Many medical studies involving children never finished. This is a critical issue, as incomplete research hinders our understanding of child health and delays the development of effective treatments. Why do so many studies fall short of their goals? What are the ethical, financial, and logistical hurdles that prevent these vital investigations from reaching completion? We’ll delve into the reasons behind these unfinished studies, examining their impact on the field, and exploring potential solutions to ensure future success.
This article explores the complex issues surrounding incomplete pediatric medical studies. We’ll look at the reasons for these unfinished projects, the impact on research, and the challenges in managing and analyzing data from young participants. Ultimately, we’ll discuss potential solutions to improve the completion rates of these critical studies.
Reasons for Incomplete Studies
Incomplete medical studies involving children represent a significant challenge to advancing pediatric medicine. The ethical imperative to protect vulnerable populations, coupled with the complex nature of pediatric research, often necessitates adjustments or terminations of studies. Understanding the reasons behind these incomplete studies is crucial for improving research design and promoting responsible scientific practices.The termination of a study, while unfortunate, is sometimes unavoidable due to various factors.
These factors range from unforeseen ethical dilemmas to logistical and financial constraints. The following sections delve into the potential reasons for incomplete pediatric studies, examining the ethical considerations, challenges, and limitations that researchers face.
Potential Reasons for Study Termination
Several factors can contribute to the premature termination of medical studies involving children. These include unforeseen safety concerns, difficulties in recruitment, and budget constraints. Furthermore, ethical considerations and regulatory issues can also lead to the discontinuation of a study. These reasons are not mutually exclusive and often intertwine in complex ways.
It’s a real shame that so many medical studies involving children never see the finish line. It’s easy to get caught up in the daily grind of a quarantine beauty routine, like trying out new face masks or perfecting my skincare regimen. But the truth is, these seemingly trivial self-care activities are nothing compared to the importance of completing those crucial medical studies on child development and health.
I often wonder what discoveries we’re missing out on because of incomplete research. Beauty routine in quarantine might be a temporary escape, but the need for comprehensive child health research is a pressing concern. The unfinished studies highlight the critical need for funding and resources to ensure these projects are brought to a successful conclusion.
- Ethical Concerns: Ethical review boards, such as Institutional Review Boards (IRBs), play a critical role in ensuring the protection of children’s rights and welfare. If a study raises serious ethical concerns, including potential harm to participants, the IRB may recommend termination.
- Unforeseen Safety Issues: Unexpected adverse reactions in trial participants can lead to immediate study termination. For example, if a new drug causes a significant increase in side effects or an unexpected health complication, the study may be halted to prevent further harm. Data analysis of the initial stages of the trial might reveal an unexpected relationship between the treatment and negative outcomes, necessitating immediate action.
- Recruitment Difficulties: Studies often require a specific number of participants to achieve statistically significant results. If recruitment falls short of expectations, the study may become unfeasible and be terminated. For example, a study might target children with a rare genetic condition, making it challenging to assemble a sufficient sample size within the allocated time frame.
- Financial Limitations: The cost of conducting research, particularly pediatric research, can be substantial. Budget constraints, including funding shortages or unexpected expenses, can necessitate the cessation of a study. For example, escalating costs for equipment maintenance or unforeseen clinical complications might strain the available budget, ultimately leading to termination.
- Regulatory Issues: Government regulations and guidelines, particularly those concerning data privacy and safety, must be strictly adhered to during research involving children. Failure to comply with these regulations can lead to study termination. For instance, a study might be halted if it fails to adhere to stringent data handling procedures Artikeld by the relevant regulatory bodies.
Examples of Challenges in Pediatric Research
Medical studies involving children often face unique challenges that are not encountered in studies with adult populations. These challenges can stem from the inherent vulnerability of children, the complexities of pediatric conditions, and the need for meticulous ethical considerations.
- Complex Patient Populations: Pediatric patients present a diverse array of conditions, ages, and developmental stages. This heterogeneity can complicate the interpretation of results and require extensive stratification and control measures. For instance, a study evaluating the effectiveness of a new treatment for asthma in children might need to account for differences in severity of the condition, age, and co-existing illnesses.
- Longitudinal Studies: Longitudinal studies, which track participants over extended periods, are particularly challenging in pediatric research due to the inherent mobility of children and families, as well as the possibility of family dynamics changing.
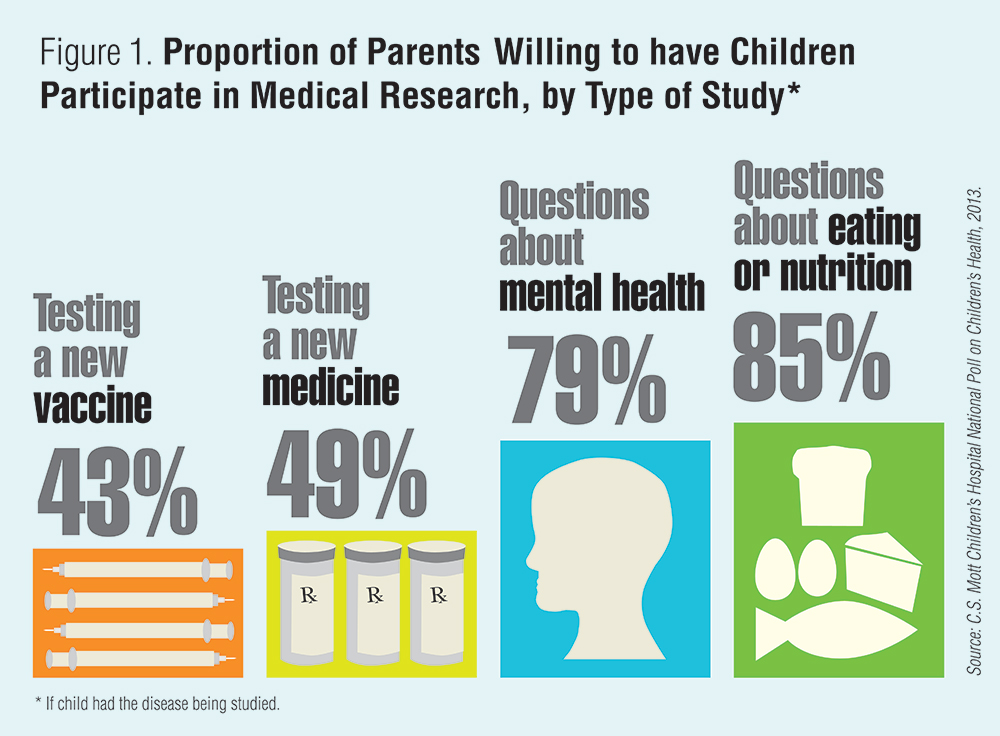
- Parental Consent and Assent: Obtaining informed consent from parents and assent from children, especially younger ones, can be a significant hurdle. Furthermore, ensuring consistent participation throughout the study can be a challenge.
Financial Limitations in Pediatric Research
Pediatric research often requires specialized equipment, skilled personnel, and extensive follow-up care, leading to considerable financial burdens. These costs can strain research budgets, potentially leading to the discontinuation of studies.
It’s a real shame that so many medical studies involving children never reach completion. Often, these unfinished studies leave huge gaps in our understanding of child health. This lack of conclusive data makes it hard to truly grasp the impact of various factors, and it’s a topic that’s frequently overlooked. For example, when looking at the nutritional value of foods like spinach dip, a key question arises: is spinach dip good for you?
This article delves into the potential benefits and drawbacks of this popular appetizer. Ultimately, the lack of finished studies on children is a significant concern, hindering our ability to provide the best possible care for the next generation.
- Specialized Equipment: Conducting pediatric research frequently demands specialized equipment and facilities, which can be expensive. For instance, a study on rare neurological disorders might necessitate access to advanced neuroimaging technology.
- Personnel Expertise: The need for experienced researchers, nurses, and other support staff with specialized pediatric knowledge can add significantly to the study’s financial demands.
- Long-Term Follow-up: Many pediatric studies require long-term follow-up to assess the long-term effects of interventions. These follow-up costs can significantly impact the feasibility of the study.
Role of Regulatory Bodies
Regulatory bodies, such as the FDA and ethical review boards, play a crucial role in overseeing and regulating pediatric research. These bodies ensure the safety and well-being of child participants.
- Review Processes: Regulatory bodies rigorously review research protocols to identify potential risks and ensure ethical considerations are adequately addressed. These reviews are essential to the success and integrity of child-focused studies.
- Compliance Requirements: Regulatory bodies impose strict compliance requirements for research involving children. These requirements include adherence to data privacy, safety guidelines, and informed consent procedures.
- Monitoring Procedures: Ongoing monitoring of study progress is crucial to ensure that ethical standards are maintained and that safety concerns are addressed promptly. This monitoring process is vital to the integrity of the study and the safety of participants.
Frequency of Study Termination Across Medical Fields
| Medical Field | Frequency of Study Termination (Estimated %) | Reasons (Summary) |
|---|---|---|
| Oncology | 15-20% | Safety concerns, recruitment difficulties, and financial constraints. |
| Cardiology | 10-15% | Ethical concerns, recruitment difficulties, and financial constraints. |
| Neurology | 12-18% | Safety concerns, logistical issues, and recruitment difficulties. |
| Developmental Pediatrics | 18-25% | Ethical concerns, recruitment difficulties, and logistical challenges. |
Note
The percentages are estimates and may vary depending on the specific study and the research context.
Solutions to Minimize Incomplete Studies
Strategies to reduce the number of incomplete studies involving children are essential for advancing pediatric medicine. These strategies encompass improving research design, enhancing collaboration, and increasing funding.
- Improved Research Design: Carefully designed studies with realistic timelines and clear outcome measures can reduce the risk of premature termination.
- Enhanced Collaboration: Interdisciplinary collaboration between researchers, clinicians, and regulatory bodies can improve study design, implementation, and ethical oversight.
- Increased Funding: Increased funding for pediatric research can address financial constraints and allow for more comprehensive and longer-term studies.
Impact of Incomplete Studies: Many Medical Studies Involving Children Never Finished
Incomplete medical studies involving children pose significant challenges to the advancement of child health. The absence of complete data hinders our understanding of crucial developmental stages, disease progression, and treatment efficacy, ultimately delaying the development of effective therapies. This impacts not only current patient care but also future generations.The incomplete nature of these studies often stems from various factors, including ethical considerations, logistical hurdles, and participant attrition.
Regardless of the reason, the consequences of missing data on child health outcomes are profound and multifaceted.
Consequences of Missing Data on Child Health Outcomes
The absence of complete data in child health studies significantly limits our ability to fully understand disease mechanisms and their impact on developmental trajectories. This lack of comprehensive information can result in inaccurate risk assessments, leading to potentially inappropriate interventions or delayed diagnoses. Missing data can also lead to a skewed understanding of the effectiveness of different treatments.
It’s a real shame that so many medical studies involving children never reach completion. Often, these studies are halted due to various factors, and it leaves a lot of unanswered questions. For example, a great resource for understanding the challenges of managing childhood diabetes is Brendan McEachern’s book, “Bolus Blues” bolus blues diabetes book brendan mceachern.
This underscores the need for more robust support systems and funding to ensure these crucial investigations are finished, providing valuable insights into pediatric health.
Impact on Treatment Recommendations for Children
Incomplete studies directly affect the evidence base for treatment recommendations. When data is incomplete or missing, it’s challenging to establish clear, reliable correlations between specific interventions and positive outcomes. This uncertainty can result in the adoption of treatments with questionable efficacy or the delayed implementation of effective therapies. Furthermore, the limited data often does not capture the diverse range of responses among children, hindering the personalization of treatment plans.
Potential Biases in Available Data Due to Incomplete Studies
Incomplete studies can introduce biases that skew the interpretation of results. For example, if a study enrolling children with specific characteristics is incomplete, the conclusions drawn might not be generalizable to the broader population of children. The lack of representation of certain demographic groups or specific disease presentations can also introduce selection bias, leading to inaccurate conclusions about treatment efficacy and safety.
Delays in the Development of Effective Treatments for Childhood Illnesses
The absence of complete data in medical studies can directly delay the development of effective treatments for childhood illnesses. This delay can have profound consequences for affected children and their families. The lack of conclusive evidence can lead to hesitation among healthcare professionals in implementing potentially beneficial therapies, further hindering progress in the field.
Examples of Diseases Hampered by Incomplete Studies, Many medical studies involving children never finished
Asthma, a prevalent childhood respiratory condition, exemplifies the challenges posed by incomplete studies. Incomplete studies can make it difficult to fully understand the interplay of environmental factors and genetic predispositions in asthma development. Similarly, studies on childhood cancers often lack the necessary long-term follow-up data to fully assess the long-term effects of treatment and the potential for recurrence.
Incomplete studies can result in treatment recommendations that are not entirely tailored to the unique needs of children with these diseases.
Types of Medical Studies Frequently Left Unfinished
- Longitudinal studies following children’s development over time are often challenging to complete due to factors such as participant attrition, financial constraints, and the need for long-term follow-up.
- Clinical trials involving rare childhood diseases often struggle to enroll a sufficient number of participants, which can limit the statistical power of the study and hinder the ability to draw definitive conclusions.
- Studies evaluating the long-term effects of specific treatments for chronic conditions like cystic fibrosis or sickle cell disease face challenges in maintaining long-term follow-up and data collection, potentially leading to incomplete datasets.
Impact on Confidence in Available Medical Information
Incomplete studies erode the confidence in the available medical information. When the data is incomplete or missing crucial elements, it creates uncertainty regarding the reliability of conclusions drawn from the study. This lack of confidence can lead to skepticism among healthcare professionals and the public, hindering the adoption of potentially beneficial treatments and preventive measures. The inconsistencies in data can also confuse patients and families, making informed decisions about their children’s health more challenging.
Data Management and Analysis Challenges
Collecting and analyzing data from pediatric participants presents unique challenges compared to adult studies. The developmental stages, varying levels of cooperation, and ethical considerations surrounding data collection and storage significantly impact the overall process. Maintaining long-term follow-up is particularly complex, demanding consistent engagement with families and navigating the dynamic nature of childhood.
Difficulties in Collecting and Managing Pediatric Data
Gathering data from children requires specialized techniques. Consent procedures must adhere to ethical guidelines for minors, often involving parental or guardian authorization. The complexity of data collection methods increases as children mature, demanding adaptability and flexibility. Recruitment strategies must target families and potentially involve community outreach programs. Furthermore, ensuring data security and privacy for children is paramount.
Data encryption and anonymization procedures are crucial to protect sensitive information.
Challenges in Maintaining Long-Term Follow-Up
Maintaining long-term follow-up in pediatric research is notoriously difficult. Children’s changing circumstances, such as moving, family transitions, or loss of contact, can disrupt data collection. Motivation and engagement can wane over time, necessitating creative strategies for retention. The natural progression of developmental stages can also influence the collection of data, necessitating the adaptation of data collection instruments.
Consequently, researchers need robust strategies for tracking and managing these changes.
Data Formats in Pediatric Studies
Numerous data formats are employed in pediatric studies. Structured electronic health records (EHRs) provide a valuable source of information. Questionnaires and surveys are frequently used, with various formats like Likert scales and open-ended questions. Observations and clinical assessments are also common, often recorded in standardized forms. Video recordings can provide detailed insights, but pose challenges in storage and analysis.
Data is frequently stored in databases, with specialized software supporting the management and analysis of pediatric-specific data.
Ensuring Data Quality and Consistency
Maintaining data quality and consistency is crucial in pediatric research. Standardized protocols for data collection and entry are essential. Regular data audits and quality checks can identify and rectify errors. Training researchers and data collectors on appropriate data entry techniques and adherence to ethical guidelines is paramount. Data validation procedures, such as cross-checking information, can minimize inconsistencies.
Utilizing data cleaning algorithms can enhance the accuracy and reliability of collected data.
Data Analysis Methods for Incomplete Datasets
Analyzing data from incomplete datasets requires specific methodologies.
| Data Analysis Method | Description | Suitability for Incomplete Data |
|---|---|---|
| Imputation | Substituting missing values with estimated ones | Potentially useful, but requires careful consideration of imputation methods |
| Multiple Imputation | Generating multiple imputed datasets | More robust than single imputation |
| Sensitivity Analysis | Assessing the impact of different assumptions on results | Essential to understand the potential influence of missing data |
| Listwise Deletion | Excluding cases with missing values | Simplest method, but can lead to significant loss of data |
| Pairwise Deletion | Using available data for each analysis | Can be less biased than listwise deletion |
Impact of Data Management Strategies on Study Completion Rates
Studies that incorporate robust data management strategies, including standardized data collection tools, clear data entry protocols, and effective data storage methods, tend to have higher study completion rates. Strategies that proactively address potential drop-outs, such as providing incentives or maintaining ongoing communication with families, are also critical. This ensures the collection of comprehensive and reliable data, leading to stronger research outcomes.
Visual Representation of Data Management in Pediatric Research
Imagine a complex network diagram. At the center is a child, representing the study subject. Connecting to the child are multiple branches representing various data collection methods (questionnaires, clinical assessments, etc.). These branches lead to a central hub representing data storage and management. From this hub, other branches extend to different analysis methods (statistical software, databases, etc.).
A final set of branches depicts the output of the research, including reports, publications, and insights gained from the study. This network highlights the interconnected nature of each step in the process and the importance of each component for successful completion.
Addressing the Issue of Incomplete Studies
Incomplete pediatric medical studies pose significant challenges, hindering the advancement of knowledge and the development of effective treatments for childhood illnesses. These unfinished investigations represent a lost opportunity to learn crucial information about diseases and their management in children, a vulnerable population with unique physiological and developmental factors. The reasons for incompletion vary, from logistical difficulties to ethical considerations, and the consequences are far-reaching, potentially delaying crucial discoveries.Addressing the issue of incomplete pediatric studies requires a multifaceted approach, encompassing improvements in study design, recruitment strategies, and ethical considerations.
Strategies must be developed to not only increase completion rates but also foster long-term engagement in research. This comprehensive effort aims to ensure the integrity and value of pediatric research.
Improving Completion Rates
Strategies to enhance completion rates in pediatric studies necessitate a proactive approach. One key element involves refining study protocols to minimize burden on families and researchers. This could include streamlining consent procedures, reducing the frequency of visits, and using innovative technologies to collect data remotely. Furthermore, clear communication with families throughout the study is paramount. Regular updates and clear explanations of the study’s purpose and procedures can enhance understanding and trust.
Innovative Approaches for Long-Term Participation
Encouraging long-term participation in pediatric research requires innovative approaches that acknowledge the unique circumstances of childhood. Building strong relationships with families and fostering trust are essential. This involves creating a supportive environment where families feel comfortable raising questions and concerns. Furthermore, offering incentives that are meaningful to families, such as educational resources, access to healthcare professionals, or financial assistance, can motivate participation over extended periods.
Parental Consent and Communication
Parental consent is critical in pediatric research. Comprehensive and accessible information about the study, presented in an easily understandable manner, is crucial for informed consent. Clear communication about the study’s procedures, risks, and benefits is vital. This includes regular updates on the child’s progress and any changes in the study protocol. Transparent communication fosters trust and understanding, leading to increased participation and study completion.
Resources and Infrastructure
Adequate resources and infrastructure are essential for successful pediatric research. This includes dedicated research personnel, well-equipped facilities, and robust data management systems. Furthermore, training programs for researchers, focusing on the unique challenges of pediatric studies, are crucial for ensuring the quality and integrity of the research process. Investment in these areas directly impacts the completion rate of studies and the quality of the data collected.
Ethical Review Boards
Ethical review boards play a vital role in ensuring the integrity of pediatric research. These boards critically evaluate study protocols to protect the rights and welfare of the children involved. Their rigorous review process helps to mitigate potential risks and ensure that studies adhere to the highest ethical standards. Furthermore, active engagement of families in the review process can foster trust and encourage participation.
Incentives and Support Systems
| Incentive Category | Examples |
|---|---|
| Financial Support | Gift cards, stipends, transportation assistance |
| Healthcare Services | Access to specialist consultations, follow-up care |
| Educational Resources | Workshops, educational materials for parents |
| Community Support | Networking opportunities with other families involved in research |
Process Flow Diagram
(A visual diagram illustrating the steps involved in addressing incomplete studies would be displayed here. It would include stages such as protocol refinement, recruitment strategies, communication plans, resource allocation, ethical review, and data management. This would be a flow chart that visualizes the steps in a sequential manner, enabling quick comprehension of the procedure.)
Global Perspectives
Incomplete pediatric studies pose a significant global challenge, hindering the advancement of medical knowledge and potentially impacting the well-being of children worldwide. Understanding the varying completion rates across different regions is crucial to identifying the root causes and implementing effective strategies for improvement. This analysis will explore the global variations in study completion, comparing successes and challenges, and examining the crucial role of international collaborations and resource allocation in promoting pediatric research.Global variations in pediatric study completion rates are substantial, influenced by a complex interplay of factors.
Completion rates are not uniform, and different regions face unique challenges that affect the success of these critical research endeavors. Understanding these regional disparities is vital to addressing the global gap in pediatric research data.
Regional Variations in Study Completion Rates
Different countries and regions exhibit varying completion rates for medical studies involving children. These discrepancies are often rooted in diverse socio-cultural contexts, resource limitations, and regulatory frameworks. Variations in infrastructure, research capacity, and ethical considerations further contribute to these differences. The completion rates are often lower in regions with limited resources, less robust research infrastructure, and stricter ethical guidelines, which can influence the feasibility and sustainability of pediatric studies.
Challenges and Successes in Different Regions
The challenges faced in different regions vary. In some regions, logistical difficulties, such as obtaining informed consent from parents, may hinder study progress. In other regions, limited access to specialized pediatric expertise or advanced technologies could be a significant obstacle. Successes, however, highlight potential strategies for improvement. Some countries have demonstrated successful collaborations, streamlined regulatory processes, and robust ethical review systems.
These examples can be instrumental in improving completion rates in other regions. For instance, the successful completion of a study on the prevalence of malnutrition in South Asia could inform similar studies in other parts of the developing world.
Cultural and Societal Factors Influencing Completion
Cultural and societal norms significantly impact the completion of pediatric studies. These norms influence parental consent rates, willingness to participate, and adherence to study protocols. Cultural sensitivity and tailored communication strategies are essential for ensuring ethical and effective participation. For example, culturally appropriate language and methods for explaining the study’s purpose and procedures are crucial in gaining parental trust and informed consent.
Impact of Resource Allocation on Completion Rates
Adequate funding and resources are critical for the successful completion of pediatric studies. Inadequate funding can lead to delays, difficulties in recruitment, and ultimately, incomplete data sets. A lack of funding for infrastructure, research personnel, and essential equipment can impede progress. For example, a study investigating the effectiveness of a new treatment for childhood asthma in a low-income country might be significantly impacted by a lack of access to necessary equipment for accurate data collection.
Examples of International Collaborations
International collaborations can overcome regional limitations and contribute to more robust and comprehensive pediatric research. These collaborations bring together expertise, resources, and perspectives from different countries, resulting in more impactful findings. For example, the Global Initiative on Asthma (GINA) is a prominent international collaboration that promotes evidence-based guidelines and research on childhood asthma globally.
Role of International Organizations
International organizations play a crucial role in promoting and supporting pediatric research. These organizations often provide funding, training, and technical assistance to researchers in developing countries. The World Health Organization (WHO) plays a significant role in coordinating global efforts to improve child health through research and evidence-based interventions.
Summary Table of Key Factors Affecting Study Completion Rates
| Region | Key Factors Affecting Completion | Challenges | Successes |
|---|---|---|---|
| Developed Countries | Strong research infrastructure, adequate funding, established ethical guidelines | Maintaining participant recruitment, ensuring data quality | High completion rates, robust data sets |
| Developing Countries | Limited resources, infrastructure challenges, cultural considerations | Obtaining informed consent, data collection logistics, ensuring participant safety | International collaborations, capacity building programs |
Final Conclusion
The issue of incomplete medical studies involving children is a multifaceted problem, demanding a comprehensive approach. From ethical considerations to logistical challenges and data management issues, many factors contribute to the discontinuation of these projects. Addressing these issues requires a collective effort involving researchers, policymakers, and families. Improved communication, enhanced resources, and a focus on ethical practices are crucial to ensuring that future pediatric research reaches its full potential and benefits children’s health worldwide.
By working together, we can ensure that valuable data is collected and utilized to improve the lives of children.