Toxicity in rheumatoid arthritis medications is a critical concern for patients and healthcare professionals alike. This in-depth exploration delves into the various aspects of medication-related side effects, from understanding the different types of RA medications and their mechanisms of action to identifying specific adverse effects and monitoring strategies. We’ll also examine the mechanisms of toxicity, patient education, research advancements, and illustrative case studies, ultimately offering a comprehensive overview for better management and treatment.
Rheumatoid arthritis (RA) affects millions worldwide, demanding effective treatment. Various medications, including disease-modifying antirheumatic drugs (DMARDs) and biologics, are crucial in managing RA symptoms. However, these medications can sometimes lead to significant side effects, which we will carefully examine, considering individual factors and risk profiles. A critical understanding of potential toxicity is essential for optimizing treatment outcomes and minimizing harm.
Introduction to Rheumatoid Arthritis Medications
Rheumatoid arthritis (RA) is a chronic autoimmune disease that primarily affects the joints, causing inflammation, pain, and stiffness. Over time, this inflammation can lead to joint damage and disability if left untreated. Effective management of RA hinges on a multifaceted approach, with medication playing a crucial role in controlling the disease’s progression and improving patients’ quality of life.
This approach involves various classes of drugs targeting different aspects of the disease process.The goal of RA treatment is to reduce inflammation, prevent joint damage, and alleviate symptoms. Medications play a central role in achieving these goals, and the choice of medication often depends on the severity of the disease, the patient’s response, and potential side effects. Understanding the different types of RA medications and their mechanisms of action is key for patients and healthcare providers to make informed decisions about treatment strategies.
Common Types of Rheumatoid Arthritis Medications
RA medications are categorized into several classes, each with its own mechanism of action and potential side effects. Commonly used medications include disease-modifying antirheumatic drugs (DMARDs), corticosteroids, and biologics. These medications work by targeting different components of the immune system and inflammatory pathways involved in RA.
Disease-Modifying Anti-Rheumatic Drugs (DMARDs)
DMARDs are foundational medications in RA treatment. They aim to modify the disease’s progression by suppressing the immune response and reducing inflammation. Methotrexate, a frequently prescribed DMARD, is a cornerstone of RA treatment, often used in combination with other medications. Other examples include sulfasalazine, hydroxychloroquine, and leflunomide.
- Methotrexate is often the first-line DMARD due to its effectiveness in slowing disease progression and reducing joint damage.
- Leflunomide is an immunosuppressant that works by inhibiting the production of certain immune cells.
- Sulfasalazine is an anti-inflammatory drug with a mechanism of action that is still being fully researched, but it is thought to interfere with the immune system’s inflammatory response.
- Hydroxychloroquine reduces inflammation by altering immune cell function.
Biologics
Biologics are a newer class of RA medications that target specific proteins and pathways involved in the immune response. They are often used when DMARDs are not sufficient to control the disease. Examples include TNF inhibitors (e.g., adalimumab, etanercept), interleukin-6 inhibitors (e.g., tocilizumab), and B-cell inhibitors (e.g., rituximab).
- TNF inhibitors (e.g., adalimumab, etanercept) work by blocking tumor necrosis factor-alpha (TNF-α), a protein that plays a key role in inflammation.
- Interleukin-6 inhibitors (e.g., tocilizumab) target interleukin-6 (IL-6), a cytokine that contributes to inflammation.
- B-cell inhibitors (e.g., rituximab) target B cells, a type of immune cell that produces antibodies.
Corticosteroids
Corticosteroids are potent anti-inflammatory drugs that can quickly reduce inflammation in RA. They are often used in conjunction with other medications to manage flares or acute symptoms. Common examples include prednisone and methylprednisolone.
Potential Side Effects of RA Medications
All RA medications, regardless of class, have the potential for side effects. These side effects can range from mild to severe and may vary depending on the specific medication and the individual patient. It’s crucial for patients to discuss potential side effects with their healthcare provider and report any concerning symptoms promptly. Careful monitoring and adjustments to the treatment plan are often necessary.
Comparison of RA Medication Classes
| Medication Class | Examples | Mechanism of Action | Potential Side Effects |
|---|---|---|---|
| DMARDs | Methotrexate, Leflunomide, Sulfasalazine, Hydroxychloroquine | Modify disease progression, suppress immune response | Gastrointestinal upset, liver problems, bone marrow suppression |
| Biologics | Adalimumab, Etanercept, Tocilizumab, Rituximab | Target specific proteins/pathways in the immune response | Increased risk of infections, allergic reactions, injection site reactions |
| Corticosteroids | Prednisone, Methylprednisolone | Potent anti-inflammatory | Osteoporosis, weight gain, increased risk of infections |
Identifying Potential Toxicity
Understanding the potential side effects of rheumatoid arthritis (RA) medications is crucial for both patients and healthcare providers. This knowledge empowers informed decision-making regarding treatment choices and allows for proactive management of potential complications. Careful monitoring and communication between patients and their doctors are key to minimizing the risks associated with these medications.
Adverse Effects Linked to Different RA Medications
Various RA medications target different inflammatory pathways and have unique side effect profiles. For instance, disease-modifying antirheumatic drugs (DMARDs) like methotrexate can cause gastrointestinal upset, liver damage, and bone marrow suppression. Biologics, while often effective, can potentially lead to infections, allergic reactions, and certain types of cancers. These examples highlight the importance of individualized treatment plans and ongoing monitoring.
Potential for Long-Term Toxicity in Various RA Medication Classes
Long-term use of RA medications can sometimes lead to cumulative adverse effects. For example, prolonged corticosteroid use can result in osteoporosis, cataracts, and adrenal insufficiency. Certain DMARDs, if not properly monitored, might contribute to organ damage over time. It’s important to emphasize that these potential risks are not inevitable and are often mitigated through careful dose adjustments and regular monitoring.
Frequency and Severity of Side Effects
The frequency and severity of side effects vary considerably between different RA medications. The following table provides a general overview, but it’s crucial to remember that individual responses differ significantly. This table is not exhaustive, and specific side effects can vary based on individual patient factors.
| Drug Category | Common Side Effects | Potentially Serious Side Effects | Frequency (General) | Severity (General) |
|---|---|---|---|---|
| NSAIDs | Gastrointestinal upset, headache, dizziness | Kidney problems, heart problems, stomach ulcers | Frequent | Variable |
| DMARDs (Methotrexate) | Nausea, fatigue, mouth sores | Liver damage, bone marrow suppression, lung problems | Variable | Variable |
| Biologics | Injection site reactions, infections | Serious infections, allergic reactions, certain cancers | Variable | Variable |
| Corticosteroids | Weight gain, mood changes, insomnia | Osteoporosis, cataracts, adrenal insufficiency | Frequent | Variable |
Note: Frequency and severity are general estimations and can vary widely based on individual factors. Always consult with your physician for personalized advice.
Factors Increasing Risk of Medication Toxicity, Toxicity in rheumatoid arthritis medications
Several factors can increase the risk of medication toxicity in RA patients. These include pre-existing medical conditions, such as kidney or liver disease, and concurrent use of other medications. Age, genetic predisposition, and adherence to treatment protocols can also play a role. For example, a patient with pre-existing liver issues might be more susceptible to liver damage from methotrexate.
Comparing Risk Profiles of Different RA Medication Classes
Different RA medication classes carry distinct risk profiles. Corticosteroids, while potent in reducing inflammation, carry a high risk of long-term side effects. Biologics, while often very effective, have a risk of infections. DMARDs, while generally considered safe, can still cause significant adverse effects if not closely monitored. Ultimately, the optimal choice of medication requires careful consideration of individual patient needs and risk factors.
Mechanisms of Toxicity in RA Medications
Understanding the mechanisms behind the adverse effects of rheumatoid arthritis (RA) medications is crucial for safe and effective treatment. These mechanisms, often complex and multifaceted, involve interactions with various physiological pathways. Knowing how medications work, both their intended and unintended consequences, empowers both patients and healthcare providers to make informed decisions.
Physiological Pathways Affected by RA Medications
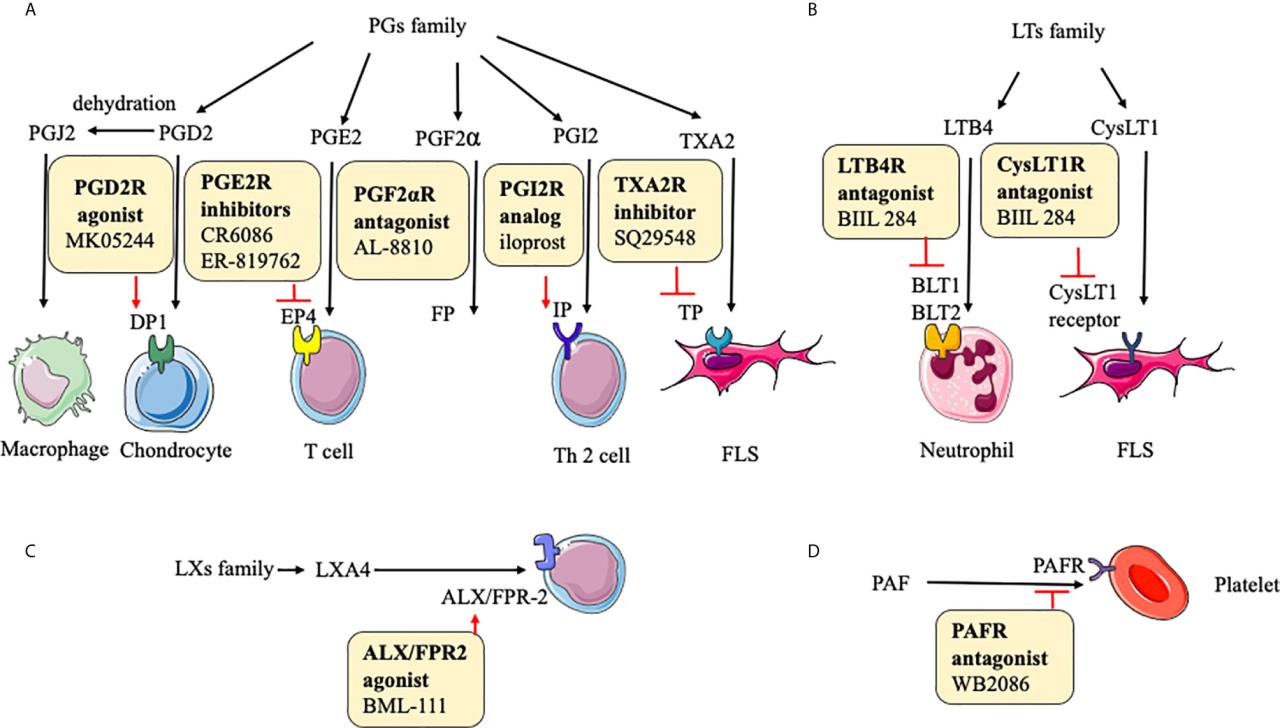
RA medications target different aspects of the immune system to control inflammation and slow disease progression. However, this targeted approach can lead to unintended consequences. These effects often arise from interactions with various physiological pathways, including those involved in cell signaling, metabolism, and even the cardiovascular system. Different classes of medications have varying mechanisms of action, which in turn dictate the specific pathways they influence.
Medication Dosage and Toxicity
The relationship between medication dosage and toxicity is a crucial factor in RA management. Generally, higher dosages increase the risk of adverse effects. This is due to the amplified impact on the targeted pathways and the potential for greater disruption in other systems. It is important to understand that the optimal dosage varies considerably between individuals. Factors like body weight, organ function, and concurrent conditions play a significant role in determining appropriate dosages.
Individual Patient Factors in Medication Response and Toxicity
Individual patient factors greatly influence how an RA patient responds to medication and their susceptibility to toxicity. Genetic variations can impact drug metabolism and the body’s response to the medication’s effects. Pre-existing conditions, such as kidney or liver impairment, can affect how the body processes the medication, potentially leading to higher concentrations and increased risk of toxicity. Nutritional status, including vitamin and mineral intake, also plays a role in medication efficacy and side effects.
For example, patients with compromised liver function may require lower doses of medications metabolized by the liver.
Drug Interactions in RA Patients
Drug interactions are a significant concern in RA patients. Concurrent use of other medications, including over-the-counter drugs, supplements, and even certain foods, can alter the metabolism or efficacy of RA medications. For instance, some medications can inhibit the enzymes responsible for breaking down other drugs, leading to elevated levels of the latter and potentially dangerous side effects. It’s essential for patients to disclose all medications, supplements, and herbal remedies to their healthcare providers to avoid potential interactions.
This meticulous documentation allows for informed adjustments to treatment plans, preventing adverse events. Examples include interactions between nonsteroidal anti-inflammatory drugs (NSAIDs) and some RA medications, which can increase the risk of gastrointestinal complications.
Examples of Toxicity Mechanisms
- Immunosuppressants: These medications can suppress the immune system, increasing susceptibility to infections. This is a direct consequence of the intended action of the medication. The risk of infection is directly correlated to the degree of immunosuppression. For instance, patients taking high doses of methotrexate may experience increased susceptibility to opportunistic infections.
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): NSAIDs, commonly used to alleviate pain and inflammation, can cause gastrointestinal issues, such as ulcers and bleeding. This toxicity stems from the inhibition of cyclooxygenase (COX) enzymes, which are crucial for the production of protective prostaglandins in the stomach lining. The inhibition disrupts the balance and can lead to mucosal damage.
Factors Influencing Toxicity
- Age: Older adults often have decreased kidney and liver function, affecting drug clearance and increasing the risk of toxicity. Therefore, appropriate dose adjustments may be necessary based on age-related physiological changes.
- Renal function: Patients with impaired kidney function may require dose reductions for medications that are primarily eliminated through the kidneys. Kidney function tests are crucial to monitor drug levels and adjust dosages as needed.
- Liver function: Medications metabolized by the liver require adjustments in dosage based on liver function tests. Liver dysfunction can result in elevated medication levels, leading to toxicity.
Monitoring and Management of Toxicity
Managing the potential side effects of rheumatoid arthritis (RA) medications is crucial for patient well-being. Careful monitoring and prompt adjustments to treatment plans can significantly mitigate harm and maintain therapeutic efficacy. A proactive approach, involving regular assessments and adaptable strategies, is key to ensuring patients receive the most effective and safest RA medication regimens.Monitoring toxicity in RA medications requires a multi-faceted approach, encompassing not just blood tests but also careful observation of symptoms and overall patient response.
Navigating the side effects of rheumatoid arthritis medications can be tough, especially when you’re juggling everything else life throws your way. It’s easy to feel overwhelmed by the potential toxicity, but amidst the challenges, the unwavering beauty of motherhood shines through, just like in what makes motherhood beautiful. Ultimately, though, the focus needs to remain on managing the toxicity of these medications effectively to maintain overall well-being.
This multifaceted approach allows for early detection of adverse effects, enabling timely interventions to prevent severe complications and maintain treatment efficacy.
Monitoring Strategies for RA Medication Toxicity
Effective monitoring strategies for RA medication toxicity are designed to detect adverse effects early and intervene appropriately. This allows for adjustments in medication dosages or the potential for switching to alternative treatments. A proactive approach to monitoring ensures patients receive the most beneficial and safest RA medication regimen.
Importance of Regular Blood Tests
Regular blood tests are essential for assessing the impact of RA medications on various organ systems. These tests provide valuable insights into potential toxicity, allowing healthcare professionals to adjust dosages or treatments as needed. Comprehensive blood work provides critical data for early detection and intervention in case of developing toxicity.
- Complete blood count (CBC): Monitors for changes in red blood cells, white blood cells, and platelets, crucial indicators of bone marrow function and potential anemia or infection.
- Liver function tests (LFTs): Assess liver health, which can be affected by certain RA medications. Regular monitoring helps identify potential liver damage early.
- Kidney function tests (KFTs): Evaluate kidney function, another organ system susceptible to drug-induced damage. These tests are vital to identify potential nephrotoxicity.
- Creatinine and blood urea nitrogen (BUN): These markers help assess kidney function, providing additional insights beyond KFTs. Monitoring these markers helps prevent further damage.
Adjusting Dosages Based on Toxicity Monitoring Results
Adjusting dosages based on toxicity monitoring results is a critical aspect of patient management. This tailored approach allows for optimized treatment efficacy while minimizing potential harm. The goal is to achieve the desired therapeutic effect with the lowest possible risk of side effects.
- Medication dose reductions: If toxicity is detected, the medication dosage can be lowered to reduce the risk of further adverse effects. The goal is to maintain efficacy while minimizing harm.
- Medication discontinuation: In severe cases, the medication might need to be discontinued. This decision should be made carefully, considering the benefits and risks for each individual patient.
- Switching to alternative medications: If a particular medication is causing toxicity, switching to an alternative with a lower risk of adverse effects can be an option. This approach requires careful consideration of the potential benefits and risks of different medications.
Strategies for Managing Adverse Effects and Minimizing Harm
Managing adverse effects and minimizing harm requires a multifaceted approach, encompassing symptom management, supportive care, and communication with healthcare providers. This holistic approach to patient care is vital to ensure optimal treatment outcomes.
- Symptom management: Strategies for managing specific symptoms (e.g., nausea, fatigue, gastrointestinal issues) can involve medications, dietary adjustments, or lifestyle modifications.
- Supportive care: Providing supportive care, such as nutritional counseling or physical therapy, can help patients cope with the challenges of RA and its treatment.
- Communication: Open and honest communication between patients and healthcare providers is crucial for identifying and managing potential toxicity. This involves discussing any concerns or symptoms promptly.
Specific Tests and Their Frequency
| Medication Category | Specific Tests | Frequency |
|---|---|---|
| Disease-modifying antirheumatic drugs (DMARDs) | CBC, LFTs, KFTs, Creatinine, BUN | Every 2-4 weeks initially, then as clinically indicated |
| Biologics | CBC, LFTs, KFTs, Creatinine, BUN, specific tests for potential infections (e.g., TB testing) | Every 4-8 weeks initially, then as clinically indicated |
| Corticosteroids | CBC, LFTs, KFTs, Glucose | Every 2-4 weeks initially, then as clinically indicated |
Patient Education and Awareness
Empowering rheumatoid arthritis (RA) patients with knowledge about their medications is crucial for managing the disease effectively. Understanding potential side effects and actively participating in their care leads to better outcomes and improved quality of life. This proactive approach fosters a strong patient-provider relationship, essential for successful treatment strategies.
Importance of Patient Education
Comprehensive patient education about medication toxicity is vital. Educated patients are better equipped to recognize and report potential side effects, enabling timely intervention and adjustments to treatment plans. This proactive approach can prevent severe complications and maintain optimal health. Patients become active partners in their healthcare journey, leading to more effective management of their RA.
Educational Materials for Patients
Providing accessible and user-friendly educational materials is key to patient understanding. These materials should be tailored to different learning styles and include clear explanations of potential side effects, symptoms to watch for, and strategies for managing them. Examples of educational materials include:
- Fact sheets and brochures: These materials can provide concise summaries of common side effects, their potential causes, and steps to take if they occur.
- Videos and online resources: Short, engaging videos and interactive online tools can make complex information more accessible and easier to understand. Animated sequences demonstrating how medications work can also be beneficial.
- Patient handbooks and medication guides: Comprehensive handbooks with detailed information on individual medications, including potential side effects, can help patients stay informed.
- Personalized medication checklists: These tools can assist patients in tracking their medications, side effects, and any adjustments made to their treatment plans.
Key Information for Patients
Clear communication of potential side effects is paramount. A well-organized table outlining potential side effects, their frequency, and management strategies can be invaluable for patients.
| Potential Side Effect | Frequency | Description | Management Strategies |
|---|---|---|---|
| Gastrointestinal upset (e.g., nausea, vomiting, diarrhea) | Common | Discomfort in the stomach or intestines | Take medication with food, adjust dosage, or seek medical advice. |
| Headache | Common | Pain in the head | Use over-the-counter pain relievers, manage stress, and contact doctor if severe. |
| Skin rash | Less common | Changes in skin appearance | Monitor for worsening rash; seek medical advice immediately if rash is severe or accompanied by other symptoms. |
| Fatigue | Common | Persistent tiredness | Prioritize rest, maintain a healthy lifestyle, and discuss with doctor. |
| Elevated liver enzymes | Rare | Abnormal liver function | Regular blood tests and monitoring; discuss with doctor if levels are elevated. |
Open Communication Between Patients and Healthcare Providers
Open communication between patients and healthcare providers is essential for managing potential side effects. Patients should feel comfortable discussing any concerns or side effects they experience with their doctor or other healthcare team members. Regular check-ups and open dialogue can ensure the best possible treatment plan.
Role of Patient Support Groups
Patient support groups can provide invaluable resources for patients managing medication toxicity. These groups offer a platform for sharing experiences, coping strategies, and support from peers who understand the challenges of living with RA. Support groups can be a source of strength and encouragement, and they can help to reduce feelings of isolation and promote better self-management.
Research and Future Directions
The quest to refine rheumatoid arthritis (RA) medication strategies and minimize toxicity is an active area of ongoing research. Scientists are exploring new approaches to drug design, delivery, and monitoring to ensure patients receive effective treatment while experiencing fewer side effects. This involves understanding the complex mechanisms of toxicity and developing innovative solutions to manage them.Researchers are actively investigating the potential of personalized medicine approaches, tailoring therapies to individual patient characteristics to optimize efficacy and minimize adverse reactions.
This approach acknowledges the variability in how individuals respond to RA medications and aims to predict and prevent toxicity based on a patient’s unique genetic makeup and other factors.
Ongoing Research into RA Medication Toxicity
Extensive research is underway to identify the specific molecular pathways and mechanisms responsible for the diverse range of toxicities associated with various RA medications. This includes studies analyzing how drugs interact with different cell types and organs, revealing the underlying reasons behind adverse events. Understanding these mechanisms is critical for developing targeted strategies to mitigate these effects. Researchers are also examining the long-term consequences of RA medications, exploring the potential for late-onset or cumulative toxicity.
New Approaches to Mitigating Toxicity
Several novel approaches are being explored to reduce the toxic effects of RA medications. One prominent area of research involves developing new drug formulations, aiming to improve drug bioavailability and reduce the concentration of active compounds reaching non-target tissues. Researchers are also investigating methods to enhance drug metabolism and excretion, preventing accumulation and potential damage to healthy organs.
Another approach involves identifying specific biomarkers that predict individual susceptibility to medication toxicity.
Innovative Therapies and Strategies
Emerging therapies are showing promise in reducing toxicity while maintaining efficacy. Biologic response modifiers, for instance, offer a more targeted approach to RA treatment, potentially reducing the risk of systemic side effects seen with traditional disease-modifying antirheumatic drugs (DMARDs). Additionally, researchers are exploring the use of combination therapies to achieve better disease control with lower individual drug doses.
This approach has the potential to minimize toxicity by reducing the overall drug load while maintaining effectiveness.
Emerging Technologies in Monitoring and Managing Medication Toxicity
Advancements in technology are transforming how RA medication toxicity is monitored and managed. Real-time monitoring systems and wearable sensors can continuously track key physiological parameters, enabling early detection of potential adverse reactions. This continuous data collection offers valuable insights into individual responses to treatment and allows for timely adjustments to medication regimens. Furthermore, sophisticated computational models are being developed to predict and simulate drug-induced toxicity in individual patients, helping clinicians make more informed treatment decisions.
Research Areas Requiring Further Investigation
- Personalized medicine approaches: Developing individualized treatment strategies based on genetic and other patient-specific factors is crucial. This includes identifying specific genetic markers that predict susceptibility to toxicity and designing personalized dosing regimens to minimize risk.
- Early detection and prevention of toxicity: Establishing reliable and sensitive biomarkers for early detection of toxicity is essential. This includes developing non-invasive diagnostic tools that can identify subtle changes in organ function indicative of toxicity. Proactive monitoring and preventive strategies can be implemented once potential toxicity is identified.
- Combination therapies for optimized efficacy and reduced toxicity: Exploring novel combination therapies that achieve optimal disease control with reduced individual drug doses is a key research area. This approach can maximize efficacy while minimizing potential adverse effects.
- Drug delivery systems: Developing targeted drug delivery systems that minimize exposure of non-target tissues to medication can reduce toxicity. This includes the exploration of nanoparticles and liposomes to deliver medications directly to affected areas.
- Long-term effects of RA medications: Investigating the long-term consequences of RA medications is crucial for understanding potential cumulative or late-onset toxicity. This includes longitudinal studies following patients on RA medications over extended periods.
Case Studies: Toxicity In Rheumatoid Arthritis Medications
Understanding the potential toxicities of rheumatoid arthritis (RA) medications requires examining real-world examples. Case studies offer invaluable insights into the clinical presentation, management strategies, and ultimately, patient outcomes. These accounts highlight the importance of proactive monitoring and early intervention in mitigating adverse effects.Analyzing specific cases allows for a nuanced understanding of how different medications manifest toxicity and how healthcare professionals can adapt their approaches.
This section will detail several examples, emphasizing the clinical course and management decisions made to improve patient well-being.
Specific Cases of Methotrexate Toxicity
Methotrexate, a commonly prescribed RA medication, can lead to various toxicities. Understanding these potential side effects is crucial for effective management. A key aspect is recognizing early signs of toxicity and promptly adjusting treatment.
Dealing with the potential toxicity of rheumatoid arthritis medications can be tough, especially when you’re already battling the disease. It’s a long, arduous journey, much like the road back for Randy Travis after his health struggles, as detailed in randy travis long road back. Finding the right balance between managing symptoms and minimizing side effects is crucial, and it requires careful monitoring and open communication with your doctor.
Ultimately, the goal remains the same: to effectively manage the arthritis while minimizing any potential toxicity from the medication.
- Case 1: A 50-year-old female with RA experienced severe nausea, vomiting, and diarrhea following a dose increase of methotrexate. The symptoms were attributed to gastrointestinal toxicity. The physician reduced the dose and administered supportive care, including antiemetics and intravenous fluids. The patient’s symptoms resolved within a week, and the methotrexate dosage was gradually increased to a tolerable level.
- Case 2: A 65-year-old male with RA on long-term methotrexate therapy developed severe liver enzyme elevations. The elevated liver function tests (LFTs) prompted a reduction in methotrexate dosage and the addition of folic acid. Liver function tests were monitored closely, and the patient’s condition improved significantly. The physician carefully monitored the patient, ensuring that the benefits of methotrexate treatment outweighed the potential risks.
This approach emphasizes the importance of regular monitoring for patients on long-term methotrexate therapy.
Clinical Course and Outcomes Comparison
The following table summarizes the clinical courses and outcomes of the presented cases, highlighting the importance of early intervention and management strategies.
Ugh, rheumatoid arthritis medications can be tricky. The potential toxicity is a real concern, especially when you’re trying to figure out the best way to manage your symptoms. Sometimes, I wonder if there’s a perfect time to be sick, like what is the best time of day to be sick , but realistically, it’s all about finding the right balance for your body.
Navigating the side effects of these medications takes careful consideration, and it’s not always easy to determine the safest course of action. Ultimately, it’s essential to be in close contact with your doctor to manage the toxicity risks properly.
| Case | Clinical Presentation | Management | Outcome |
|---|---|---|---|
| Case 1 | Severe gastrointestinal distress (nausea, vomiting, diarrhea) | Dose reduction, supportive care (antiemetics, IV fluids) | Complete resolution of symptoms; successful continued methotrexate therapy with adjusted dosage |
| Case 2 | Elevated liver enzymes (LFTs) | Dose reduction, folic acid supplementation, close monitoring of LFTs | Significant improvement in liver function; successful continued methotrexate therapy with adjusted dosage |
Successful Outcomes Despite Toxicity
Recognizing that successful outcomes are possible even with toxicity requires highlighting positive patient experiences. These cases demonstrate the importance of collaboration between patients and healthcare professionals in navigating challenges.
- Patient 1: Despite experiencing mild gastrointestinal side effects, Patient 1 actively participated in managing their methotrexate regimen. Through close monitoring and adjustments to the medication schedule, the patient successfully maintained their RA treatment while minimizing adverse effects. This case illustrates the significance of patient engagement in treatment plans.
- Patient 2: Patient 2, experiencing mild liver enzyme elevation, actively cooperated with their physician. Through careful monitoring and dose adjustments, Patient 2 successfully continued methotrexate therapy while effectively managing the potential toxicity. The patient’s active role in treatment underscores the positive impact of open communication and collaboration.
Illustrative Examples of Toxicity
Navigating the complexities of rheumatoid arthritis (RA) treatment often involves balancing therapeutic benefits against potential side effects. Understanding the various manifestations of medication toxicity is crucial for both patients and healthcare providers. This section will delve into specific adverse events, explore the role of genetics, emphasize the importance of lifestyle modifications, and discuss tailored management strategies for different patient populations.
Adverse Event: Gastrointestinal Ulcers from NSAIDs
Nonsteroidal anti-inflammatory drugs (NSAIDs), commonly used in RA management, can lead to gastrointestinal (GI) ulcers. These ulcers can range from minor irritation to severe complications, impacting quality of life significantly. Symptoms may include abdominal pain, nausea, vomiting, and bleeding. Early detection is critical. Diagnosis typically involves endoscopy, a procedure where a camera is inserted into the GI tract to visualize the lining.
Management of GI Ulcers
Management of NSAID-induced GI ulcers involves a multi-faceted approach. Firstly, reducing NSAID dosage or switching to a different medication can significantly lessen the risk. Proton pump inhibitors (PPIs) are frequently prescribed to suppress stomach acid production, thus protecting the GI lining. Lifestyle modifications, such as adopting a balanced diet rich in fiber and avoiding excessive alcohol consumption, can also contribute to healing.
Regular follow-up appointments with a gastroenterologist are essential to monitor the ulcer’s progression and ensure adequate healing.
Role of Genetics in Medication Toxicity
Genetic variations can significantly influence how individuals metabolize medications. Certain genes play a critical role in drug metabolism, affecting the rate at which medications are broken down and eliminated from the body. Variations in these genes can lead to either increased or decreased drug levels, potentially increasing the risk of toxicity. For example, individuals with specific polymorphisms in cytochrome P450 enzymes may experience higher levels of certain RA medications, increasing the chance of adverse effects.
Pharmacogenomics, the study of how genes affect a person’s response to drugs, is increasingly utilized to personalize medication regimens and minimize toxicity.
Lifestyle Modifications for Managing Side Effects
Adopting healthy lifestyle choices can play a vital role in mitigating the impact of RA medications on overall well-being. A balanced diet rich in fruits, vegetables, and whole grains provides essential nutrients to support the body’s healing processes. Regular exercise, tailored to individual capabilities, can improve joint function, reduce inflammation, and boost mood. Adequate sleep is crucial for overall health and well-being.
Stress management techniques, such as meditation or yoga, can help minimize the body’s inflammatory response.
Managing Toxicity in Specific Patient Populations
Different patient populations require tailored approaches to managing medication toxicity. Elderly patients, for example, often have reduced organ function, impacting drug metabolism and excretion. Lower doses of medication may be necessary to prevent toxicity. Patients with kidney or liver disease also require careful monitoring of medication levels to avoid adverse effects. Similarly, pregnant or breastfeeding women require specialized consideration of drug safety, as certain medications can pass through the placenta or breast milk.
Case Study: Methotrexate-Induced Hepatotoxicity
A 55-year-old female with RA was prescribed methotrexate for disease management. Over time, she experienced elevated liver enzymes, a hallmark of hepatotoxicity. The dosage of methotrexate was gradually reduced, and folic acid supplementation was initiated to mitigate the toxicity. Regular liver function tests were performed to monitor liver health. In this case, close monitoring and a prompt response to elevated liver enzymes were crucial in preventing further complications.
This case underscores the importance of routine monitoring for patients on methotrexate and other medications known to have hepatotoxic potential.
End of Discussion
In conclusion, managing toxicity in rheumatoid arthritis medications necessitates a multi-faceted approach. By thoroughly understanding the various types of medications, potential side effects, monitoring strategies, and patient education, healthcare professionals and patients can work collaboratively to optimize treatment outcomes and ensure the best possible quality of life. Future research and innovative therapies will further refine our approach to this complex issue.
