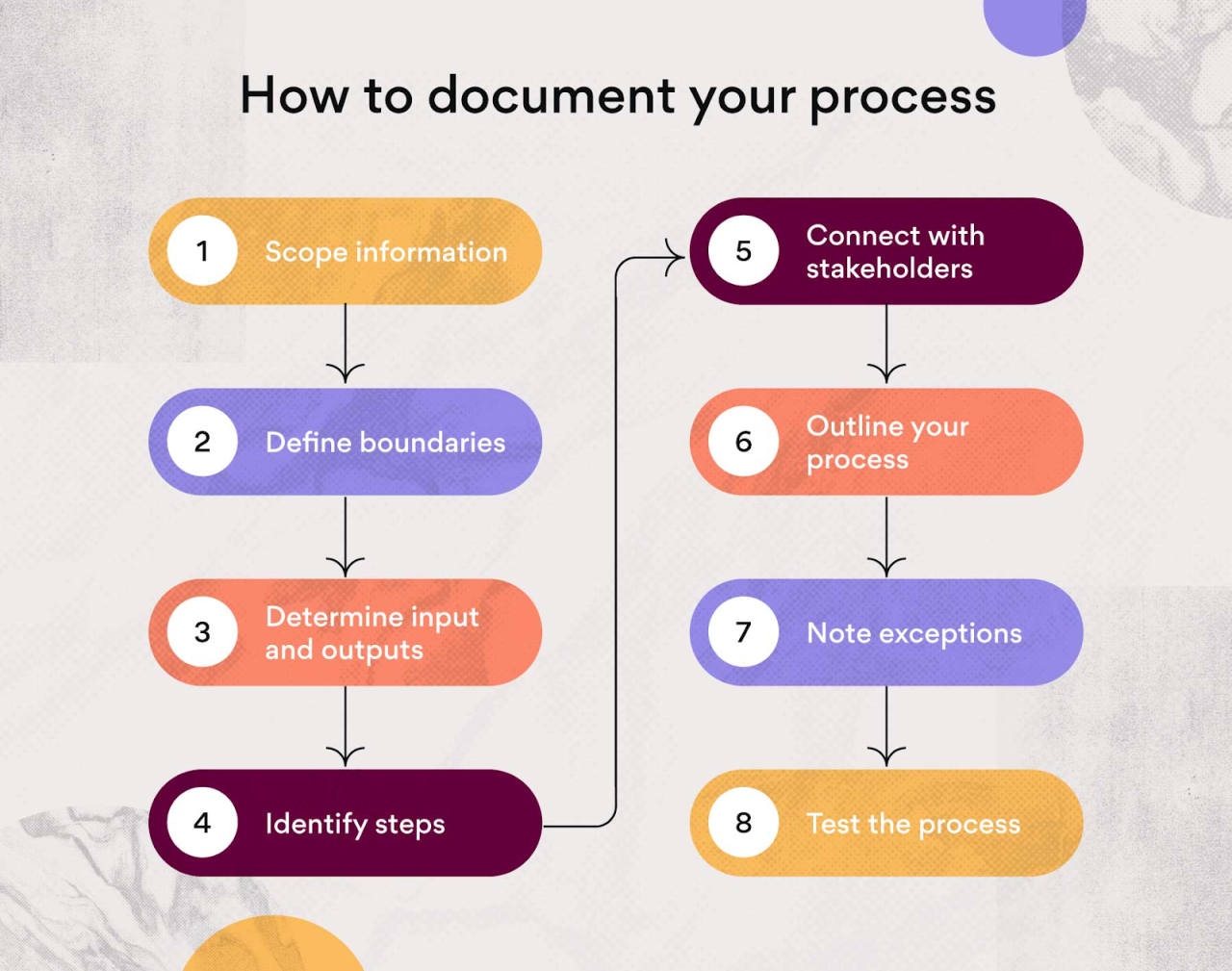
Presenting information clearly and concisely is crucial for any meeting, especially when discussing complex medical topics. Visual aids are powerful tools to enhance understanding and engagement. They can transform potentially dry data into easily digestible insights, making your points memorable and impactful. Use them strategically to guide your conversation and leave a lasting impression.
Importance of Visual Aids
Visual aids, like charts and graphs, significantly enhance the effectiveness of communication. They make complex information more accessible and understandable for both the clinical trials research coordinator and the doctor. Visual representations often convey information more quickly and efficiently than textual descriptions.
| Visual Aid | Importance |
|---|---|
| Charts | Excellent for displaying trends, comparisons, and distributions of data. |
| Graphs | Ideal for visualizing relationships between variables, highlighting patterns, and showcasing correlations. |
| Diagrams | Helpful for illustrating processes, structures, and mechanisms, particularly useful for outlining the clinical trial methodology. |
| Images/Illustrations | Effective for demonstrating medical conditions, equipment, or procedures, enhancing understanding and engagement. |
Visual Aids for Medical Data
Visual aids are essential for presenting medical data effectively. They allow you to quickly highlight key findings, patterns, and trends in a way that’s easy for the coordinator and doctor to grasp. Here’s a table illustrating the use of visual aids for medical data:
| Type of Data | Visual Aid | Example |
|---|---|---|
| Patient demographics | Bar charts, pie charts | Displaying the distribution of patient ages, genders, or ethnicities. |
| Treatment response | Line graphs, scatter plots | Visualizing the progression of symptoms or the effectiveness of a treatment over time. |
| Side effect profiles | Bar charts, tables | Comparing the frequency and severity of different side effects across treatment groups. |
| Laboratory results | Scatter plots, line graphs | Illustrating the relationship between laboratory markers and treatment outcomes. |
Example: Presenting Medical History
A crucial visual aid for medical history involves a timeline. Representing key events like diagnoses, treatments, hospitalizations, and significant life events on a timeline visually communicates the patient’s medical history and context. This approach allows for a clear overview of the patient’s journey, highlighting relevant factors that might influence the clinical trial participation.
“A well-structured timeline clearly depicts the progression of a patient’s medical history, facilitating a comprehensive understanding for the research team.”
Presenting Medication Details
Presenting medication details involves a table outlining medications, dosages, frequencies, and potential interactions. This structured format enables quick comprehension of the patient’s current medication regimen. Use clear labeling and concise descriptions to minimize confusion and maximize clarity.
Presenting Your Understanding of the Clinical Trial
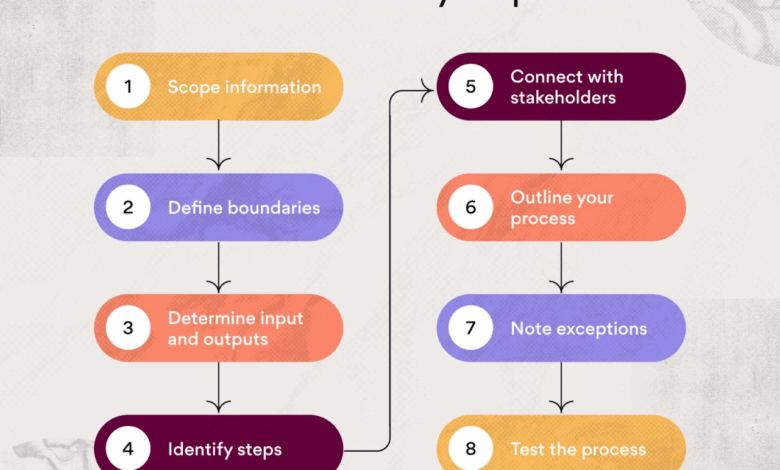
To showcase your comprehension of the clinical trial, a flow chart outlining the trial phases and key procedures is beneficial. The chart should clearly depict the study design, highlighting the roles of participants, the criteria for inclusion/exclusion, and the expected outcomes. This visual representation helps solidify your understanding and demonstrates your preparedness to the clinical trial research coordinator and doctor.
For instance, if the trial involves multiple steps or procedures, a flowchart can effectively illustrate the sequence and connections between them. This aids in conveying the intricacies of the clinical trial.
Last Word
In summary, thorough preparation is key for a productive clinical trial meeting. By understanding the meeting’s purpose, gathering essential information, and crafting a clear presentation, you can ensure a positive outcome. Remember to manage expectations, follow up promptly, and maintain accurate records. This comprehensive approach will empower you to effectively participate in these critical discussions and maximize their benefit.
