Is thermography a good way to detect breast cancer? This question delves into the potential of this non-invasive imaging technique. Thermography uses heat signatures to create images of the breasts, looking at blood flow patterns. Understanding its advantages, limitations, and comparison to other methods like mammograms is crucial to assessing its effectiveness in breast cancer detection.
This exploration will analyze the fundamental principles behind thermography, examining how it works and how images are interpreted. We’ll explore potential benefits like early detection and cost-effectiveness, alongside the limitations, such as its accuracy and potential for false positives. A comparison to established methods will provide a comprehensive understanding of thermography’s role in a broader breast cancer screening strategy.
Introduction to Thermography for Breast Cancer Detection
Thermography is a non-invasive diagnostic imaging technique used to assess breast health. Unlike mammography, which uses X-rays, thermography detects infrared heat emitted from the body. This approach can reveal subtle changes in blood flow and temperature patterns that may indicate underlying issues, including potential precancerous or cancerous conditions. While not a replacement for mammography, thermography can be a valuable complementary tool in the early detection of breast health problems.Thermography works by measuring the heat emitted from the body.
Variations in this heat, related to blood flow patterns, can highlight areas of potential concern. The technology measures minute temperature differences, which can be amplified and displayed as images. This allows medical professionals to identify areas with increased or decreased blood flow compared to surrounding tissue. These patterns can provide clues about potential issues, but further investigation is often necessary to confirm findings.
While thermography might seem like a promising breast cancer detection method, it’s important to remember that it’s not a reliable replacement for traditional screenings. Just like it’s a terrible idea for people to use pet prescription medication, treating health concerns with unproven methods can be risky. There are significant concerns regarding the accuracy and reliability of thermography for detecting breast cancer, so always consult with a healthcare professional for proper diagnosis.
People using pet prescription medication is a terrible idea. Ultimately, a thorough and accurate diagnosis is crucial for effective treatment, and thermography alone shouldn’t be relied upon for that.
Basic Principles of Thermography
Thermography relies on the principle that physiological changes, like increased blood flow, correlate with variations in temperature. Cancerous tissue, for example, often has an increased blood supply compared to healthy tissue. This difference in blood flow translates to temperature variations that can be visualized using specialized equipment. The instruments detect and measure these minute differences in temperature, then process the data into a thermographic image.
Image Generation and Interpretation
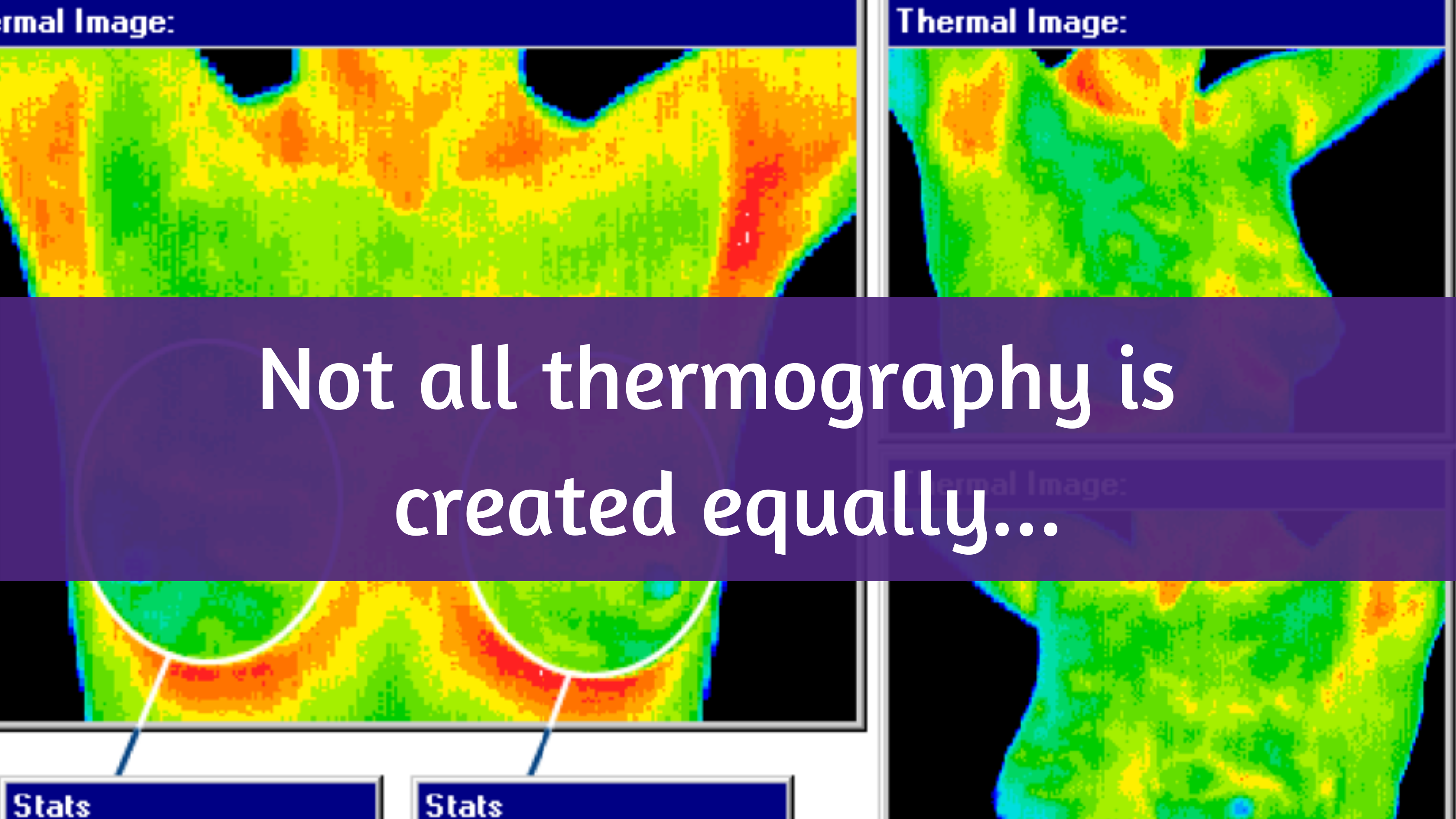
Thermography images are generated by specialized cameras that detect and measure infrared radiation emitted from the body. These cameras convert the detected infrared data into thermal images, displaying varying colors representing different temperatures. Warmer colors often signify areas of increased blood flow, while cooler colors might indicate reduced blood flow. The patterns and distribution of these colors are analyzed by trained professionals to identify potential anomalies.
Interpretation requires careful consideration of the patient’s medical history, including previous imaging results and symptoms, to assess the significance of observed patterns.
Comparison of Normal and Abnormal Breast Tissue
| Feature | Normal Breast Tissue | Abnormal Breast Tissue |
|---|---|---|
| Temperature | Generally consistent and uniform temperature distribution across the breast. | Potentially localized areas of higher or lower temperature compared to surrounding tissue, indicative of increased or decreased blood flow. |
| Blood Flow | Even distribution of blood flow across the breast. | Increased blood flow in specific regions, often associated with angiogenesis (new blood vessel formation), which may accompany tumors or inflammation. Reduced blood flow in certain areas can also be a sign of possible issues. |
| Pattern | Symmetrical, smooth, and consistent patterns across the breast. | Asymmetrical, irregular, or localized areas of abnormal patterns in blood flow or temperature distribution. Unusual branching patterns of blood vessels, or “vascularity,” are a potential indicator of abnormal activity. |
Thermography’s Potential Benefits
Thermography, a non-invasive imaging technique that measures heat patterns on the skin’s surface, shows promise as a potential tool for breast cancer detection. While it’s not a replacement for established methods like mammography, it offers unique advantages that could improve early detection and patient care. Understanding these benefits is crucial for evaluating thermography’s role in the broader landscape of breast cancer screening.Thermography’s ability to detect subtle changes in blood flow and tissue temperature could be a valuable addition to existing diagnostic methods.
It works by identifying variations in heat patterns that might correlate with the presence of tumors, often appearing as areas of increased or decreased temperature. This could potentially aid in the early detection of cancer, even before physical changes are noticeable.
Potential Advantages Compared to Other Methods
Thermography presents several potential advantages over traditional breast cancer screening methods, especially for certain patient populations. These advantages stem from its unique approach and characteristics.
- Non-invasive nature and repeated screenings:
- Thermography is a non-invasive procedure, requiring no needles or radiation exposure. This makes it suitable for repeated screenings without the potential health risks associated with radiation exposure. This repeated screening potential is particularly beneficial for women with a family history of breast cancer or those at higher risk.
- Cost-effectiveness:
- Thermography screenings are generally less expensive than mammography, making them more accessible to a wider range of individuals. This cost-effectiveness could contribute to increased screening rates, particularly in underserved communities. For example, in areas with limited access to mammography facilities, thermography could play a vital role in early detection.
Potential for Early Detection
Thermography’s ability to detect subtle changes in blood flow and temperature patterns holds the potential for early cancer detection. While it doesn’t replace established methods like mammography, it can act as a complementary screening tool. Studies suggest that certain patterns in thermal images may correlate with the presence of abnormal tissue, potentially enabling earlier intervention. This early detection could lead to more favorable treatment outcomes, as tumors identified at an early stage often have a higher chance of successful treatment.
Advantages for Specific Patient Populations
Thermography may offer particular advantages for certain patient populations, due to its non-invasive nature and relative cost-effectiveness.
While thermography is sometimes touted as a breast cancer detection method, it’s important to remember that it’s not a reliable replacement for traditional methods like mammograms. This is especially true when considering the complexities of managing diabetes, and how tools like the Fitbit can play a significant role in this. Learning more about how the Fitbit can be used for diabetes management can be really helpful for anyone interested in wearable tech for health tracking.
all about the fitbit with diabetes. Ultimately, thermography shouldn’t be seen as a primary screening tool for breast cancer, and a combination of approaches with your doctor is always best.
- Younger women:
- Younger women may find thermography to be a safer and more accessible option compared to mammography, as it does not involve radiation exposure. This is particularly important for women who are concerned about the potential long-term health effects of radiation exposure.
- Women with implants:
- For women with breast implants, mammography can sometimes be less effective due to the interference from the implants. Thermography can provide a potentially more accurate screening method for this patient group, as it is not affected by implants.
- Individuals with dense breast tissue:
- Dense breast tissue can make it challenging to detect abnormalities on a mammogram. Thermography may be a more suitable option for women with dense breast tissue, as it can potentially detect subtle changes in tissue temperature that may not be visible on a mammogram.
Limitations and Drawbacks of Thermography
Thermography, while offering a non-invasive and relatively affordable screening method, has limitations that significantly impact its effectiveness in detecting breast cancer. Understanding these limitations is crucial for accurately interpreting thermography results and avoiding misdiagnosis. A critical evaluation of the technology’s strengths and weaknesses is vital for patients and healthcare professionals alike.Thermography relies on detecting subtle temperature variations on the skin’s surface.
While these variations can sometimes indicate underlying physiological changes associated with cancer, they are not always specific to cancerous processes. This inherent ambiguity leads to a higher potential for false positives and negatives.
Factors Affecting Thermography Readings
Several factors can influence the accuracy of thermography readings, making it challenging to definitively identify breast cancer. Breast density, for instance, can significantly affect the quality of the image. Dense breast tissue can obscure subtle temperature changes, leading to difficulty in distinguishing between normal and abnormal patterns.
Examples of False Positives and Negatives
Thermography may produce false positives in cases where benign conditions, such as hormonal fluctuations, inflammation, or recent breast trauma, cause temperature changes that mimic those associated with malignancy. Conversely, some cancerous lesions might not exhibit discernible temperature variations, resulting in false negatives. A patient with a slow-growing or early-stage tumor may not show significant temperature changes that are detectable by thermography.
This can be particularly problematic in identifying early-stage breast cancer, which is often crucial for successful treatment.
Breast Density and Other Conditions
Breast density is a significant factor that impacts the accuracy of thermography. Dense breast tissue can obscure subtle temperature changes, hindering the ability to detect subtle variations associated with cancerous processes. Other conditions, such as infections, inflammation, or hormonal fluctuations, can also affect thermography readings, potentially leading to misinterpretations. For example, a patient experiencing mastitis (inflammation of the breast) might show temperature changes on a thermogram that could be misconstrued as indicative of cancer.
Need for Further Research and Development
Current research consistently emphasizes the need for further development and validation to enhance the accuracy and reliability of thermography for breast cancer detection. Comparative studies against established diagnostic methods, like mammography, are crucial to determine the true clinical value of thermography in this context.
Potential Risks and Disadvantages
Using thermography as the sole screening method for breast cancer carries inherent risks. It may not detect all cancers, leading to delayed diagnosis and potentially impacting treatment outcomes. Reliance on thermography might lead to unnecessary anxiety and further investigations if a false positive result is obtained. It’s important to acknowledge that thermography is not a replacement for established diagnostic procedures.
Comparison with Other Breast Cancer Detection Methods: Is Thermography A Good Way To Detect Breast Cancer
Thermography, while offering a unique perspective on breast health, isn’t a replacement for established diagnostic methods. Understanding its strengths and weaknesses in comparison to other techniques is crucial for a comprehensive approach to breast cancer screening. This comparison helps clarify the role each method plays in a preventative and diagnostic strategy.Thermography’s capabilities are best understood in the context of existing imaging technologies.
A balanced assessment of accuracy, cost, and accessibility is essential for tailoring a screening plan to individual needs.
While thermography is sometimes touted as a breast cancer detection method, it’s not a reliable replacement for traditional screenings. Recent research suggests that its accuracy is often debated, especially when compared to mammograms. Interestingly, scientists are still uncovering the fascinating biological reasons behind children’s seemingly endless energy, which you can explore in this insightful article about scientists explain why children never seem to get tired.
Ultimately, thermography’s role in breast cancer detection remains a topic of ongoing investigation and shouldn’t be considered a definitive solution.
Accuracy Comparison
The accuracy of a diagnostic test is typically measured by its sensitivity and specificity. Sensitivity indicates the test’s ability to correctly identify those with the condition (true positives), while specificity indicates the test’s ability to correctly identify those without the condition (true negatives). These metrics are crucial for determining a test’s reliability.
| Method | Sensitivity | Specificity | Cost | Accessibility |
|---|---|---|---|---|
| Thermography | Lower than other methods, often reported as 60-80%. Results can be influenced by factors like hormonal changes and other conditions. | Higher than other methods. Studies show a high specificity for differentiating between benign and malignant lesions, though not as high as mammography. | Generally lower than mammography, MRI, and ultrasound. | Generally more accessible than MRI due to lower equipment costs and potentially wider availability in some regions. |
| Mammography | High, typically around 80-90%. Detects dense breast tissue changes well. | High, typically around 90%. | Moderate cost, varying based on facility and insurance coverage. | Widespread availability, making it a common screening method. |
| Ultrasound | High, but may vary depending on the operator’s skill and the complexity of the breast tissue. | High, typically exceeding 90%. | Generally lower than MRI. | Commonly available, often integrated with mammography centers. |
| MRI | High, exceeding 90% in many cases, especially in dense breasts. | High, typically above 90%. | Highest cost among the four methods. | Limited accessibility due to the high cost of the equipment and potential need for contrast agents. |
Cost and Accessibility
The financial implications and availability of different methods significantly impact their suitability for a widespread screening program. Cost varies considerably, impacting access to specialized diagnostic tools. Accessibility is also a key factor, influencing the ease of scheduling appointments and receiving timely diagnoses.
Role in a Comprehensive Screening Strategy
Each method plays a distinct role in a comprehensive breast cancer screening strategy. Mammography remains the gold standard for breast cancer detection, particularly in women with a higher risk profile. Ultrasound is valuable for evaluating specific areas of concern identified by mammography or other methods, and MRI plays a critical role in evaluating dense breast tissue, aiding in the diagnosis of complex cases, or evaluating patients with a strong family history or genetic predisposition.
Thermography, with its lower cost and potential for early detection of abnormalities, might complement these methods in a tailored approach, especially for women who desire a less invasive, non-ionizing screening option. However, it’s essential to acknowledge that thermography’s accuracy is not as high as mammography, ultrasound, or MRI.
Current Research and Future Directions
Thermography’s journey toward reliable breast cancer detection is an ongoing process, marked by both promising advancements and critical areas requiring further investigation. While its limitations have been clearly established, the potential for enhancing its accuracy and expanding its applications remains a driving force in current research. Understanding the current state of research is crucial to assessing thermography’s true potential and its place alongside established imaging techniques.Current research efforts are primarily focused on refining thermography’s sensitivity and specificity, aiming to reduce false positives and improve its ability to identify subtle changes associated with breast cancer.
This involves advanced signal processing techniques, improved image acquisition protocols, and development of new algorithms to interpret thermal patterns more effectively. Researchers are continually exploring how to better distinguish between benign and malignant conditions, a key aspect of any diagnostic tool.
Current State of Research
The current research landscape on thermography’s effectiveness in breast cancer detection is characterized by a mix of ongoing studies and a persistent focus on improving the technology’s diagnostic capabilities. Researchers are investigating ways to enhance the quality and interpretation of thermal images. This involves exploring novel approaches to image processing and developing algorithms to improve the identification of subtle thermal patterns indicative of potential breast cancer.
Ongoing Studies and Clinical Trials
Several studies are investigating the potential of combining thermography with other imaging techniques, such as mammography and ultrasound. This combination approach aims to leverage the strengths of each modality to provide a more comprehensive evaluation of breast health. For example, some ongoing studies are examining the use of thermography as a screening tool to identify patients who might require further diagnostic testing, potentially reducing unnecessary biopsies.
Specific details on these ongoing trials are often restricted due to the evolving nature of research protocols.
Areas Needing Further Investigation
To truly validate thermography’s role in breast cancer detection, further research is needed in several critical areas. Standardization of imaging protocols and interpretation criteria is paramount to ensuring consistency and reproducibility of results across different settings. This includes establishing clear and objective guidelines for thermal pattern analysis to minimize inter-observer variability. Comparative studies directly comparing thermography’s performance against established methods are essential to demonstrate its added value in the diagnostic process.
Combining Thermography with Other Techniques
The potential for combining thermography with other imaging techniques holds considerable promise for enhancing accuracy. A multi-modal approach, utilizing thermography alongside mammography or ultrasound, could potentially increase the detection rate of subtle abnormalities, while minimizing the risk of false negatives or false positives. The integration of artificial intelligence (AI) algorithms to analyze thermal images could further refine interpretation and potentially improve the accuracy of breast cancer detection.
Potential Future Applications and Developments, Is thermography a good way to detect breast cancer
Future applications of thermography could involve its use in monitoring the response of breast cancer patients to treatment. Changes in thermal patterns could potentially indicate treatment effectiveness or the emergence of new tumors. The development of portable, affordable thermography devices could expand access to early detection screening in underserved populations. The application of machine learning algorithms could enable automated analysis of thermal images, reducing the time and workload for radiologists and improving diagnostic efficiency.
Early identification and monitoring of breast conditions are likely to be central in the future development of thermography, improving patient outcomes.
Patient Perspective and Experiences
Patients often view thermography as a convenient and non-invasive alternative to traditional breast cancer screening methods. This perception stems from the lack of physical contact and radiation exposure associated with the procedure. However, it’s crucial to understand that patient experiences and perceptions are shaped by varying levels of information and understanding about the technology’s limitations.Understanding the patient perspective is vital for accurately portraying thermography’s role in breast cancer detection.
It helps in navigating potential misconceptions and fostering informed decision-making. A nuanced view of patient experiences is crucial to provide accurate information and support their choices regarding breast health.
Patient Perceptions of Thermography
Patient perceptions of thermography are largely influenced by marketing materials and anecdotal accounts. Some patients perceive it as a “miracle cure” or a “natural” screening method. This perception can lead to unrealistic expectations and a sense of false security. This enthusiasm may be a result of the non-invasive nature of the procedure. However, it’s essential to emphasize that thermography is not a replacement for established diagnostic methods.
Patient Experiences with Thermography Screenings
Patients often report a comfortable and relatively quick screening experience with thermography. The procedure involves minimal discomfort, primarily from the application of a specialized camera to the breast area. However, the lack of physical contact may be perceived as less comprehensive than a physical exam. Some patients may experience anxiety related to the lack of immediate results, or an initial feeling of relief, which can be misleading.
Patient Concerns and Misconceptions
Patients may harbor misconceptions about thermography’s accuracy and diagnostic capabilities. A common concern is the perceived ability of thermography to detect cancer at very early stages, a claim that is not entirely accurate. Patients may also be unaware of the technology’s limitations in differentiating between benign and malignant conditions. Misconceptions can lead to delays in seeking appropriate medical care if they interpret the results incorrectly.
Another concern is the lack of standardization in training and interpretation of thermographic images.
Common Questions and Answers about Thermography
| Question | Answer |
|---|---|
| Is thermography a reliable method for detecting breast cancer? | Thermography is not a substitute for established breast cancer screening methods like mammograms and ultrasound. While it can detect heat patterns that might indicate abnormalities, it cannot definitively diagnose breast cancer. |
| How accurate is thermography in identifying early-stage breast cancer? | Thermography’s accuracy in detecting early-stage breast cancer is debated. While some studies show promising results, further research is needed to establish its reliability in this regard. |
| Can thermography differentiate between benign and malignant breast conditions? | Thermography alone cannot reliably differentiate between benign and malignant breast conditions. Additional diagnostic tests are often necessary to confirm a diagnosis. |
| What are the limitations of thermography? | Thermography’s limitations include its inability to detect very small tumors, its dependence on the operator’s expertise, and its sensitivity to factors such as hormonal fluctuations. |
Last Recap
In conclusion, while thermography shows promise in certain aspects, particularly for repeated screenings and potential cost-effectiveness, it’s not a replacement for established breast cancer detection methods. Its limitations, including accuracy issues and dependence on factors like breast density, need to be acknowledged. The current research and future directions in this field are promising, but more investigation is necessary to validate its role and potential for improving breast cancer outcomes.
Ultimately, a multi-faceted approach involving various diagnostic tools remains the best strategy for early detection and effective treatment.

