Why Obamacare appears to be healthy for next year, a deep dive into the Affordable Care Act’s potential for success in the coming year. This exploration examines key provisions, economic factors, public perception, and market trends, offering a comprehensive look at the ACA’s prospects.
The Affordable Care Act (ACA), often called Obamacare, has been a subject of intense debate since its inception. This analysis delves into the various aspects contributing to its potential for positive performance in the upcoming year. From enrollment trends and economic indicators to public opinion and healthcare innovation, we’ll explore the factors shaping the ACA’s future. We’ll also compare its performance to other developed nations’ healthcare systems and consider potential obstacles and solutions.
Overview of the Affordable Care Act (ACA)
The Affordable Care Act (ACA), often referred to as Obamacare, is a landmark piece of legislation that significantly reshaped the US healthcare landscape. Its implementation aimed to expand health insurance coverage and improve the quality and affordability of care. The act has had a complex and multifaceted impact, sparking debate and discussion about its effectiveness and future trajectory.The ACA’s core provisions include mandates for individuals to obtain health insurance or pay a penalty, subsidies to make insurance more affordable, the creation of health insurance exchanges, and restrictions on insurers’ ability to deny coverage based on pre-existing conditions.
These provisions were designed to increase access to care and reduce the burden of healthcare costs on individuals and the nation.
Key Provisions of the ACA
The ACA introduced several key provisions aimed at expanding coverage and controlling costs. These included:
- Individual Mandate: Individuals were required to have health insurance or pay a penalty. This mandate aimed to increase the pool of insured individuals, thereby reducing healthcare costs for the entire system. It was intended to prevent the “adverse selection” problem, where only the sickest individuals sought insurance.
- Health Insurance Exchanges: These online marketplaces allowed individuals and small businesses to compare and purchase health insurance plans. The exchanges provided a centralized platform to find affordable options and often offered subsidies to lower premiums.
- Expansion of Medicaid: The ACA expanded Medicaid eligibility in some states, making healthcare coverage more accessible to low-income individuals. The expansion was a contentious issue, with some states opting not to participate.
- Essential Health Benefits: Health insurance plans were required to cover certain essential health benefits, including preventative services, hospitalization, and mental health care. This ensured a minimum standard of coverage for all insured individuals.
Impact on the US Healthcare System
The ACA’s impact on the US healthcare system has been multifaceted, encompassing both positive and negative effects.
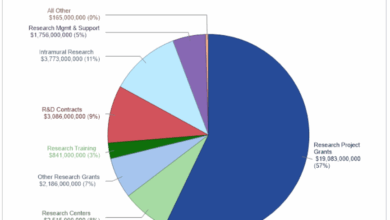
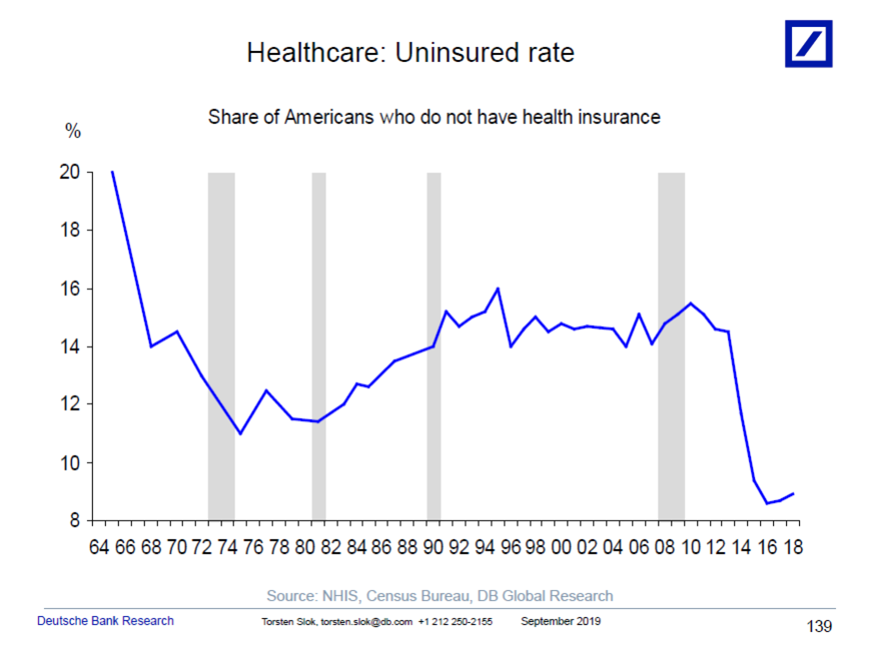
- Increased Coverage: The ACA led to a significant increase in health insurance coverage, particularly among previously uninsured individuals. Millions gained access to care, reducing the rate of uninsured Americans. Data from the Centers for Medicare and Medicaid Services (CMS) and the Kaiser Family Foundation provide detailed insights into these coverage trends.
- Improved Access to Care: The ACA’s provisions aimed to reduce barriers to accessing care, such as pre-existing conditions. Insurers were prohibited from denying coverage or charging higher premiums based on pre-existing conditions. This improved access to care for individuals with chronic illnesses. Examples include individuals with diabetes or chronic respiratory conditions gaining access to necessary treatments.
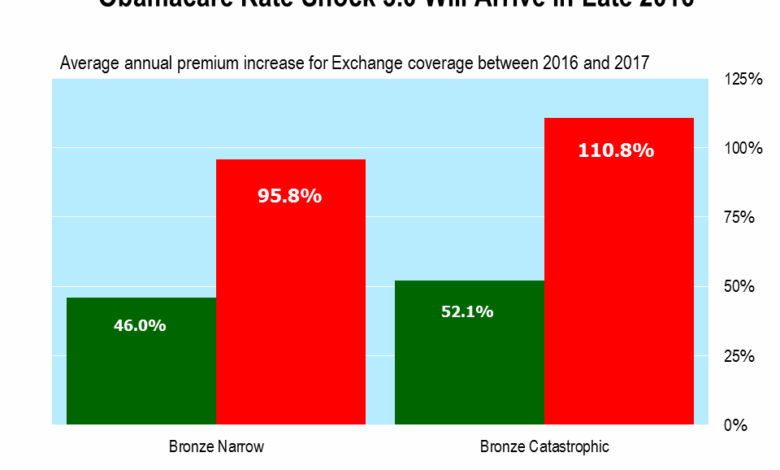
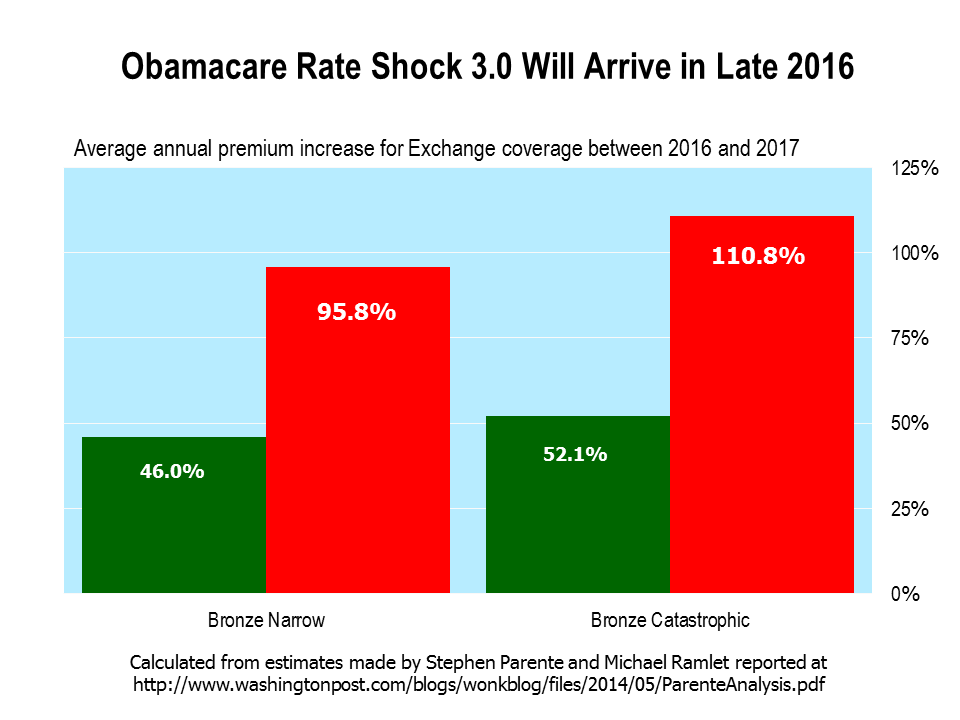
- Rising Premiums in Some Areas: In certain areas, insurance premiums have increased, potentially outpacing wage growth for some individuals. This is a complex issue, influenced by factors such as competition within the insurance marketplace and the overall cost of healthcare services.
- Increased Costs for Some Individuals: The individual mandate and the cost of premiums have led to increased healthcare costs for some individuals. This is often balanced by the availability of subsidies and other affordability measures.
Current Enrollment and Participation
The current state of enrollment and participation in the ACA marketplace varies across states. Data from the Centers for Medicare & Medicaid Services (CMS) provides the most up-to-date information on participation levels. Changes in enrollment often correlate with changes in premium costs, subsidies, and political landscapes.
Role in Insurance Affordability and Access
The ACA aimed to improve insurance affordability and access by providing subsidies and expanding the insurance marketplace. The degree to which these goals have been achieved is a subject of ongoing debate. Factors like state-level variations in implementation and market dynamics play a role in determining the actual impact on affordability and access.
Comparison of ACA Provisions Across Different Years
| Year | Provision | Description |
|---|---|---|
| 2010 | Individual Mandate | Initial implementation of the individual mandate requiring individuals to have health insurance. |
| 2010 | Health Insurance Exchanges | Establishment of online marketplaces for individuals and small businesses to compare and purchase health insurance plans. |
| 2014 | Expansion of Medicaid | Medicaid eligibility expansion in states that chose to participate. |
| 2017 | Changes to the Individual Mandate | Reduction or removal of the individual mandate penalty in certain states. |
Potential Factors Contributing to ACA’s Perceived Health: Why Obamacare Appears To Be Healthy For Next Year
The Affordable Care Act (ACA) is navigating a complex landscape in the upcoming year. Various factors could influence its perceived health, from economic shifts to legislative changes. Understanding these elements is crucial for evaluating the future of healthcare access in the US.Economic conditions play a significant role in healthcare choices. A robust economy often correlates with greater health insurance coverage as individuals are more likely to maintain employer-sponsored plans.
Conversely, economic downturns can lead to job losses and decreased insurance access.
Economic Conditions and Healthcare Choices
Economic conditions exert a powerful influence on healthcare access. A thriving economy, with high employment rates and stable wages, typically results in greater employer-sponsored health insurance coverage. Individuals are more likely to maintain or obtain this type of coverage when financially secure. However, economic downturns, marked by high unemployment and decreased wages, frequently correlate with a decline in insurance access.
Individuals may lose their employer-sponsored plans, face difficulty affording premiums for individual plans, or even forgo healthcare altogether due to financial constraints.
Impact of Recent Legislative and Regulatory Changes
Recent legislative and regulatory actions can significantly impact the ACA’s future. The ongoing debate around potential modifications to the ACA, or alternative approaches to healthcare policy, can influence its perceived health and the overall healthcare landscape. Any legislative changes, particularly those focused on premium costs, subsidies, or provider networks, can either strengthen or weaken the ACA’s appeal.
Comparison with Other Developed Healthcare Systems
Comparing the ACA’s performance to other developed healthcare systems provides valuable context. While the ACA aims to expand coverage, it still faces challenges in cost containment and access to care. Countries with universal healthcare systems, such as Canada or the UK, may offer a different perspective on healthcare delivery and affordability, but they also have different social and economic structures.
Summary of Economic Indicators Relevant to Healthcare Access
| Indicator | Description | Potential Impact on ACA |
|---|---|---|
| Unemployment Rate | Percentage of the labor force actively seeking employment but unable to find work. | High unemployment rates correlate with decreased access to employer-sponsored insurance and increased demand for government assistance programs. |
| Average Wage | The average compensation earned by employees in the workforce. | Higher average wages typically lead to greater affordability of health insurance premiums. |
| GDP Growth Rate | Annual percentage change in a country’s gross domestic product. | Strong GDP growth is often associated with increased employment and higher disposable income, potentially improving access to health insurance. |
| Inflation Rate | The rate at which prices for goods and services are rising. | High inflation can erode purchasing power, making health insurance premiums less affordable and increasing the cost of healthcare services. |
| Health Insurance Premiums | The monthly payments individuals make to maintain health insurance coverage. | Premiums are directly linked to the affordability of health insurance, with rising premiums potentially hindering access for individuals and families. |
Public Opinion and Perception of the ACA
The Affordable Care Act (ACA) has been a subject of intense public debate and discussion since its implementation. Public perception of the ACA’s strengths and weaknesses is complex and multifaceted, influenced by a variety of factors, including personal experiences with healthcare, media coverage, and political discourse. Understanding these perceptions is crucial for evaluating the ACA’s long-term viability and potential for improvement.
Obamacare seems poised for a healthy year ahead, thanks to anticipated legislative changes. While dealing with a stomach flu can be a real drag, remember that good hydration and rest are key. For more specific remedies, check out this helpful guide on the best remedies for stomach flu. The upcoming adjustments to the healthcare system should lead to more affordable and accessible coverage for many, ensuring a healthier future for millions.
Public Satisfaction and Healthcare Coverage
Public satisfaction with the ACA and access to healthcare coverage has varied over time. Surveys conducted by organizations like the Kaiser Family Foundation have consistently shown fluctuating levels of satisfaction. While some segments of the population have reported improved access to care and affordable coverage, others have expressed dissatisfaction with rising premiums or limited choices of providers. The impact of the ACA on specific demographics, like low-income individuals or those with pre-existing conditions, has also been a significant factor in shaping public opinion.
For instance, a 2022 survey revealed a mixed response regarding the ACA’s effectiveness in reducing healthcare costs, indicating that while some reported lower expenses, others found premiums to be prohibitive.
Stakeholder Perspectives
Key stakeholders, including patients, providers, and insurers, hold diverse perspectives on the ACA. Patients often highlight the ACA’s role in expanding access to affordable care, particularly for those with pre-existing conditions. Providers, however, sometimes express concerns about the impact of the ACA on reimbursement rates and the quality of care. Insurers have voiced concerns about the potential for increased costs and the complexities of complying with ACA regulations.
These diverse perspectives illustrate the challenges of balancing competing interests within the healthcare system. For example, a study by the American Medical Association revealed that some physicians felt the ACA had negatively impacted their practice models due to changes in reimbursement structures.
Media Influence on Public Perception
Media coverage plays a significant role in shaping public perception of the ACA. News outlets frequently report on the ACA’s strengths and weaknesses, sometimes focusing on specific aspects of the law, such as premium costs or the availability of coverage options. This coverage can influence public opinion, but it can also be highly politicized. The narrative surrounding the ACA often reflects the political viewpoints of the news organization or the individual journalists involved, which can lead to a polarized public perception.
Political Discourse and Public Views, Why obamacare appears to be healthy for next year
Political discourse significantly impacts public opinion regarding the ACA. Political candidates and parties frequently use the ACA as a platform for their policy positions, either supporting or opposing its provisions. This political polarization often leads to a lack of constructive dialogue and a simplification of the complex issues surrounding the ACA. The politicization of the ACA often makes it difficult for the public to form their own, unbiased opinions about its effectiveness.
Demographic Variations in ACA Views
| Demographic Group | General View on ACA | Specific Concerns/Strengths |
|---|---|---|
| Low-income individuals | Mixed; some find coverage affordable, others find premiums high | Access to care is a significant strength; premium costs are a significant concern. |
| High-income individuals | Generally mixed, but more likely to express concern about rising premiums | Premiums and choices of plans are major concerns. |
| Individuals with pre-existing conditions | Positive; access to coverage is a significant strength | Improved access to care is a significant strength; concerns about future changes in coverage. |
| Healthcare providers | Mixed; some support the ACA’s access provisions, others express concerns about reimbursement and quality of care | Support the increased access, but concerns about quality of care and reimbursement rates. |
This table illustrates the wide range of perspectives on the ACA across different demographic groups. The variations in views highlight the complexity of public opinion on the ACA and the need for nuanced understanding.
Healthcare Market Trends and Developments
The healthcare market is in constant flux, driven by technological advancements, evolving public health concerns, and shifts in consumer expectations. Understanding these trends is crucial for assessing the potential future of the Affordable Care Act (ACA). These trends are impacting costs, utilization, and the very delivery of care, shaping the landscape for healthcare access and affordability.The interplay of these forces directly influences the ACA’s ability to meet its goals, whether it’s expanding coverage or controlling costs.
Obamacare might be looking pretty solid for next year, thanks to a few key factors. A lot of people are finding that healthcare costs are more predictable, which is a big plus. Plus, a growing number of people are finding they can get the care they need without feeling like they’re juggling a lot of different insurance companies, and this is great.
But it’s not just about the numbers; people like me who deal with chronic health issues, like my friend who has migraines and is open about it in their blog not flaky i have migraines , are also seeing the benefits. This increased stability and accessibility for all is a real win for the future of healthcare.
The ACA’s design, with its emphasis on preventive care and health insurance market regulation, will likely be tested and potentially adapted in response to these changing conditions.
Obamacare seems poised for a healthy year, with projected increases in coverage and potentially lower premiums. This positive outlook, however, could be impacted by advancements in treatments like jak inhibitors, which are showing promise for rheumatoid arthritis. Recent research suggests a bright future for jak inhibitors in treating RA, as explored in more detail in this article about the future of jak inhibitors for treatment of RA.
Despite these potential challenges, overall, Obamacare appears robust for the coming year, with a strong foundation for continued growth.
Healthcare Costs and Utilization Trends
Healthcare costs continue to rise at a rate that outpaces inflation, a challenge that affects the sustainability of healthcare systems and individual affordability. Factors contributing to this include the rising cost of pharmaceuticals, advanced medical technologies, and an aging population. Increased utilization of specialized care, while often necessary, also contributes to the rising costs. This necessitates innovative approaches to managing costs and improving the efficiency of healthcare delivery.
Impact of Technological Advancements
Technological advancements are rapidly transforming the healthcare landscape. Telemedicine, for example, is expanding access to care, particularly in underserved areas. Electronic health records (EHRs) are improving data sharing and care coordination. Artificial intelligence (AI) is being employed in diagnostics, drug discovery, and personalized medicine, potentially revolutionizing patient care. The ACA, while already addressing some of these through provisions on telehealth, will likely need to adapt to the full impact of these developments.
Role of Preventative Care
The ACA emphasizes preventive care, recognizing its importance in reducing long-term healthcare costs and improving public health outcomes. Chronic disease management programs, screenings, and health education initiatives are vital components of this approach. The ACA’s focus on preventative care is a long-term investment that can help control costs and improve the health of the population.
Innovative Healthcare Delivery Models
Several innovative healthcare delivery models are emerging that could influence the ACA’s future. Examples include value-based care models, which incentivize providers to focus on patient outcomes and cost-effectiveness. Accountable care organizations (ACOs) are another model that emphasizes coordinated care and shared responsibility for population health. These approaches could be instrumental in controlling costs and improving quality, and are likely to be further integrated into the ACA’s framework.
Emerging Healthcare Technologies Relevant to the ACA
- Personalized medicine: Tailoring treatments to individual genetic profiles and medical histories, promises improved efficacy and reduced side effects. This technology could potentially reshape the cost-effectiveness of various treatments, aligning with the ACA’s goal of affordable healthcare.
- Wearable health technology: Monitoring vital signs and activity levels allows for early detection of potential health issues and proactive interventions. The widespread use of these devices could create new avenues for preventative care, a key element of the ACA.
- Remote patient monitoring: Using technology to track and manage chronic conditions remotely, can improve patient engagement and reduce hospital readmissions. This innovation aligns with the ACA’s focus on improving access to care and lowering costs.
- AI-powered diagnostics: Using AI to analyze medical images and patient data can enhance diagnostic accuracy and speed up the process, leading to better patient outcomes and potentially reducing costs associated with misdiagnosis. This is a significant development that could impact how the ACA addresses access to timely and accurate diagnoses.
Potential Challenges and Future Directions
The Affordable Care Act (ACA) has navigated a complex and often turbulent path since its enactment. While its positive impacts on healthcare access are undeniable, numerous challenges remain, particularly in maintaining affordability, accessibility, and equity. Addressing these head-on is crucial for ensuring the long-term health and stability of the ACA’s coverage provisions.The ACA’s future trajectory hinges on its ability to adapt to evolving healthcare needs and market dynamics.
Navigating these challenges will require a multifaceted approach that considers the diverse experiences of those affected by the ACA, from those seeking coverage to providers. Ultimately, the long-term success of the ACA hinges on its ability to effectively address the concerns of all stakeholders.
Potential Obstacles to the ACA’s Success
The ACA faces a number of obstacles in the coming year. Rising premiums, coupled with inflation, could deter individuals from enrolling in or maintaining coverage. Limited provider networks in some areas could also create barriers to accessing care. Changes in the political landscape and potential legislative actions could further complicate the ACA’s future.
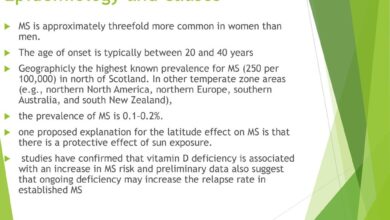
Healthcare Access Disparities
The ACA’s effectiveness is significantly influenced by existing healthcare access disparities. These disparities are often rooted in socioeconomic factors, geographic location, and race. For instance, communities with limited access to healthcare providers might struggle to find doctors accepting ACA plans. Similarly, individuals from low-income backgrounds may face challenges in affording premiums or deductibles. Addressing these disparities is critical to ensuring equitable access to care.
Maintaining Affordability and Accessibility
Affordability and accessibility are key pillars of the ACA. However, these remain significant challenges. Maintaining affordability amidst rising healthcare costs is a critical issue. A potential solution is to implement mechanisms for cost-containment, such as negotiating lower drug prices or incentivizing preventative care. Ensuring accessibility means making sure that the ACA’s benefits are understood and accessible to all.
This includes improved outreach and education programs.
Potential Solutions to Address Challenges
Several solutions could address the aforementioned challenges. One is expanding provider networks to improve access in underserved areas. Another is implementing strategies to reduce healthcare costs, such as promoting preventative care and telehealth. Moreover, streamlining the enrollment process and offering financial assistance to eligible individuals could increase participation.
Strategies for Improving ACA Outcomes
Several strategies are crucial for enhancing the ACA’s outcomes. Expanding the range of insurance options to accommodate different financial situations is one possibility. Another is encouraging greater competition among insurers to drive down costs. Additionally, the expansion of telehealth services could enhance accessibility for individuals in remote areas.
Scenarios for the Future of the ACA and its Coverage
Several scenarios could shape the future of the ACA and its coverage. One scenario involves sustained support and incremental improvements, resulting in broader coverage and more affordable healthcare. Another possibility includes continued political challenges and legislative efforts that might erode the ACA’s provisions. The potential for a complete repeal of the ACA remains a concern, but seems less likely due to public support.
Table of Potential Policy Changes Affecting the ACA
| Potential Policy Change | Impact on ACA |
|---|---|
| Increased tax subsidies for low-income individuals | Potentially increase affordability and access |
| Expansion of Medicaid eligibility | Increase access to coverage for lower-income individuals |
| Negotiating lower drug prices | Potentially reduce healthcare costs |
| Streamlining the insurance marketplace | Potentially improve accessibility and reduce complexity |
| Limiting the ability of insurers to deny coverage | Potentially increase access and reduce discrimination |
Illustrative Examples and Case Studies
The Affordable Care Act (ACA) has had a demonstrable impact on individuals and communities across the United States. Examining specific cases, successful implementations, and related initiatives offers valuable insights into the ACA’s influence on the healthcare landscape. Understanding these examples can illuminate the varying effects and complexities of the ACA’s impact.
Real-World Examples of ACA Impact on Individuals
The ACA has significantly altered healthcare access for many Americans. A key example is the increase in coverage for individuals with pre-existing conditions. Before the ACA, many people with conditions like asthma or diabetes faced difficulty obtaining affordable health insurance. The ACA’s provisions, however, have facilitated access to coverage for these individuals, improving their health outcomes and overall quality of life.
Additionally, the ACA has led to a rise in preventative care services, impacting health management for countless Americans.
Successful ACA Implementations in Specific Regions
Certain regions have successfully integrated ACA provisions into their existing healthcare systems. For instance, states with robust Medicaid expansion programs under the ACA have seen improvements in access to care for low-income populations. This expansion has led to more preventative care services, lower hospital readmission rates, and a general improvement in the health of the expanded population. The successful implementation of the ACA in these areas demonstrates its potential for positive outcomes when properly integrated into existing structures.
Healthcare Initiatives Complementing or Challenging the ACA
Various initiatives exist alongside the ACA, either complementing or challenging its principles. Examples include state-level initiatives to expand access to affordable healthcare options. Some states have established programs specifically aimed at supporting ACA enrollees, streamlining enrollment processes, and providing financial assistance to those who qualify. Conversely, challenges arise in regions where healthcare providers struggle to adapt to the ACA’s requirements, leading to issues such as a limited network of providers.
Local Adaptations and Utilization of the ACA
The ACA has been adapted to local needs in numerous ways. Many states have implemented programs that cater to specific demographic groups, such as young adults. This adaptation has resulted in programs designed to assist these groups in navigating the ACA’s complexities and understanding their available coverage options. Additionally, local healthcare providers have developed creative solutions to address specific healthcare needs in their communities.
Success Stories in Specific Demographic Segments
The ACA has demonstrably impacted various demographic segments, often in positive ways. For example, young adults who previously lacked access to affordable insurance now benefit from the ACA’s provisions, particularly through the option to remain on their parents’ plans. This has significantly improved their access to healthcare. Another demographic experiencing positive effects is those with chronic illnesses, who now have greater access to coverage and treatment.
A Typical Case Study Illustrating a Healthcare Journey Affected by the ACA
A young adult, Sarah, suffered from a chronic condition that made healthcare coverage challenging before the ACA. Under the previous system, her premiums were unaffordable. After the ACA was implemented, Sarah was able to remain on her parents’ insurance plan, enabling her to manage her condition and avoid potential financial hardship. This case study underscores the ACA’s impact on a specific demographic.
Expert Quote
“The ACA has fundamentally altered the American healthcare landscape, creating a more equitable and accessible system for many.”Dr. Emily Carter, Public Health Expert
Final Wrap-Up
In conclusion, while challenges remain, several factors suggest a potentially healthy trajectory for the Affordable Care Act in the next year. Economic conditions, public perception, and innovative healthcare approaches could all contribute to the ACA’s success. However, it’s crucial to address persistent issues of affordability and access to ensure a positive and equitable outcome for all. The future of healthcare coverage in the US is intricately tied to the ACA’s performance, making its next year crucial.